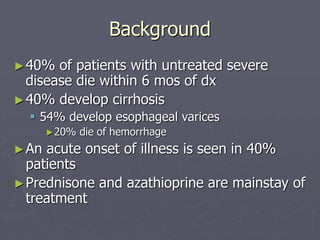
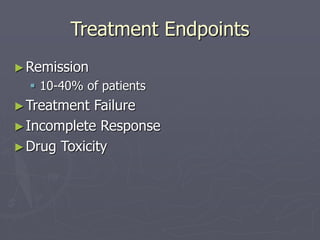
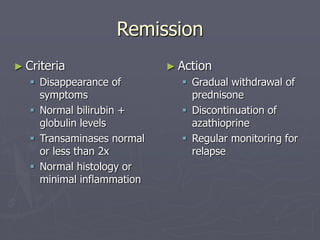
The document discusses a case presentation of a 54-year-old woman diagnosed with autoimmune hepatitis, detailing her medical history, laboratory findings, and treatment. Autoimmune hepatitis is characterized by hepatocellular inflammation, elevated liver-associated autoantibodies, and the exclusion of other liver diseases, with treatment primarily involving steroids and azathioprine. The document also covers epidemiology, clinical manifestations, diagnostic criteria, and treatment regimens, along with recommendations for management and prognosis.