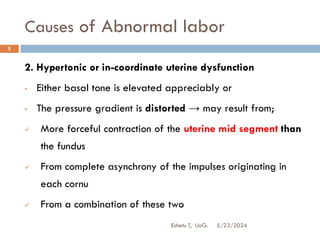
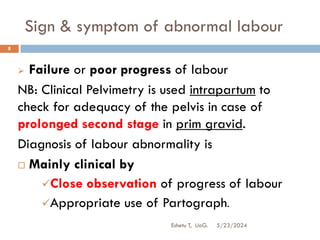
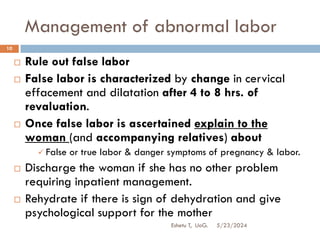
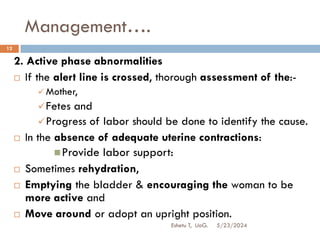
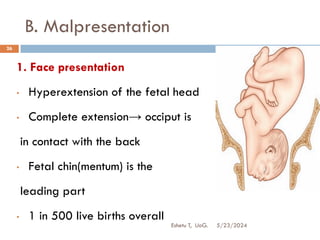
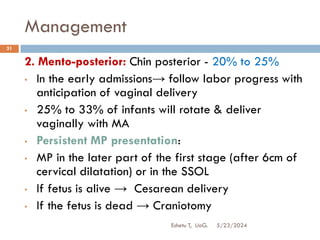
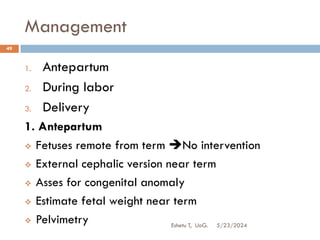
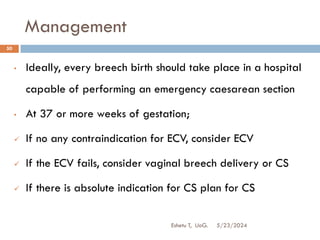
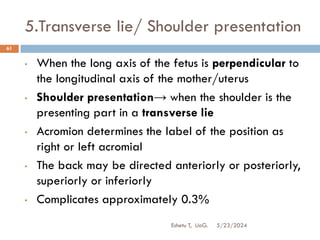
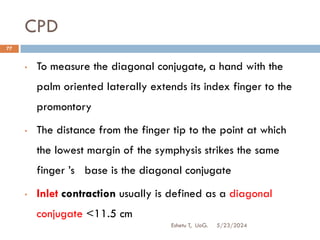
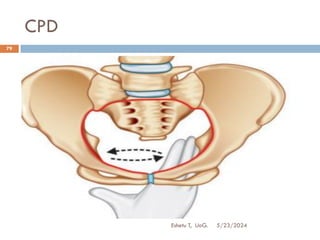
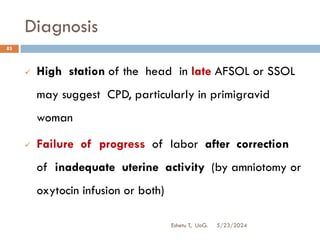
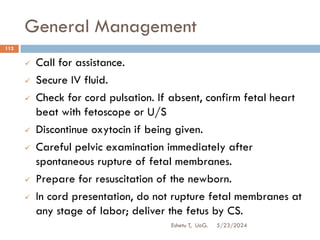
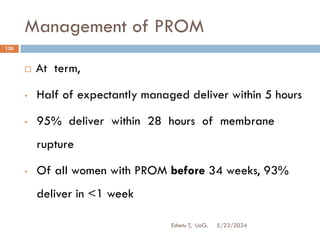
The document discusses abnormal labor, outlining its definitions, causes, diagnostic criteria, and management strategies. It emphasizes the impact of uterine contractions, the pelvis, and fetal positioning on labor progression, and identifies potential complications if not managed properly. The management approaches vary based on the specific type and phase of labor abnormality, highlighting the importance of clinical monitoring and intervention.