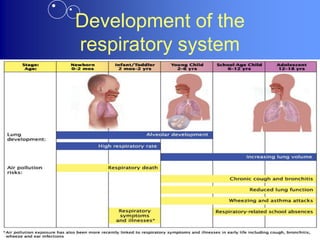
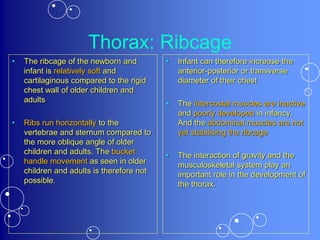
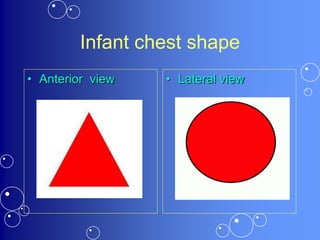
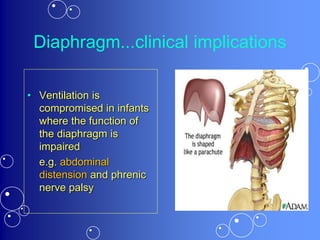
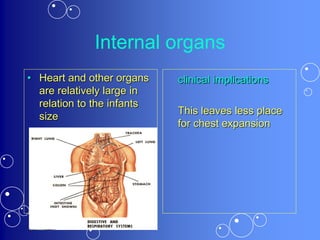
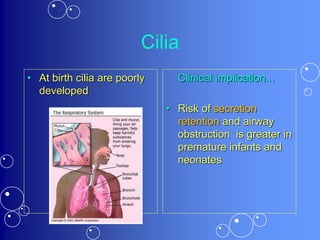
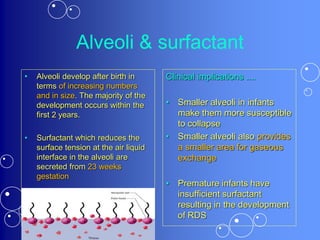
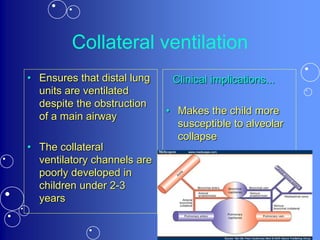
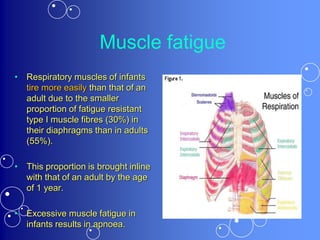
The respiratory system of children differs anatomically and physiologically from adults in several important ways. Anatomically, children have a more horizontal ribcage, larger internal organs relative to size, narrower airways, and less developed alveoli and cilia. Physiologically, children have greater airway resistance, lower respiratory compliance, higher oxygen consumption, and more easily fatigued respiratory muscles. These developmental differences impact a child's respiratory function and make them more susceptible to respiratory illnesses.