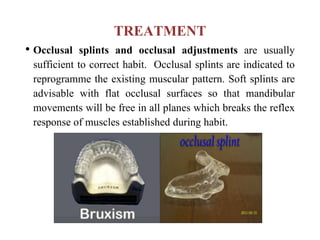
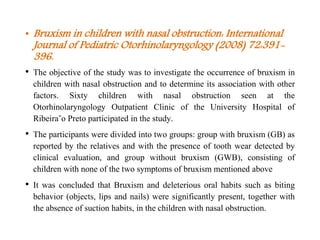
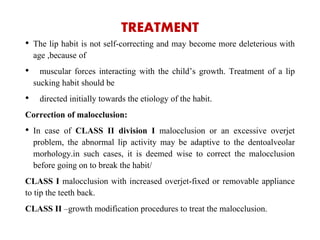
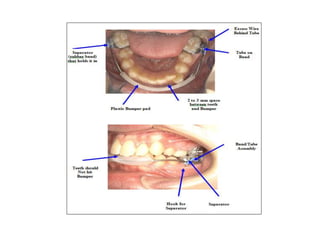
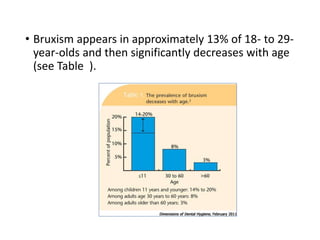
Bruxism refers to the involuntary, excessive grinding or clenching of teeth. It can occur during waking hours or sleep. The document discusses the various definitions, types, prevalence, etiology, diagnosis, and treatment of bruxism. Bruxism is a multifactorial condition influenced by morphological, pathophysiological, respiratory, and psychological factors. It is most common in children under 11 years of age. Treatment involves the use of occlusal splints and addressing any underlying causes like stress, sleep disorders, malocclusion, or respiratory conditions.

![Bruxism and Sleep
• Pathophysiological factors are believed to play a role in the
precipitation of bruxism. In younger children, bruxism may be
due to the immaturity of the masticatory neuromuscular system.
• Current thinking is that bruxism is part of an arousal response.
An arousal response is a sudden change in the depth of sleep
during which a person either arrives at a stage of lighter sleep or
wakes up. In young adults, more than 80% of sleep bruxism
episodes occur during sleep stages 1 and 2 of nonREM (light
sleep stages), and 5% to 10% in REM (deep stages). Many
bruxism episodes lead to a shift in sleep stage, usually toward
awakening or lighter sleep.[Bruxism physiology and pathology: an
overview for clinicians. J Oral Rehabil. 2008;35:476-494.]](https://image.slidesharecdn.com/newmicrosoftpowerpointpresentation2-150920085203-lva1-app6892/85/BRUXISM-13-320.jpg)