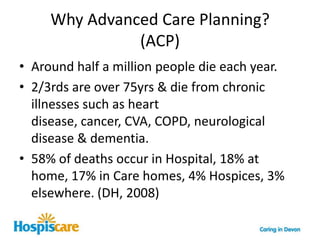
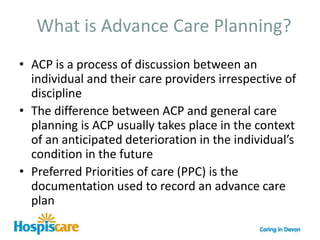
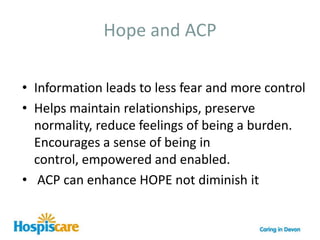
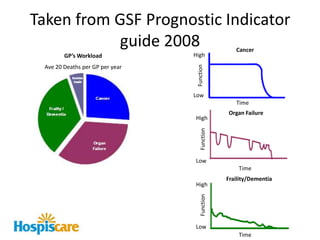
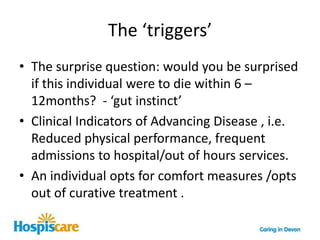
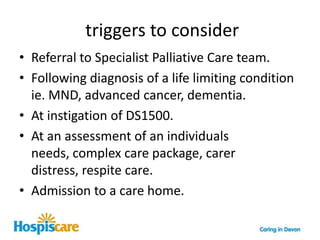
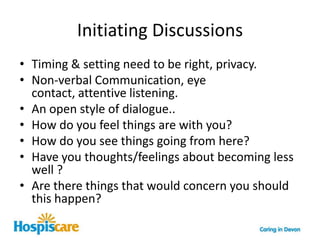
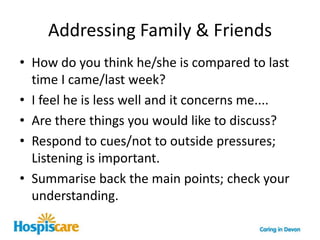
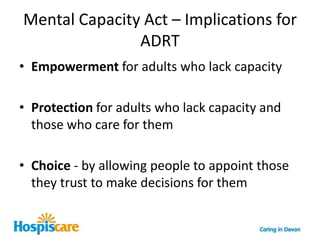
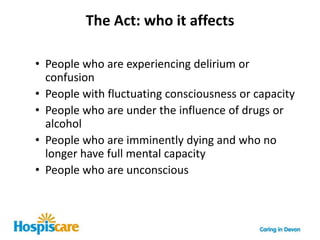
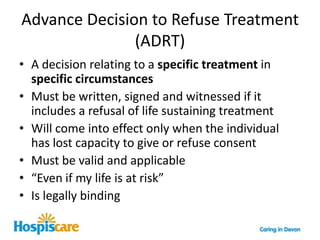
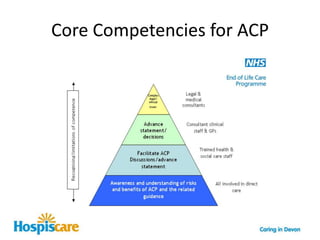
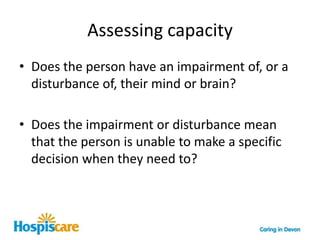
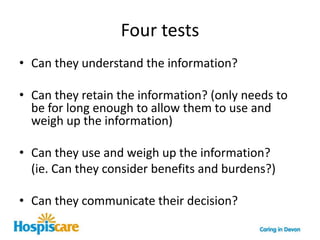
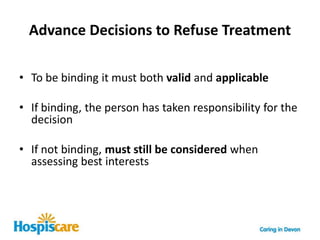
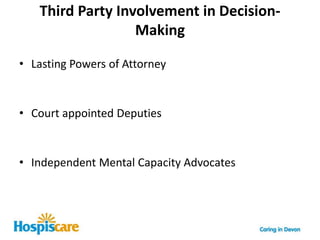
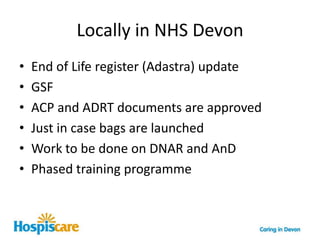
The document outlines advanced care planning (ACP) in the context of community palliative care, emphasizing its importance for individuals nearing end-of-life, particularly in aligning their care preferences and enhancing their autonomy. It highlights statistics on death locations and discusses the necessity for effective communication between healthcare providers and patients regarding end-of-life wishes, utilizing tools like the Preferred Priorities of Care (PPC) document. The piece also touches on the legal implications of Advance Decisions to Refuse Treatment (ADRT) and the need for improved understanding and documentation in various care settings.