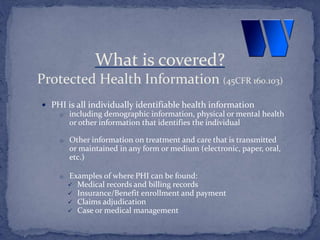
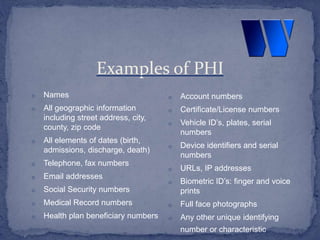
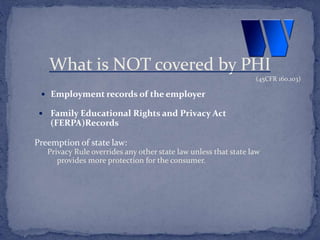
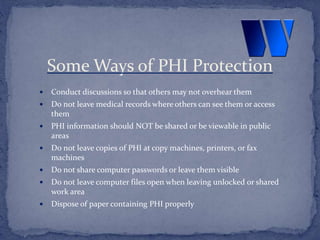
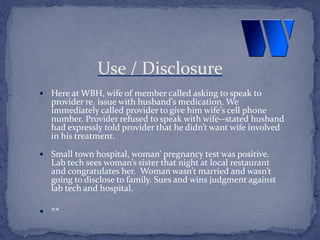
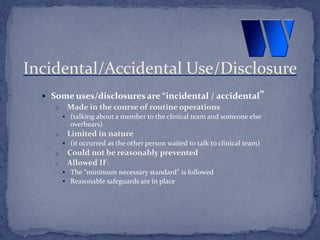
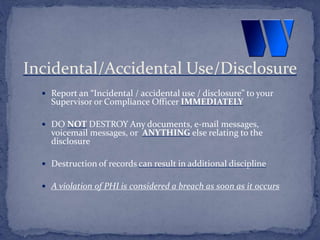
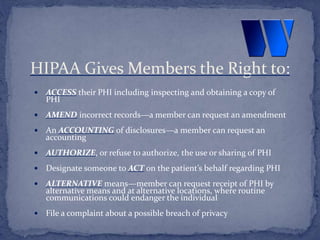
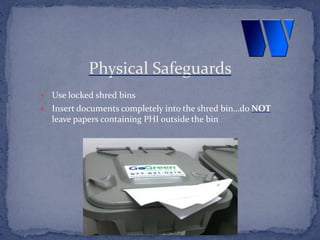
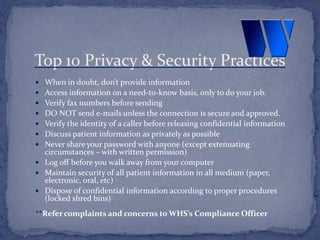
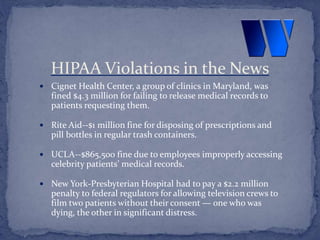
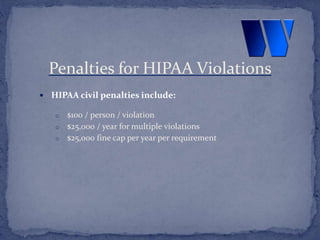
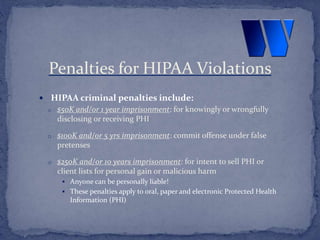
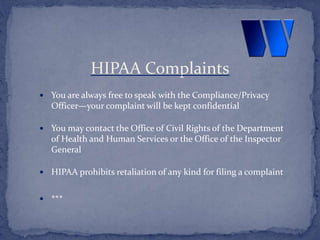
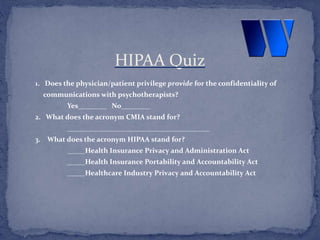
This document provides an overview of privacy training at Windstone Health Services. It covers the Health Insurance Portability and Accountability Act (HIPAA) and the Confidentiality of Medical Information Act (CMIA). It defines protected health information (PHI) and outlines employees' responsibility to protect PHI. It discusses appropriate use and disclosure of PHI, as well as patients' privacy rights. Violations of privacy laws can result in penalties such as fines and imprisonment. The corporate compliance department enforces privacy policies and can be contacted with any questions or reports of violations.