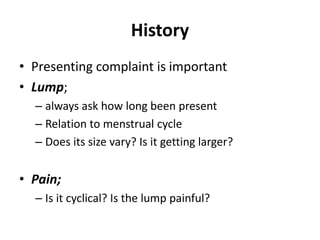
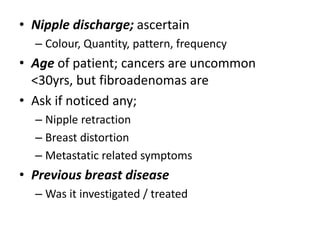
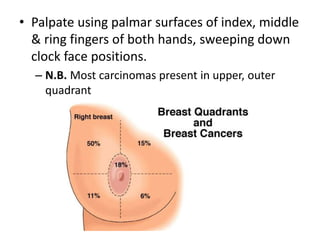
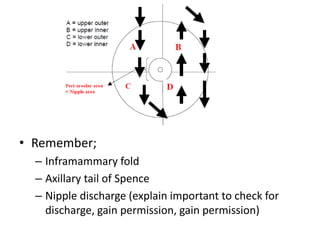
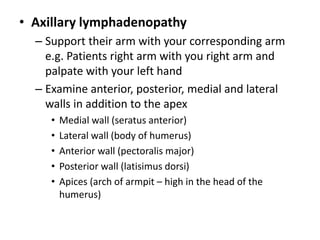
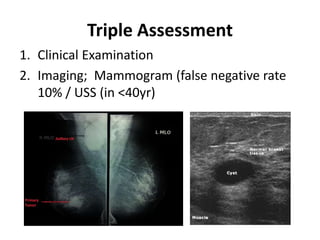
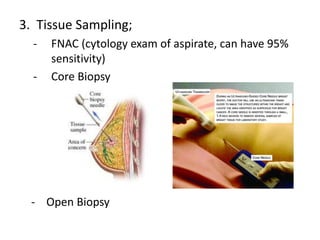
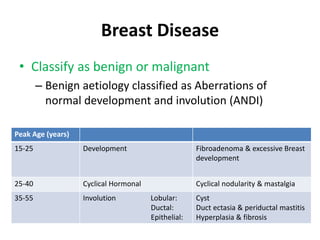
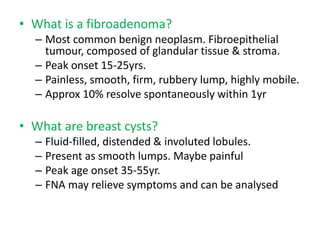
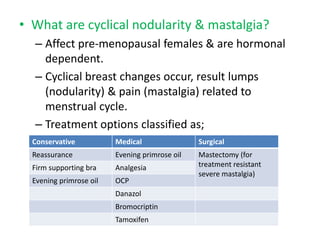
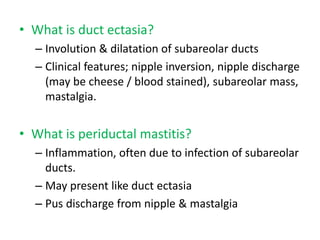
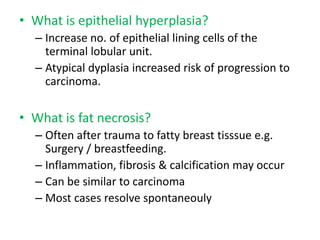
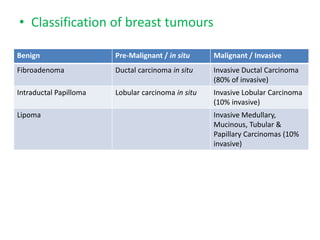
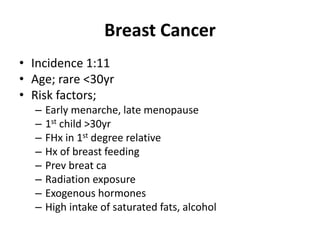
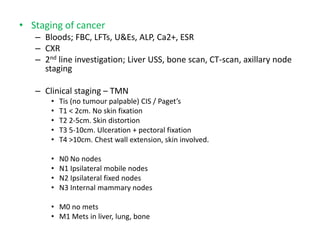
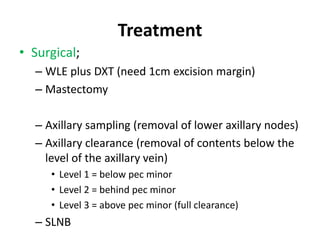
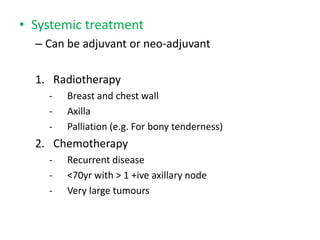
This document provides information about breast examination techniques and breast conditions. It discusses taking a history, performing a physical exam including inspection and palpation of the breasts and lymph nodes, and triple assessment with imaging and tissue sampling. Common benign breast conditions like fibroadenomas and cysts are explained. Breast cancer risk factors, staging, and treatment options including surgery, radiation, chemotherapy, and endocrine therapy are outlined.