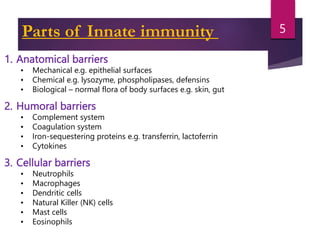
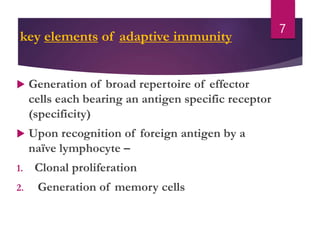
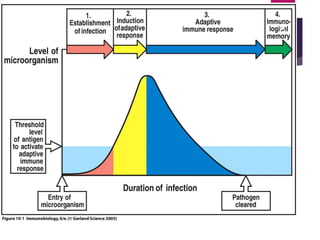
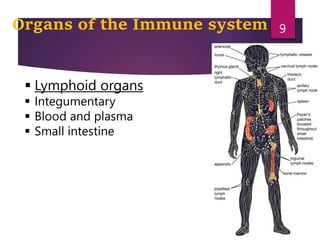
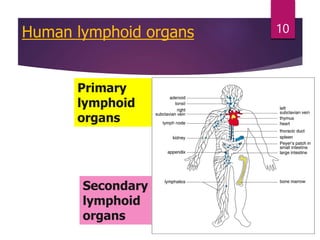
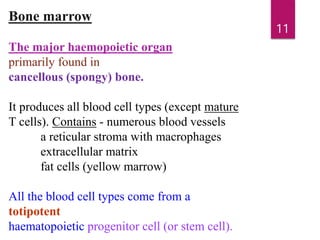
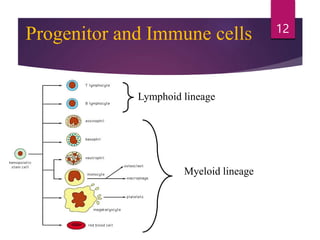
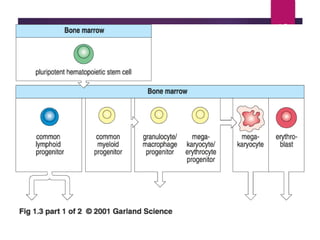
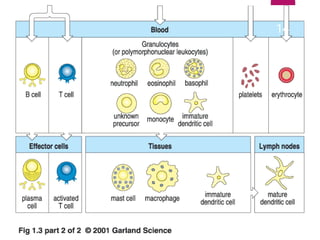
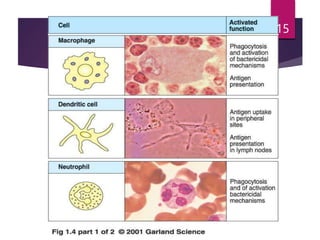
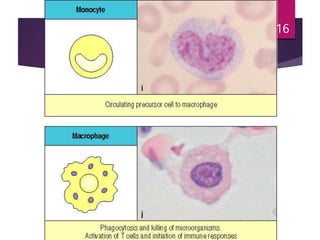
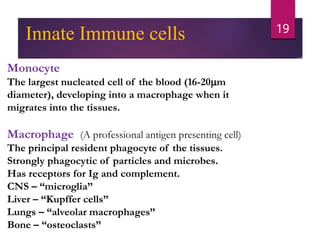
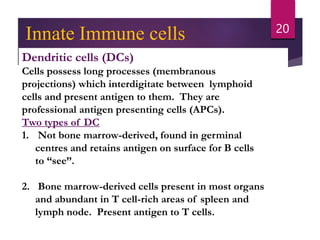
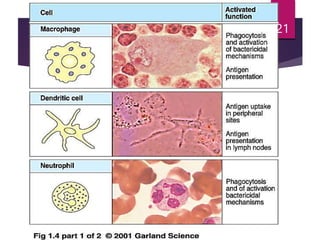
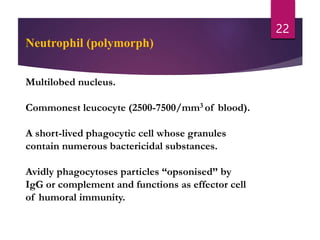
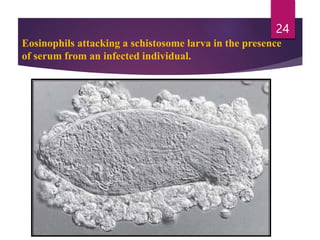
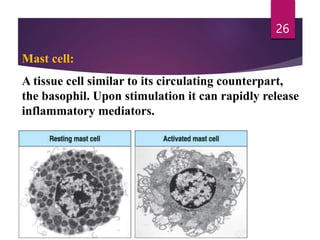
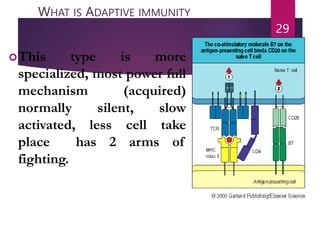
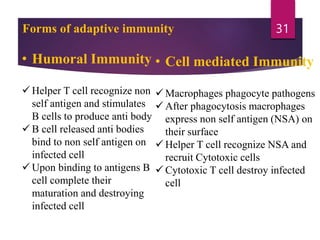
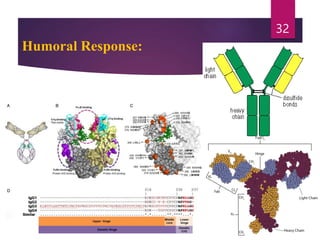
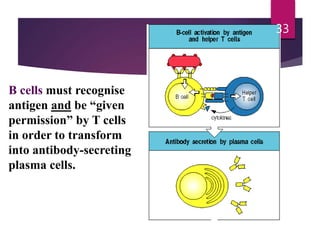
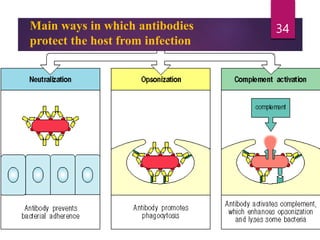
