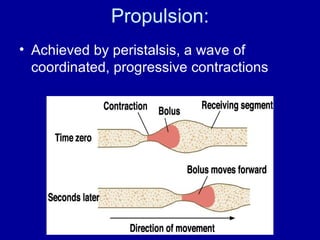
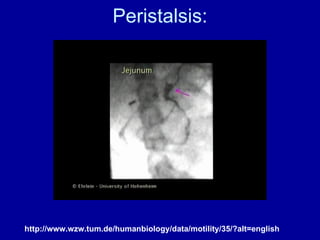
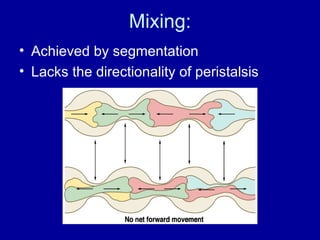
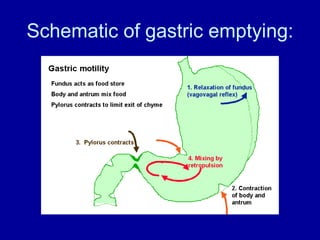
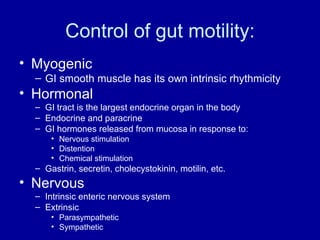
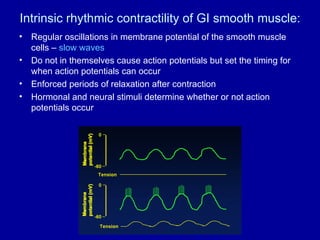
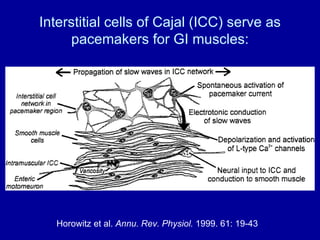
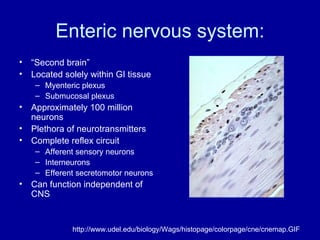
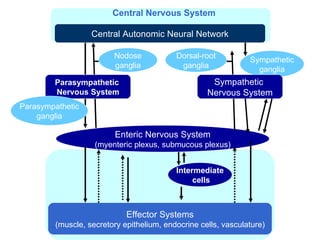
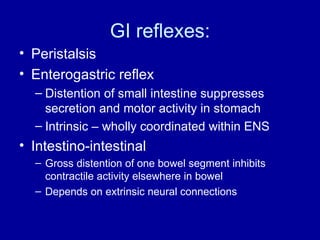
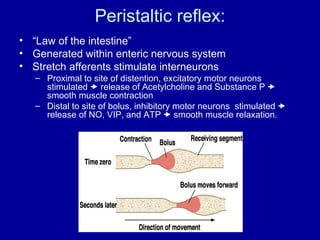
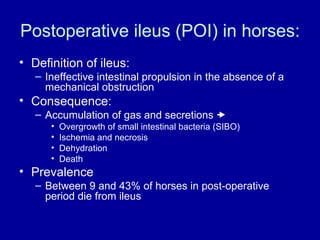
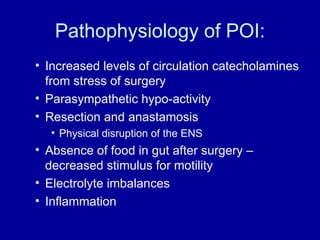
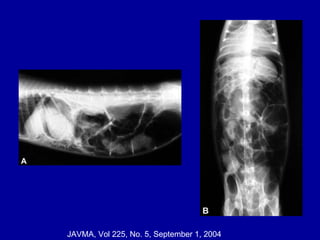
The document outlines the regulation of gastrointestinal (GI) function and motility, focusing on the patterns of motility, mechanisms controlling it, and the disturbances that can occur. It discusses the roles of myogenic activity, hormones, the enteric nervous system, and reflexes in maintaining GI motility, along with common motility disorders such as postoperative ileus and gastrointestinal stasis syndrome. Treatment approaches and key points about the intrinsic and extrinsic control of GI motility are highlighted.