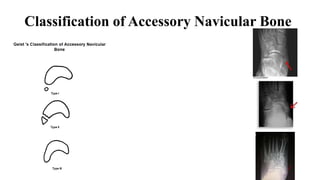
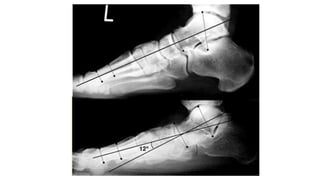
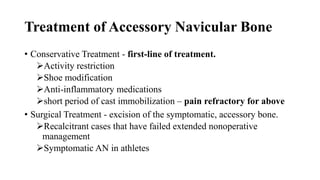
This document discusses the accessory navicular bone, a normal anatomical variant seen in around 12% of the population. It presents the case of a patient with a painful bony prominence on their left foot associated with their accessory navicular bone. The document covers the relevant anatomy, classification, pathophysiology, clinical presentation, differential diagnosis, imaging, and treatment options for symptomatic accessory navicular bone. Conservative treatment is usually first-line, while surgical excision may be considered for recalcitrant cases that fail extended nonoperative management.