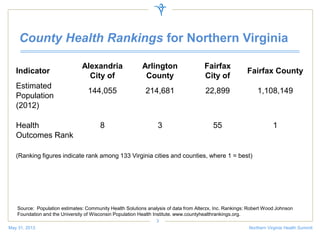
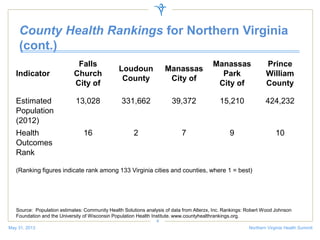
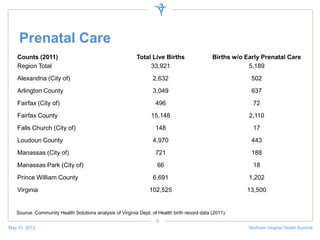
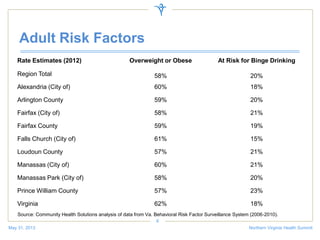
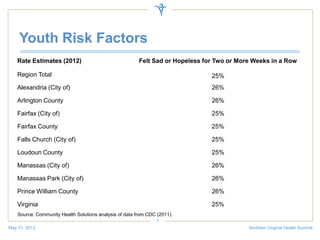
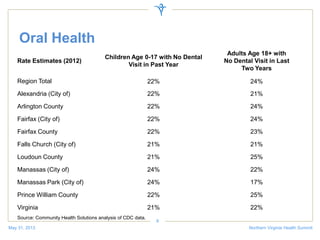
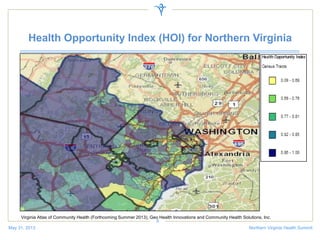
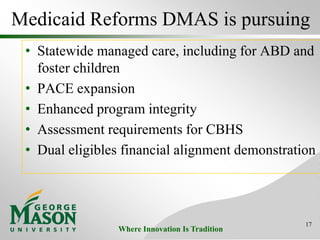
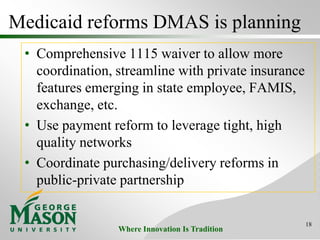
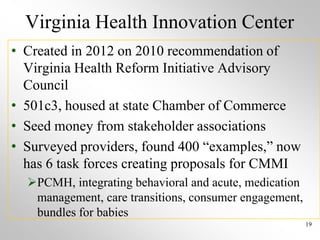
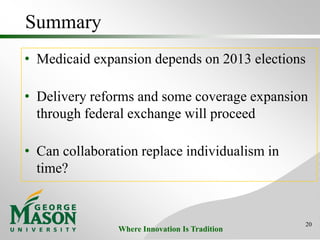
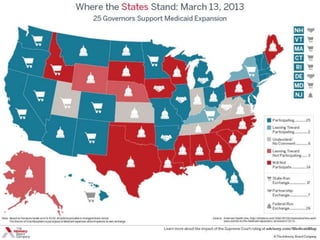
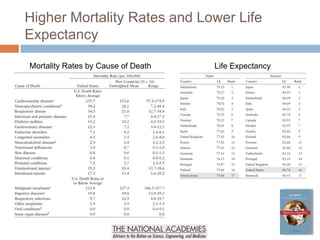
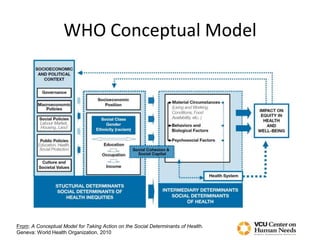
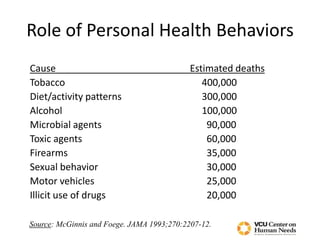
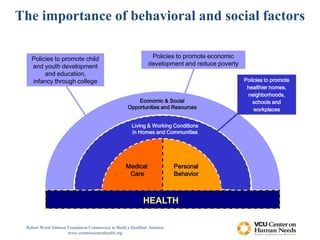
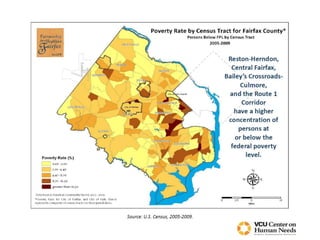
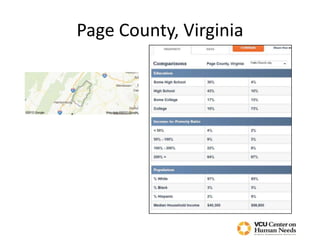
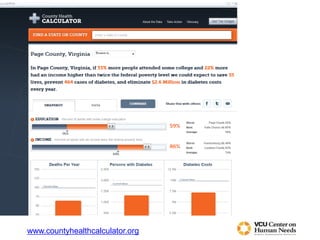
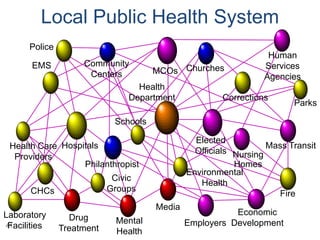
