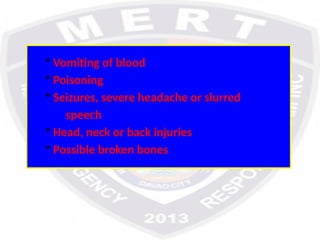
The document outlines the objectives and guidelines of a basic first aid training course designed for emergency response teams. It covers important topics such as the importance of first aid, roles, and permissions, types of injuries, and first aid management techniques for various scenarios. The training emphasizes both theoretical knowledge and practical skills, aiming to equip participants with the ability to provide effective emergency care.