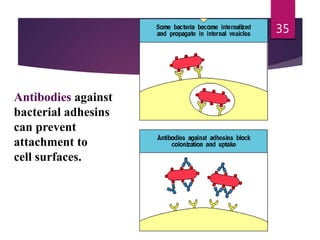
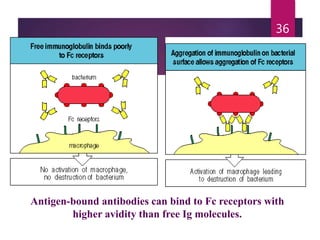
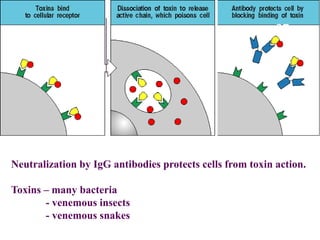
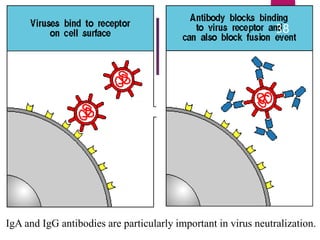
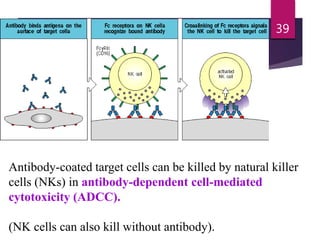
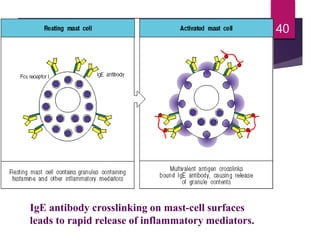
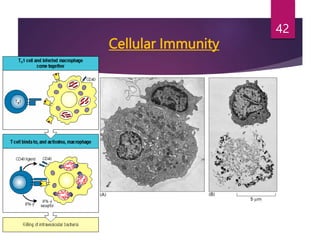
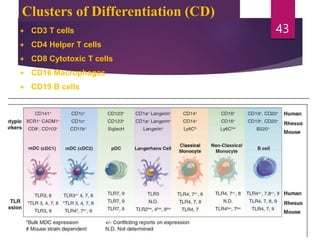
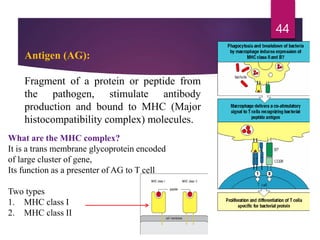
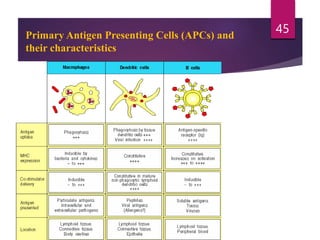
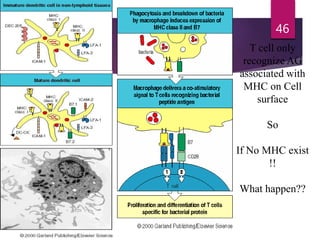
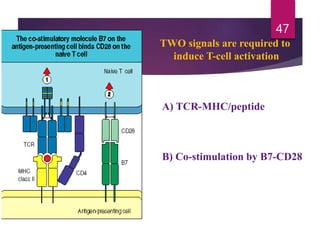
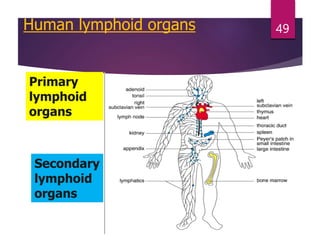
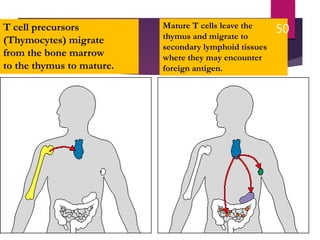
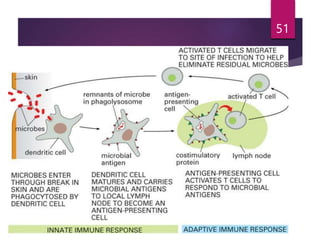
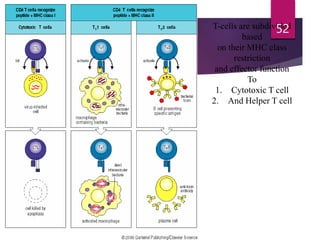
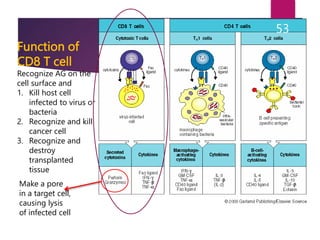
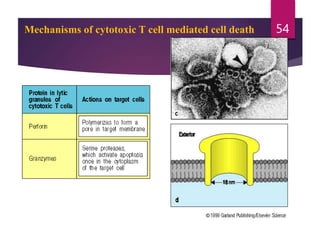
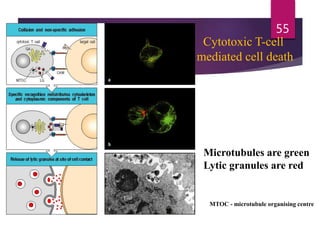
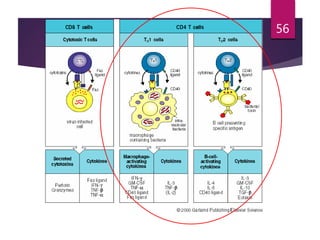
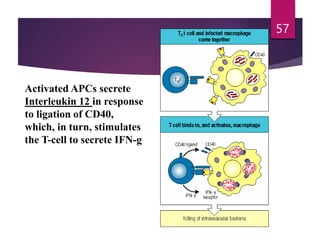
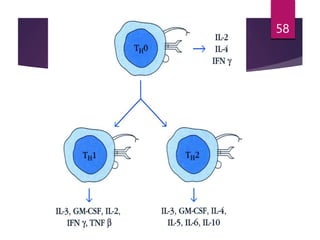
