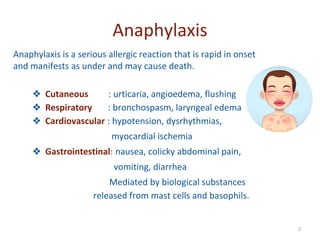
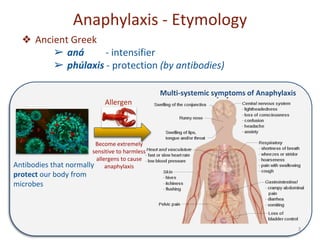
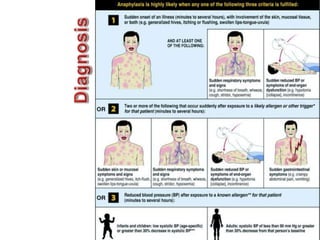
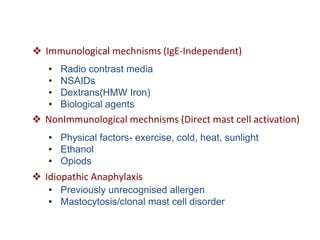
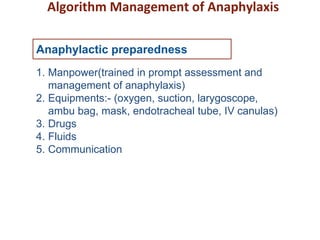
Anaphylaxis is a serious allergic reaction that affects multiple body systems and can cause death. It is caused by an immune system response to an allergen that results in the release of chemicals like histamine from mast cells that cause symptoms. Symptoms can include skin issues, respiratory distress, gastrointestinal issues, and cardiovascular problems. Treatment involves epinephrine injection, antihistamines, corticosteroids, monitoring vitals, and emergency transport if needed. Prevention focuses on having emergency medications available and management plans for high risk individuals.





![Initial management
Yes
• Assess airway, breathing,
circulation, mentation
• Inject epinephrine(IM)*
• Supine position
• IV access, oxygen, monitoring
No
Initial assessment supports
potential anaphylaxis?
Consider other diagnosis
*0.01ml/kg Epinephrine1:1000[IM]](https://image.slidesharecdn.com/anaphylaxis-220724091816-2cb8b810/85/Anaphylaxis-pptx-12-320.jpg)
![Good clinical
response?
Yes
No
Recumbent position with elevation
lower extremity • Establish airway,
O2 • Repeat epinephrine injection if
indicated
• IV fluids1 if hypotensive
Consider inhaled bronchodilators2 if
wheezing
• H1 and H2 antihistamines3
• Corticosteroids4
• Observation
• Autoinjectible
epinephrine
1NS or RL-30 mL/kg in 1st hr
2 Nebulised Albuterol- (0.83 mg/mL [3 mL]) via mask with O2
3cetrizine-0.25 mg/kg up to 10 mg PO, Ranitidine-1 mg/kg up to 50 mg IV
4methylprednisolone- 1-2 mg/kg up to 125 mg IV](https://image.slidesharecdn.com/anaphylaxis-220724091816-2cb8b810/85/Anaphylaxis-pptx-13-320.jpg)