Peritoneal Dialysis Care and History
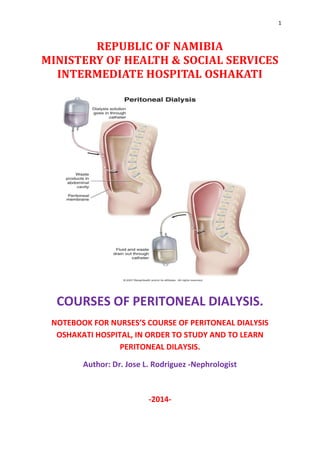
- 1. 1 REPUBLIC OF NAMIBIA MINISTERY OF HEALTH & SOCIAL SERVICES INTERMEDIATE HOSPITAL OSHAKATI COURSES OF PERITONEAL DIALYSIS. NOTEBOOK FOR NURSES’S COURSE OF PERITONEAL DIALYSIS OSHAKATI HOSPITAL, IN ORDER TO STUDY AND TO LEARN PERITONEAL DILAYSIS. Author: Dr. Jose L. Rodriguez -Nephrologist -2014-
- 2. 2 Index 1. Introduction 2. Chronic Kidney Failure. ESRD 3. History of Peritoneal Dialysis 4. What is the Peritoneal Dialysis 5. Dialysis physicochemical principles 6. Peritoneal access 7. Complication 8. Indications and Contraindications. 9. Types of Dialysis Peritoneal 10. Nursing Care and Management 11.Annexes
- 3. 3 1. Introduction This Certificate Course will provide the student acquire the skills necessary for comprehensive patient care in peritoneal dialysis, as well as the necessary skills in the field of health education, communication strategies and relationship to the renal patient. The nursing professionals have the opportunity to handle the equipment needed for renal replacement therapies in the later simulation rooms for care, under the supervision of experts, the patient and be part of the dialysis equipment for the duration of the internship clinics. On completing the program, students will be able to enter the labor market with a competitive and appropriate professional to the demands of this group of the population. Peritoneal dialysis is the most common form of renal replacement therapy performed in the home. Peritoneal dialysis is the process of removing excess fluid and metabolic by-products from the body by circulating dialysis solution through the peritoneal cavity using a peritoneal catheter. The group of Cuban doctors who worked on the creation of this book and the completion of this course student wish you success in learning and the beautiful task of saving lives with the use of this therapy. Lovingly.. Dr. Jose L. Rodriguez. Nephrologist. I.H.O. Namibia.
- 4. 4 2. Chronic Kidney Failure. ESRD Chronic kidney failure, also called chronic kidney disease, describes the gradual loss of kidney function. Your kidneys filter wastes and excess fluids from your blood, which are then excreted in your urine. When chronic kidney failure reaches an advanced stage, dangerous levels of fluid, electrolytes and wastes can accumulate in your body. In the early stages of chronic kidney failure, you may have few signs or symptoms. Chronic kidney failure may not become apparent until your kidney function is significantly impaired. Treatment for chronic kidney failure focuses on slowing the progression of the kidney damage, usually by controlling the underlying cause. Chronic kidney failure can progress to ESRD (end-stage kidney disease), which is fatal without artificial filtering (dialysis) or a kidney transplant. GFR <15 ml/mint./1.72m². SC. Creatinine>900 mg/dl., Urea> 40 mg/dl, K>7 mEq/L. Symptoms Signs and symptoms of kidney failure develop slowly over time if kidney damage progresses slowly. Signs and symptoms of kidney failure may include: Nausea Vomiting Loss of appetite Fatigue and weakness Sleep problems Changes in urine output Decreased mental sharpness Muscle twitches and cramps Hiccups Swelling of the feet and ankles Persistent itching
- 5. 5 Chest pain, if fluid accumulates around the lining of the heart Shortness of breath, if fluid accumulates in the lungs High blood pressure (hypertension) that's difficult to control Signs and symptoms of kidney failure are often nonspecific, meaning they can also be caused by other illnesses. In addition, because your kidneys are highly adaptable and able to compensate for lost function, signs and symptoms of kidney failure may not appear until irreversible damage has occurred. Causes Chronic kidney failure occurs when a disease or condition impairs kidney function, causing kidney damage to worsen over several months or years. Diseases and conditions that commonly cause chronic kidney failure include: Type 1 or type 2 diabetes High blood pressure Glomerulonephritis (gloe-mer-u-lo-nuh-FRY-tis), an inflammation of the kidney's filtering units (glomeruli) Polycystic kidney disease Prolonged obstruction of the urinary tract, from conditions such as enlarged prostate, kidney stones and some cancers Vesicoureteral (ves-ih-koe-yoo-REE-ter-ul) reflux, a condition that causes urine to back up into your kidneys Recurrent kidney infection, also called pyelonephritis. Complications Chronic kidney failure can affect almost every part of your body. Potential complications may include: Fluid retention, which could lead to swelling in your arms and legs, high blood pressure, or fluid in your lungs (pulmonary edema) A sudden rise in potassium levels in your blood (hyperkalemia), which could impair your heart's ability to function and may be life-threatening Heart and blood vessel disease (cardiovascular disease) Weak bones and an increased risk of bone fractures Anemia Decreased sex drive or impotence Damage to your central nervous system, which can cause difficulty concentrating, personality changes or seizures Decreased immune response, which makes you more vulnerable to infection Pericarditis, an inflammation of the sac-like membrane that envelops your heart (pericardium)
