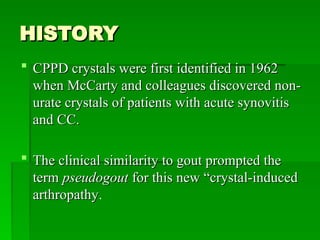
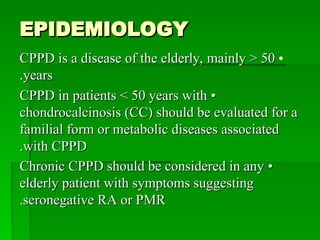
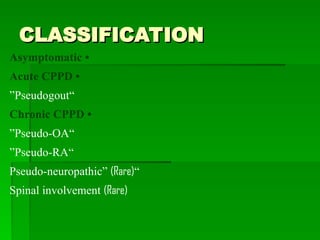
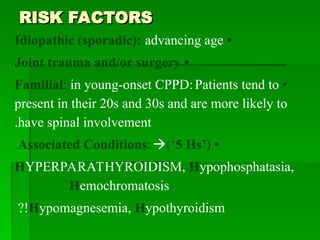
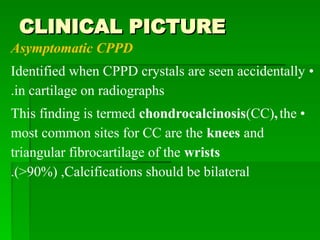
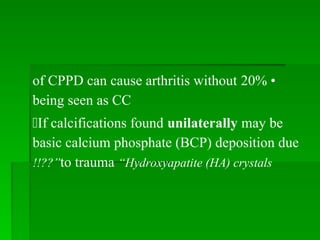
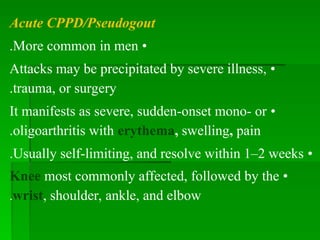
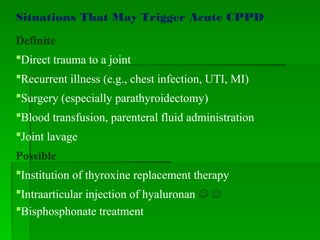
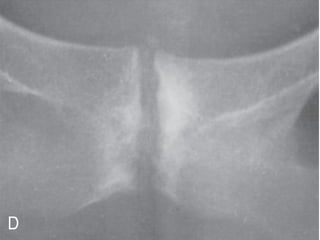
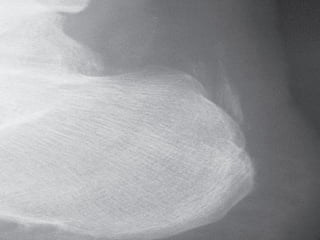
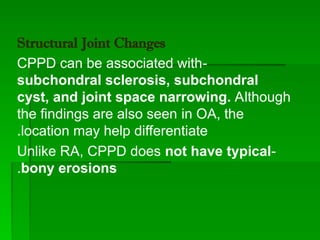
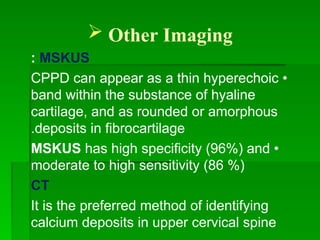
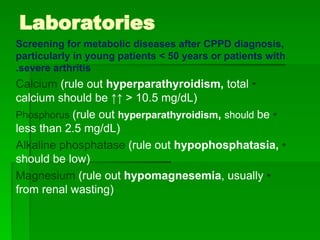
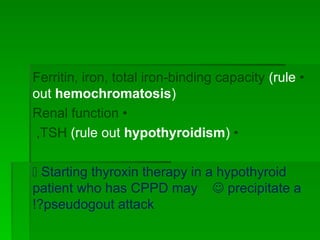
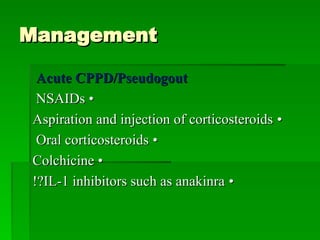
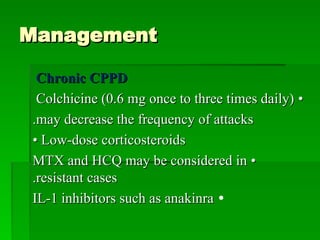
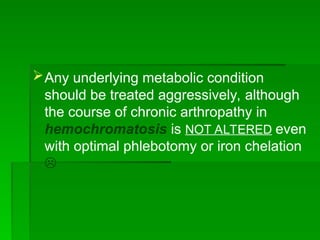
CPPD (calcium pyrophosphate dihydrate) crystals were first identified in 1962, leading to the term pseudogout for this crystal-induced arthropathy primarily affecting the elderly. The disease may manifest as asymptomatic, acute attacks, or chronic conditions like pseudo-osteoarthritis or pseudo-rheumatoid arthritis, with management options including NSAIDs and corticosteroids. Diagnosis is achieved through synovial fluid analysis and imaging, and treatment of any underlying metabolic conditions is crucial.