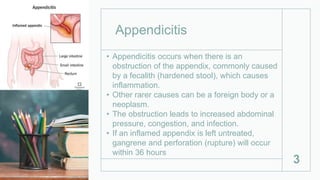
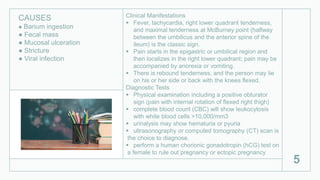
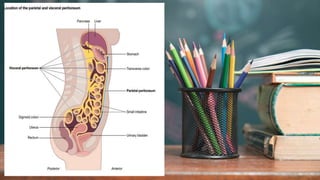
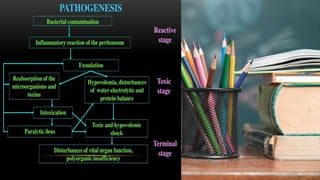
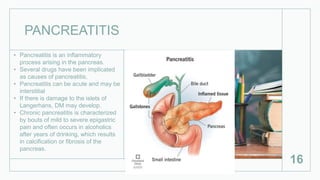
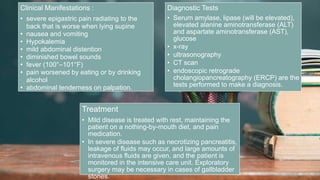
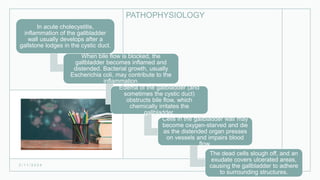
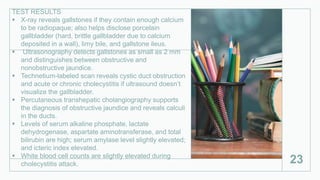
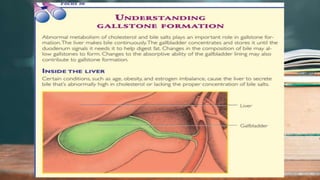
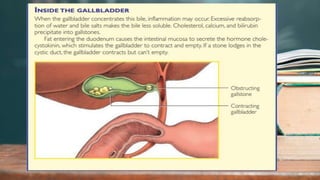
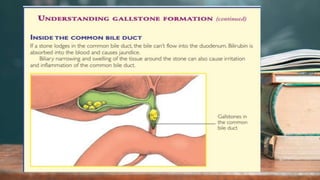
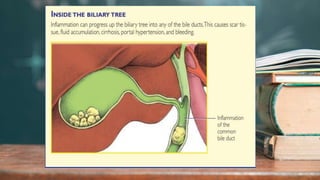
This document discusses several inflammatory conditions that can affect different body systems. It provides details on the causes, symptoms, diagnostic tests and treatments for appendicitis, peritonitis, pancreatitis, cholecystitis, and cystitis. Appendicitis is caused by obstruction of the appendix, usually by a fecalith, and requires appendectomy to prevent rupture. Peritonitis is inflammation of the abdominal lining that can result from a perforated appendix or other infections. Pancreatitis may be due to gallstones or alcohol and causes abdominal pain. Cholecystitis is gallbladder inflammation often from gallstones blocking the cystic duct. Cystitis is a urinary tract infection.






![TREATMENT
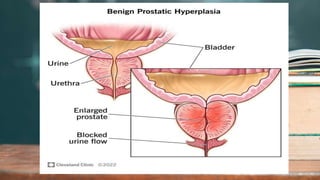
● transurethral resection (if the prostate weighs
less than 2 oz [56.7 g]); tissue removed with a wire
loop and electric current using a resectoscope
● suprapubic (transvesical) resection (most
common and useful for prostatic enlargement
remaining within the
bladder)
● retropubic (extravesical) resection allowing direct
visualization (potency and continence usually
maintained)
● balloon dilatation of the urethra and prostatic
stents to maintain urethral patency (occasionally)
● laser excision to relieve prostatic enlargement
● nerve-sparing surgical techniques to reduce
common complications such as erectile
dysfunction.
2 / 1 1 / 2 0 2 4
59](https://image.slidesharecdn.com/11-240211075654-e87ce464/85/11-Other-Problems-in-Inflammatory-Response-pptx-59-320.jpg)
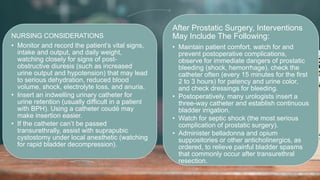
![NURSING CONSIDERATIONS
• After an open procedure, take patient comfort
measures
• Continue infusing I.V. fluids until the patient can drink
sufficient fluids (2 to 3 qt [2 to 3 L] per day) to maintain
adequate hydration.
• Administer stool softeners and laxatives, as ordered, to
prevent straining.
• Reassure the patient that temporary frequency,
dribbling, and occasional hematuria will likely occur
after the catheter is removed.
• Reinforce prescribed limits on activity.
• Instruct the patient about the prescribed oral antibiotic
drug regimen and the indications for using gentle
laxatives.
• Urge the patient to seek medical care immediately if he
can’t void or if he passes bloody urine or develops a
fever.
• Encourage annual digital rectal examinations and
screening for PSA to identify a possible malignancy.
2 / 1 1 / 2 0 2 4
61](https://image.slidesharecdn.com/11-240211075654-e87ce464/85/11-Other-Problems-in-Inflammatory-Response-pptx-61-320.jpg)
