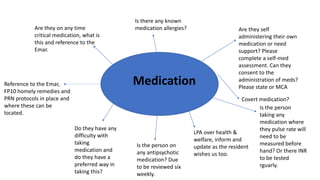
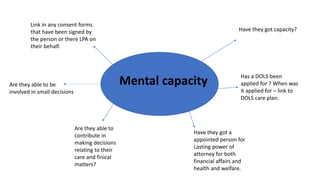
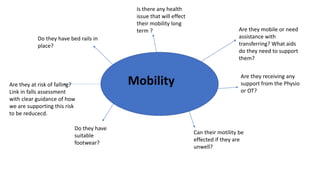
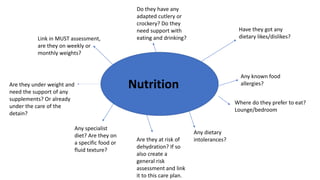
This document contains prompts for creating care plans related to communication, continence, daily life/lifestyle, death and dying, emotional support, finance, maintaining a safe environment, medical, medication, mental capacity, mobility, nutrition, personal care, sexuality, and skin integrity. For each topic, it lists relevant assessments and prompts questions about the person's needs, preferences, abilities, diagnoses, and support systems. The goal is to develop individualized care plans based on a holistic understanding of the person's situation.