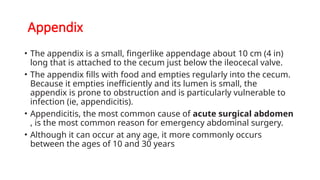
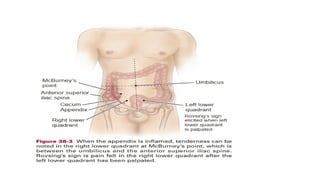
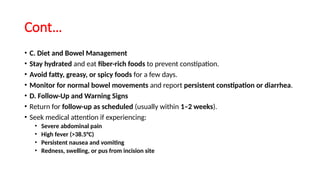
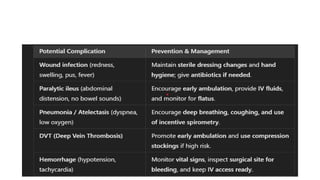
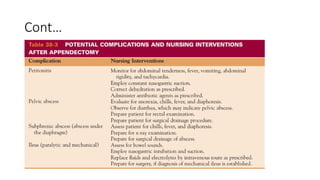
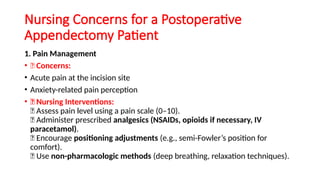
Appendicitis is an inflammation of the appendix, often necessitating surgical removal (appendectomy) due to complications such as obstruction caused by fecal matter or tumors. Symptoms typically include abdominal pain, nausea, vomiting, and fever, with diagnosis confirmed through physical exams and imaging tests. Postoperative care focuses on pain management, monitoring for complications, and educating the patient on recovery and wound care.