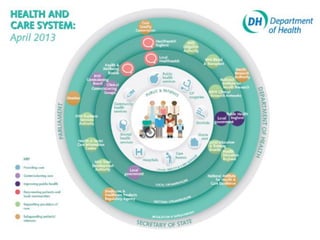
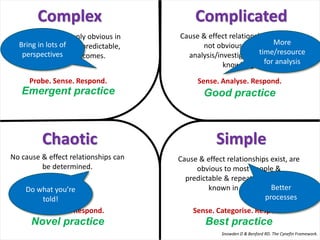
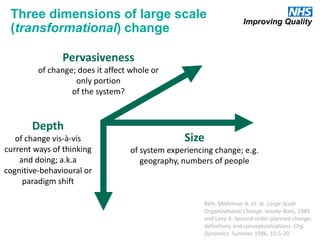
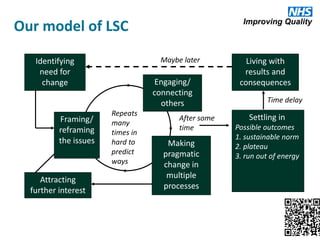
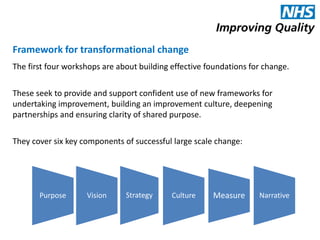
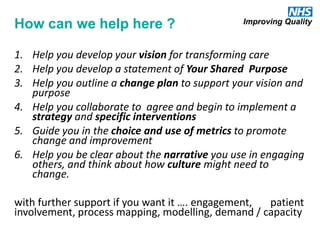
The document discusses strategies for transforming care through enhanced capabilities of Clinical Commissioning Groups (CCGs) in the NHS, highlighting challenges and a framework for large-scale change. It emphasizes the importance of commitment to change, the role of shared purpose, and the necessity of developing a clear vision and metrics for improvement. Additionally, the text outlines key components for successful change and identifies specific areas such as urgent care and mental health as significant challenges for CCGs.