- 6. 6 Pregnancy complications that carry risks for the mother and the developing fetus Irreversible damage to your kidneys (end-stage kidney disease), eventually requiring either dialysis or a kidney transplant for survival. 3 -History of Peritoneal Dialysis Peritoneal dialysis – from the beginning to the present When symptoms of uremia first appear in the body, it is a sign that the kidneys are not functioning properly or have stopped filtering toxins from the blood. The Greek origin of the word “uremia” shows that the awareness of this disease goes back much further than our ability to effectively treat people this life-threatening illness. Only within the last hundred years medical research has been able to lay the fundament for replacing the kidneys’ functions through dialysis. The first progress with this treatment type was made during the 1920s, but it would take a number of subsequent discoveries in the following decades to make peritoneal dialysis accessible for a larger number of patients with kidney disease. These advances were achieved by dedicated doctors and scientists whose efforts and discoveries led to ever- improving treatment possibilities. On the following pages, we offer an introduction to the fascinating history of peritoneal dialysis and the discoveries which, to this day, help to ensure a longer and better life for more than 250,000 peritoneal dialysis patients worldwide. The fundamentals of peritoneal dialysis As described in the introduction, peritoneal dialysis is one of the two established methods to remove toxins and excess water from the human body. The lining of the abdomen (peritoneum) is a thin, shiny membrane that has a surface of as much as two square meters and covers the entire abdominal cavity. Since the peritoneum has good blood circulation, it is an excellent natural filter membrane.
- 7. 7
- 8. 8
- 9. 9 Peritoneal Dialysis Catheter Care GENERAL INFORMATION: Peritoneal dialysis (PD) uses the lining of your abdomen (the peritoneal membrane) to filter your blood. A small, soft tube called a catheter is used to fill your abdomen with minerals and sugar dissolved in water. This cleansing liquid is called dialysis solution. Wastes, chemicals, and extra water move into the dialysis solution while it is in your abdomen. After a certain time, the solution is drained from your abdomen through the catheter, taking the wastes with it. Your abdomen is then filled again with new dialysis solution. Each cycle of filling and draining is called an exchange. PD can be done in different ways. Continuous cycler-assisted peritoneal dialysis (CCPD) uses a machine called a cycler to fill and drain your abdomen. It is usually done a few times while you sleep. CCPD is also sometimes called automated peritoneal dialysis (APD).
- 10. 10 Continuous ambulatory peritoneal dialysis (CAPD) uses gravity instead of a machine to fill and empty your abdomen. With CAPD, you do manual exchanges of fluid a few times during the day. You drain a fresh bag of dialysis solution into your belly by hanging the bag higher than your belly. For a number of hours you let the fluid work inside your belly to remove the waste fluids. Then you drain the fluid from your belly by hanging the bag at a level lower than your belly catheter. Before your first treatment, the catheter used for peritoneal dialysis is put into your belly through a small cut near your belly button. Your healthcare provider will make the cut and insert the catheter after you have been given an anesthetic. The catheter will be closed with a clamp or valve when you are not having dialysis. Your provider will give you a schedule for how often you will need to have dialysis. You will have frequent weigh-ins and lab work to make sure the dialysis is helping you get rid of wastes and keep a good balance of minerals. What are the benefits of dialysis? Dialysis does the work your failed kidneys would normally do. It keeps your blood clean and healthy. If you have kidney failure, dialysis can help you live longer. If you are otherwise healthy, dialysis may allow you to keep working or enjoying the things you like to do. If you are very sick and have other health problems, dialysis may seem like a burden that only prolongs your suffering. Having dialysis is a very personal decision to be discussed with your family and your healthcare provider. What are the risks of dialysis? Possible problems with hemodialysis include: problems with the access to your blood vessels, such as infection, blockage from clotting, and poor blood flow muscle cramps a sudden drop in blood pressure, which can make you feel weak, dizzy, or sick to your stomach. The most common serious problem with peritoneal dialysis is an abdominal infection called peritonitis. The infection can be treated with antibiotics. How can I take care of myself? Carefully follow the diet prescribed by your healthcare provider. Do not drink more liquids than your provider recommends. Follow the dialysis schedule as prescribed. Take medicines exactly as prescribed by your provider. If you are having hemodialysis, tell your provider if you have muscle cramps or feel weak, dizzy, or sick to your stomach.
