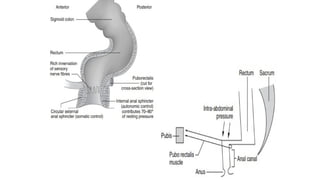
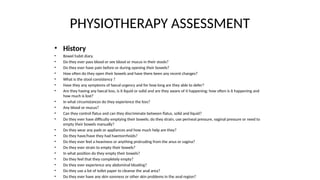
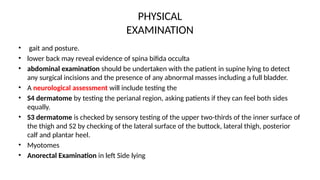
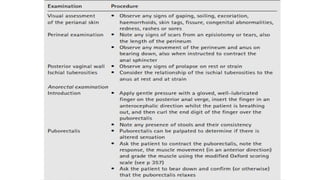
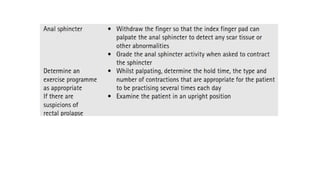
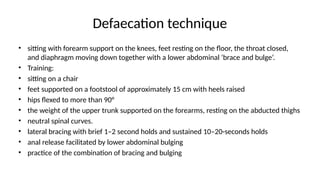
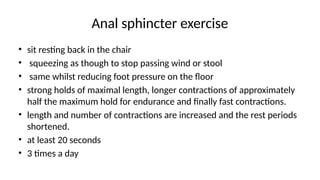
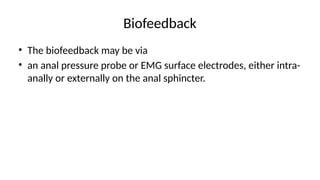
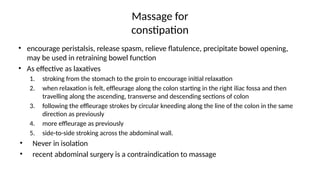
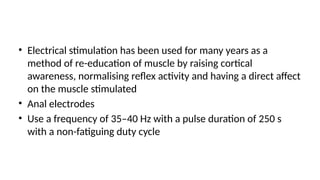
The document discusses bowel and anorectal dysfunction, outlining various conditions related to difficulty in defecation and factors contributing to constipation and anal incontinence. It details symptoms, diagnostic considerations, and treatment approaches, including diet, bowel retraining, and the use of biofeedback. Additionally, it highlights the importance of understanding the physiological mechanisms involved in bowel function and the impact of psychological and environmental factors on these disorders.