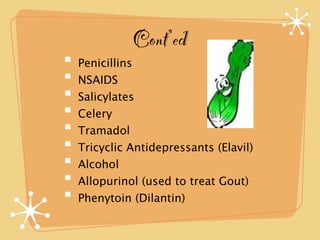
Great-Aunt Bea presented to the ER with a nosebleed that had stopped, but still felt unwell. She has a history of heart and lung conditions and was recently diagnosed with pneumonia. Her medications included Coumadin, but she was also taking azithromycin for pneumonia. Her INR was abnormally high at 13, likely due to an interaction between the azithromycin and Coumadin. She will be admitted to closely monitor and control her INR through vitamin K and possibly blood products due to the risk of internal bleeding. The nurse informed the physician and took appropriate steps to treat Great-Aunt Bea's high-risk condition.