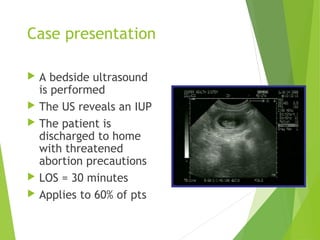
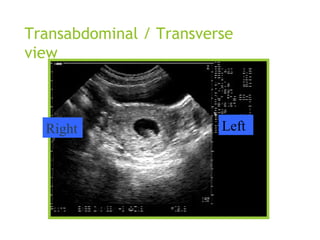
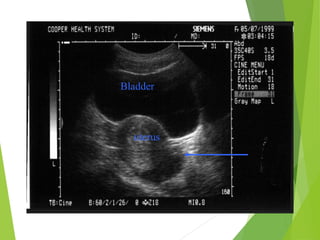
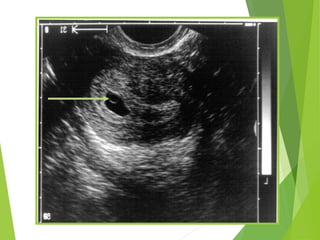
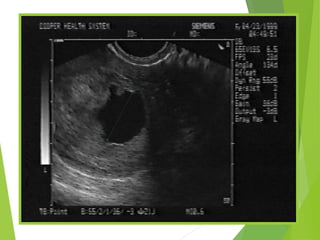
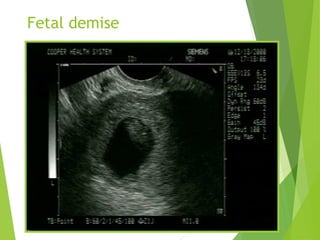
This document discusses sonographic imaging of the female pelvis for patients presenting with pelvic pain or bleeding. It begins with a case presentation of a 24-year-old female with a missed period and abdominal pain. A bedside ultrasound revealed an intrauterine pregnancy (IUP). The role of bedside sonography is to identify an IUP, establish viability, and identify sources of pelvic pain. Transabdominal and endovaginal ultrasound protocols are described. Key anatomy including the uterus, ovaries, and gestational sac are outlined. Imaging findings for normal and abnormal pregnancies as well as ectopic pregnancies are also summarized.