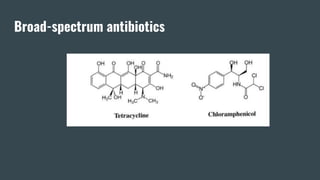
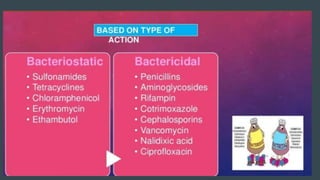
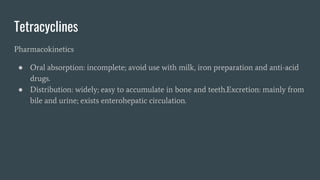
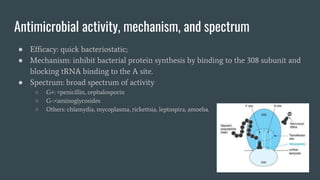
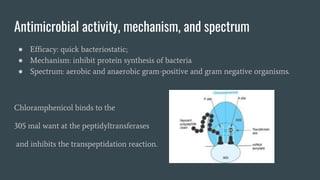
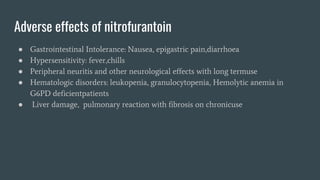
This document discusses several broad-spectrum antibiotics and their uses, including tetracyclines, chloramphenicols, and nitrofurantoin. It provides information on the pharmacokinetics, antimicrobial activity and mechanisms, therapeutic uses, and adverse reactions of each antibiotic. Tetracyclines are described as having a broad spectrum of activity against gram-positive and gram-negative bacteria via inhibiting protein synthesis. Chloramphenicols also inhibit protein synthesis but are rarely used due to toxicity risks like bone marrow suppression. Nitrofurantoin is primarily used for urinary tract infections as it is not absorbed systemically and concentrates in the urine.
![• Gram Negative Organisms
●Cocci:--[Neisseria meningitidis]
[Neisseria Gonococci ]
●Bacilli:-- E.Coli
Salmonella
Shigella
Klebsiella](https://image.slidesharecdn.com/rollno136-150-230309100540-719d2f7f/85/Broad-spectrum-antibiotics-2-320.jpg)