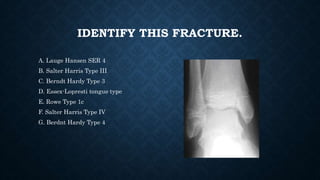
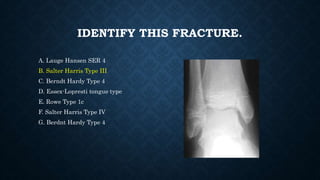
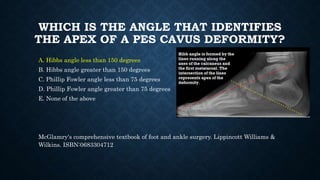
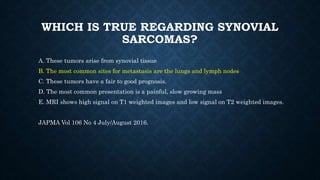
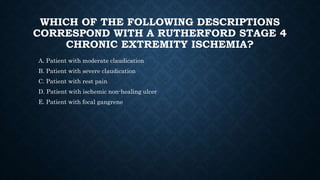
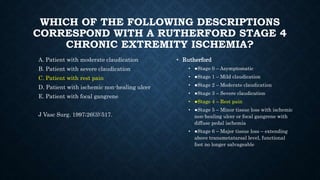
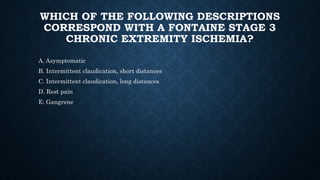
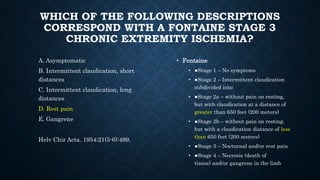
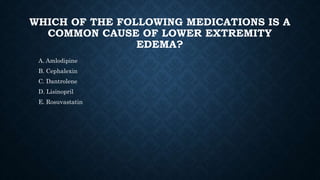
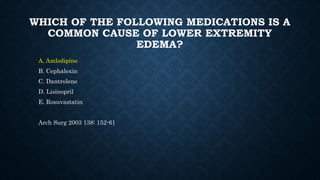
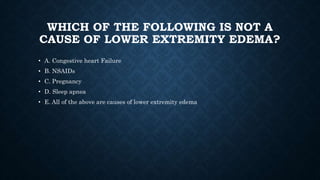
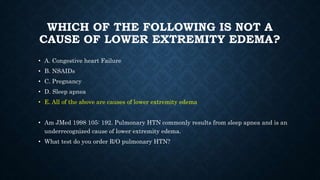
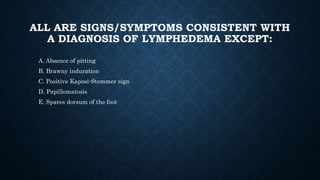
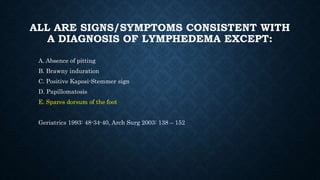
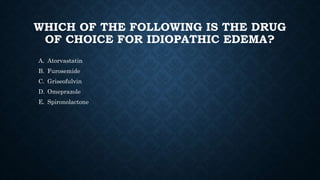
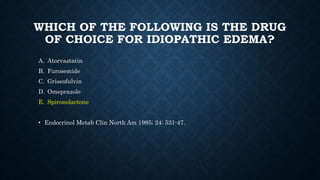
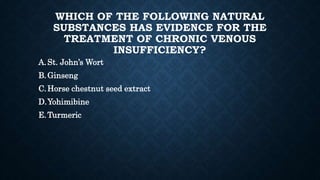
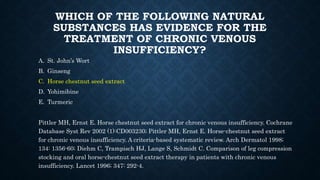
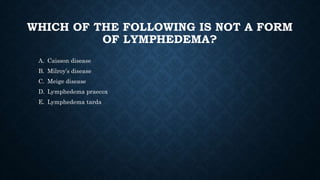
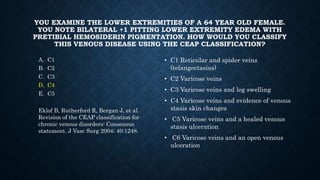
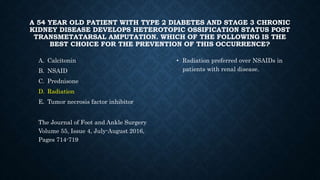
The document contains multiple choice questions related to orthopedic practice questions. Questions cover topics like ankle fractures, fracture blisters, fracture classifications, osteomalacia vs osteoporosis, foot deformities, vascular disease classifications, and causes of lower extremity edema. Answer choices are provided for each question.