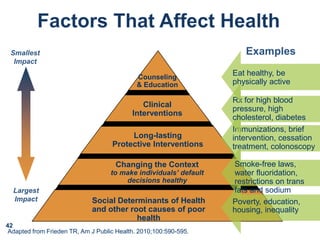
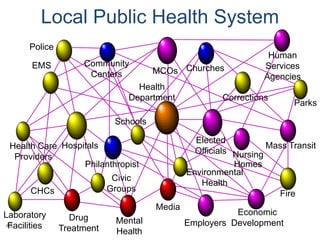
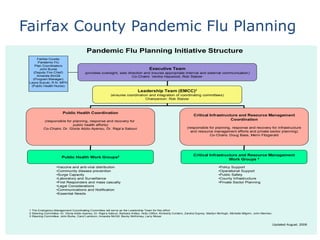
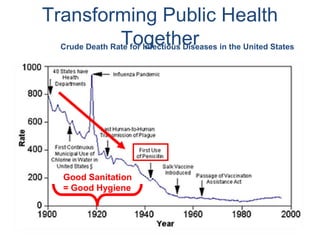
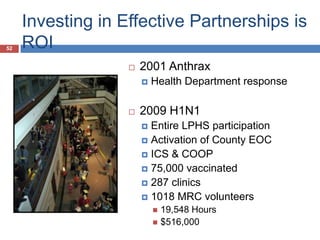
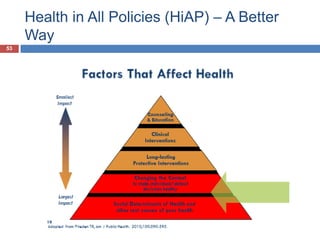
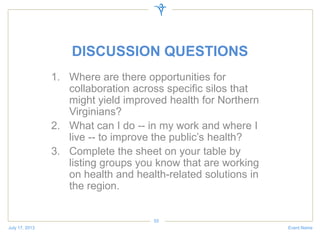
The document discusses a health summit held in Northern Virginia that reviewed health indicators and challenges across different counties in the region. It also covered topics like where the state of Virginia currently stands with health reform implementation and opportunities to advance delivery system reforms through public-private partnerships. Community partnerships were highlighted as important for addressing social determinants of health and mobilizing different agencies and groups to improve population health.