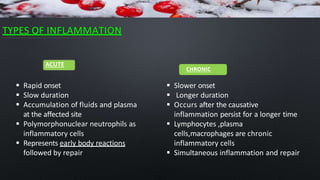
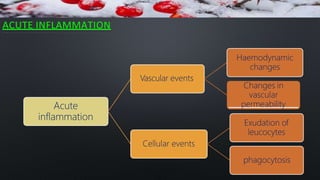
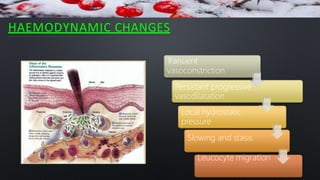
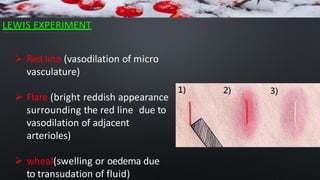
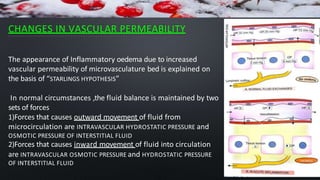
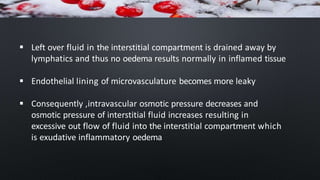
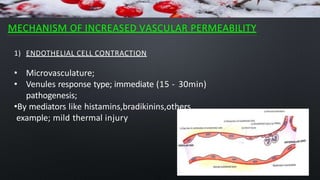
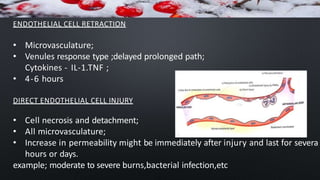
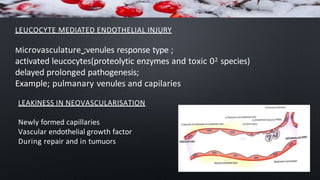
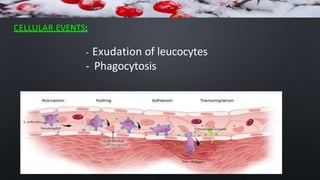
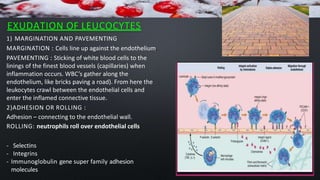
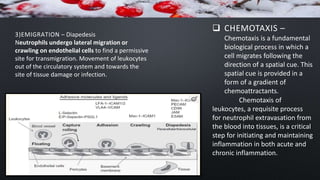
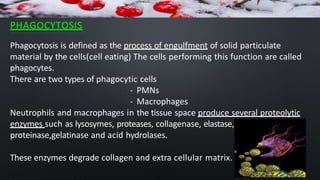
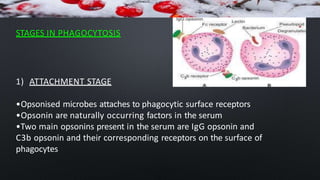
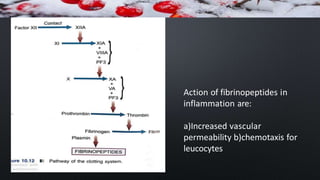
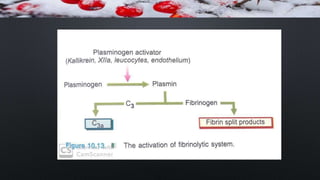
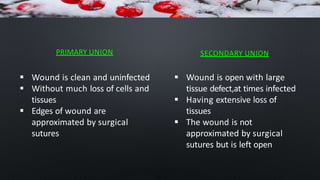
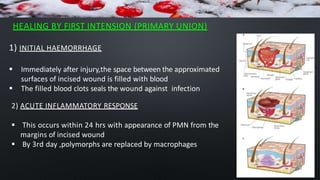
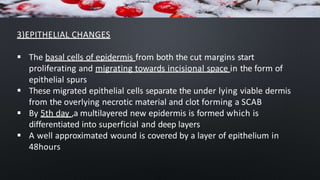
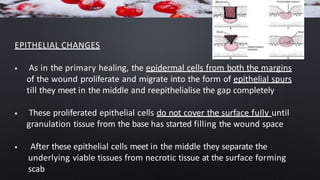
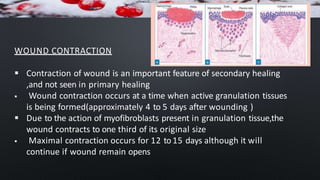
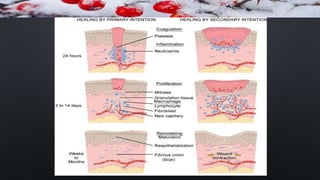
Inflammation and wound healing is a complex process involving several steps. It begins with an acute inflammatory response triggered by injury or infection, characterized by redness, swelling, heat and pain. This response involves increased vascular permeability, migration of white blood cells, and release of chemical mediators. Over time, the inflammatory response transitions to a chronic phase involving lymphocytes and macrophages. Wound healing occurs through regeneration or repair, involving re-epithelialization, granulation tissue formation, collagen deposition and wound contraction. Primary healing closes wounds through direct apposition of wound edges, while secondary healing relies on granulation tissue to fill open wounds.