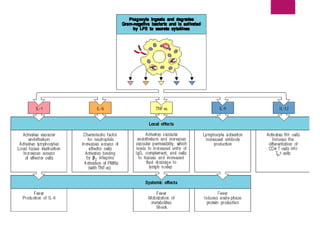
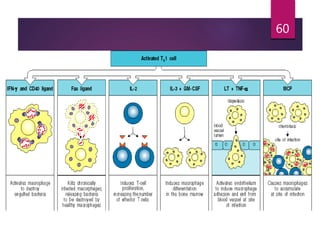
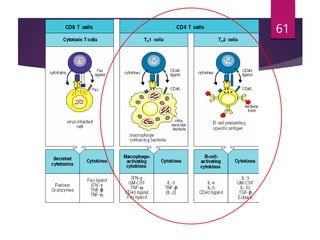
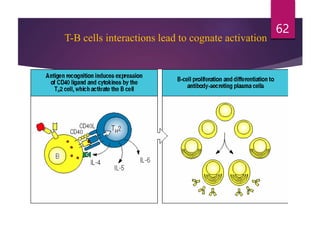
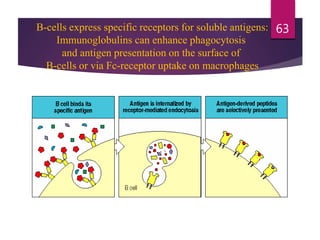
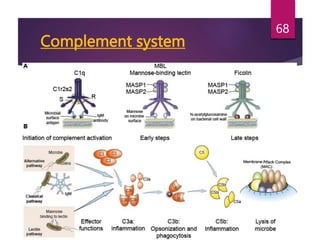
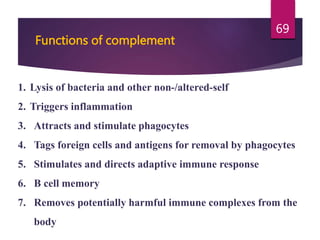
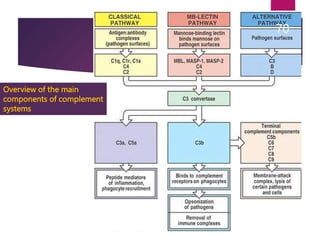
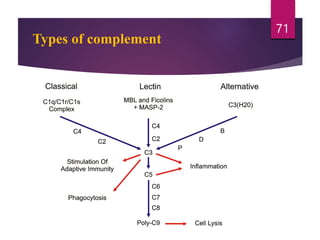
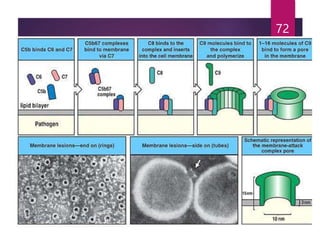
The document is a comprehensive overview of the immune system, detailing both innate and adaptive immunity, their components, and mechanisms, including the roles of various immune cells and responses. It describes the functions of humoral and cellular immunity, the activation of T and B cells, and the complement system's role in immune responses. Additionally, the document outlines hypersensitivity reactions and autoimmune diseases, providing examples and potential causes.