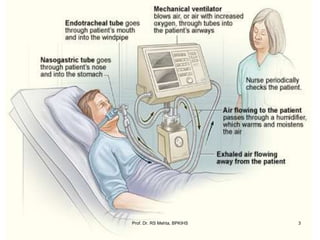
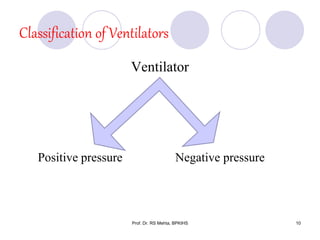
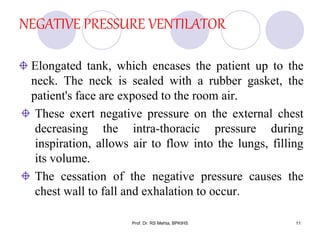
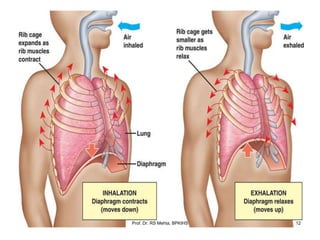
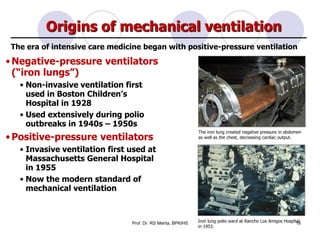
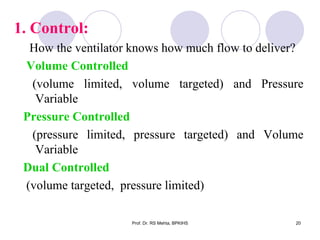
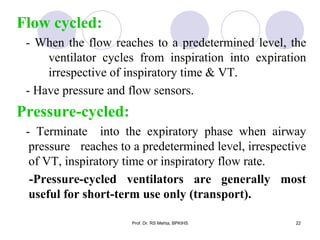
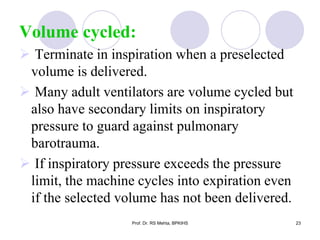
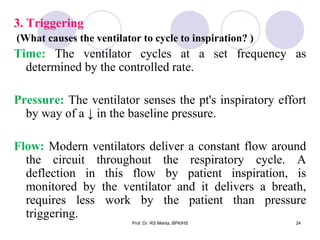
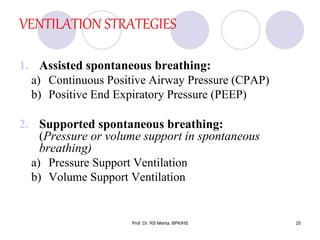
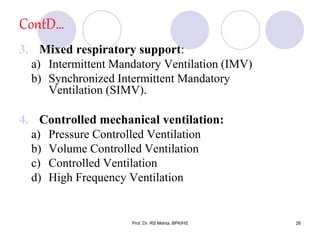
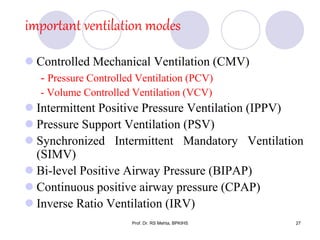
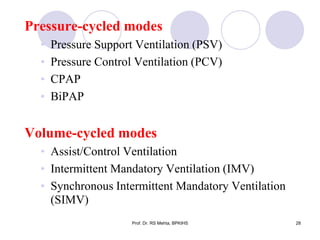
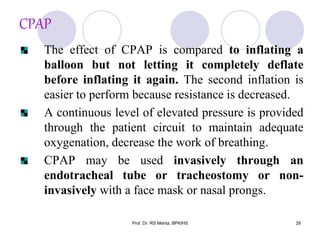
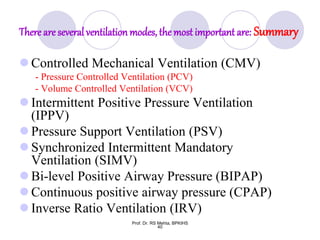
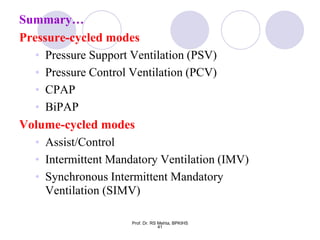
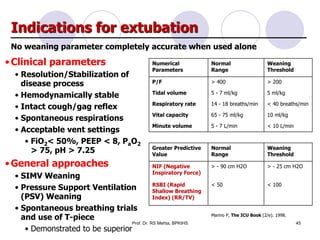
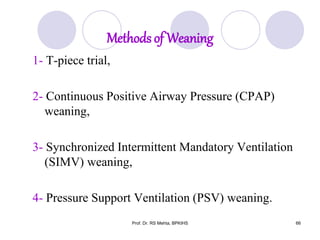
The document discusses mechanical ventilation and various ventilation modes. It describes how mechanical ventilators work using positive or negative pressure to maintain oxygen delivery. Some key ventilation modes discussed include CPAP which maintains continuous elevated airway pressure, PEEP which applies positive pressure at the end of expiration, and SIMV which provides mandatory breaths at set intervals allowing spontaneous breathing in between.