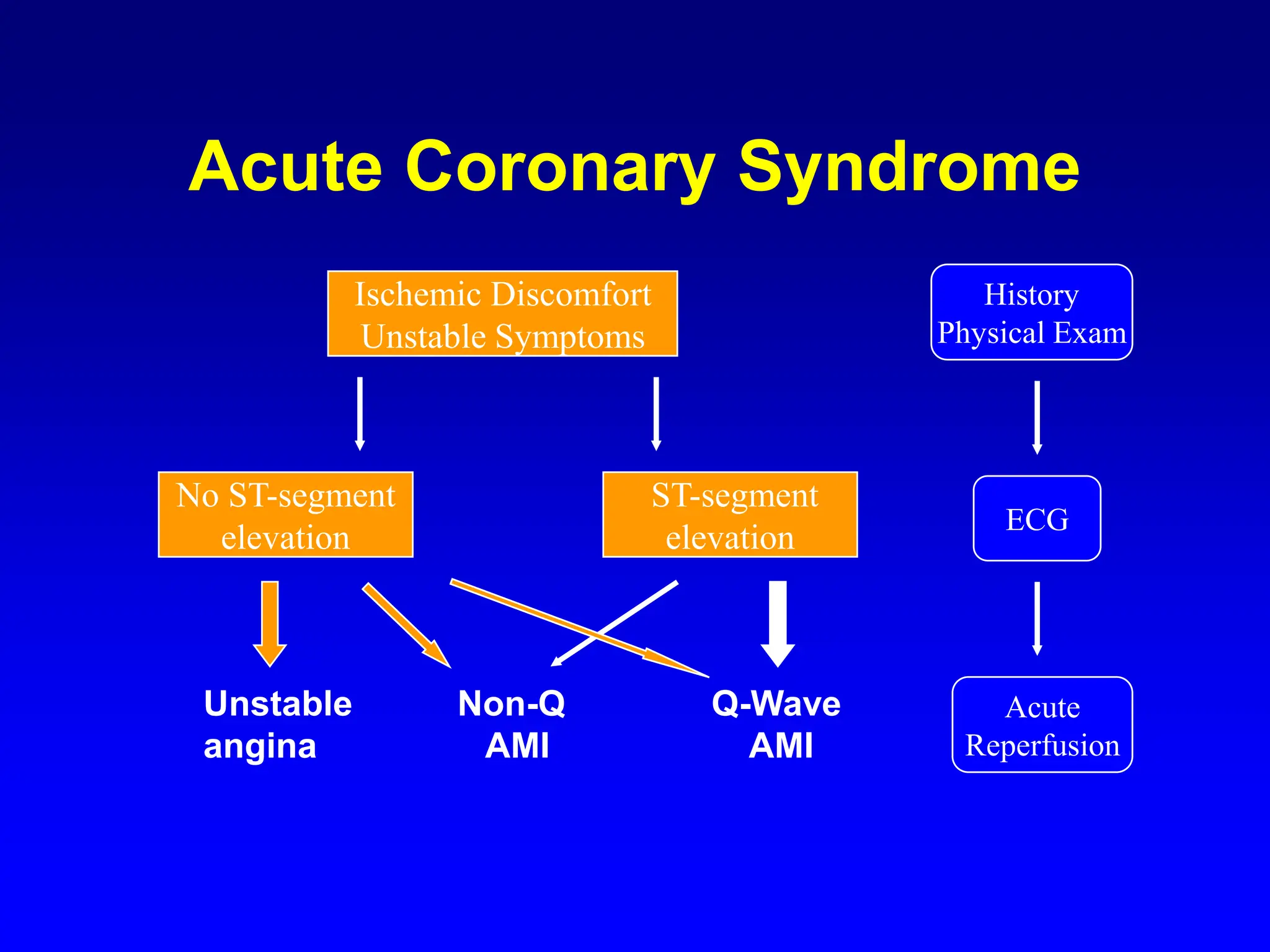
The document discusses acute coronary syndrome (ACS), detailing its diagnosis, treatment, and prevention of myocardial infarction (MI), noting that over 4 million patients experience unstable angina and acute MI annually. It outlines risk factors for atherosclerosis and MI, as well as symptoms, diagnostic procedures including ECG and cardiac enzyme studies, treatment protocols, and potential complications. Notable treatment measures include oxygen supplementation, aspirin, morphine, and thrombolytic therapy, with emphasis on risk stratification based on clinical signs and laboratory assessments.