- 11. 11 If you are having peritoneal dialysis, tell your provider right away if you have these signs of infection: You have a fever. You have belly pain. The used dialysis solution has an unusual color or cloudiness. The area around the catheter is red or painful. What is continuous ambulatory peritoneal dialysis? Continuous ambulatory peritoneal dialysis (CAPD) is done to remove wastes, chemicals, and extra fluid from your body. The peritoneum is a thin lining on the inside of your abdomen. During CAPD, a liquid called dialysate is put into your abdomen. It is put in through a CAPD catheter. The catheter is a tube that goes from the outside, to the inside of your abdomen. The dialysate pulls wastes and substances from your blood and lymph fluid through the peritoneum. The wastes mix with the dialysate. The peritoneum works like a filter as the wastes are pulled through it. The dialysate is left in your abdomen for 3 to 5 hours. This is called the dwell time. After the dwell time, the dialysate is drained out through the catheter. Filling and emptying your abdomen with dialysate is called an exchange. CAPD exchanges can decrease or take away problems such as swelling, itching, fatigue, and weakness. CAPD can help decrease high blood pressure, and make you feel more like doing the things you enjoy. When and how often should I do peritoneal dialysis? You and your caregiver will decide how many exchanges you need to do each day. Your caregiver will also discuss which type of PD may be best for you. During continuous ambulatory peritoneal dialysis (CAPD), you may need to do 3 to 5 exchanges during the day, and one exchange during the night. Automated peritoneal dialysis (APD) uses a cycler (special machine) to do your exchanges. One exchange is done during the day, and 3 to 5 exchanges are done during the night while you are asleep.
- 12. 12 How are CAPD exchanges done? Do your CAPD exchanges in a well-lit room that has no pets, dander, strong breezes, or fans. Having pets or a breeze blowing in the room may increase your risk of getting an infection. Supply list: Collect the following supplies and place them on a clean table close to where you will be doing your CAPD exchange: o Clean water and soap. o Dialysate bag. o Waste product bag. o "Y"-shaped tubing. o IV stand. This is needed so that you can hang your dialysate bag on it. The stand should have a hook at the top to help hold the bag in place. The dialysate fluid drains into your abdomen by gravity. Because of this, the bag needs to be hung up higher than the level of your abdomen. o Disposable (single use) medical gloves. o Medical mask to wear over your face while doing CAPD. o Tubing clamp, and a piece of soft cloth. Use the cloth as padding between the clamp and catheter when you are clamping the catheter tube. This will decrease the chance that the clamp will make a hole or crack in the catheter. Ask your caregiver about other clamps that are less likely to break the catheter or make holes in it. o New plastic syringe without a needle (if needed). Wash your hands with soap and water: Rub your hands together with soap for at least 15 seconds before rinsing them. Dry your hands with a clean towel or paper towel. Do not touch the tubing or your catheter without washing your hands and wearing gloves. Put on your gloves and mask: Put on your mask so that it covers your mouth and nose. Keep your fingernails short and clean. Do not use fake nails. Put on your gloves, being careful not to touch anything except your supplies while they are on. Flush the tubing: Flushing the tubing with dialysate liquid before doing CAPD may help prevent infections. Connect the lower end of the Y tubing to your catheter. Connect the two other ends of the tubing to the dialysate bag, and the waste bag. Clamp the tubing that is attached to the catheter that goes into your abdomen. This will close off the tubing so that the dialysate does not go into your abdomen yet. Allow 100 milliliters of fresh dialysate to flow out of the bag, and down the tubing into the waste bag. After this amount of dialysate has drained out, clamp the tubing that goes to the waste bag closed. Let the dialysate flow into your abdomen: Take the clamp off of the tubing that is attached to the catheter that goes into your abdomen. Let the rest of the dialysate flow into your abdomen. You may lie down, sit, or stand up while the dialysate flows in. After all of the dialysate is in your abdomen, wash your hands and put on new gloves. Disconnect your catheter from the tubing. Clamp your catheter closed. Leave the dialysate in your abdomen for 3 to 5 hours of dwell time. Drain the dialysate out of your abdomen, and into the waste bag: After the dwell time, follow the steps of washing your hands and putting on your mask and gloves. Be sure the supplies that you need are easy to reach and use. Connect the Y tubing to your catheter again. Do this in the same way as you did to put the dialysate into your abdomen. Clamp the tubing that goes to the dialysate bag so that it is closed. Remove the clamps from your catheter
- 13. 13 and the waste bag. Let the dialysate drain from your abdomen and into the waste bag. Throw away the waste bag as directed by your caregiver. What problems might I have when I have a CAPD catheter? Tell your caregiver if you have any of the following problems: Hernias (lumps) at your catheter exit site, belly button area, or groin. A hernia is a fluid-filled sac. This sac may be caused by too much dialysate going into your abdomen. Tell your caregiver if you see or feel a new lump on your abdomen. Infection: Yellowish discharge (pus) may come out from the exit site or out of your catheter. The exit site may look red and be painful to touch. You may have a fever and chills, or feel very weak. You may feel sick, or start throwing up. You may be constipated. Tell your caregiver if you get any of these problems. Leaking dialysate from the exit site: You may see dialysate leaking from the exit site for up to a month after you have your catheter put in. You may notice that the dialysate drains out more slowly during exchanges, or there is less of it. Pain: The skin around your exit site may be painful. You may feel pain in your pelvis, low back, and shoulder while doing CAPD exchanges. Change your body position when you are doing your exchanges. Try lying down, sitting, or standing up. Ask your caregiver for exercises that you may be able to do to help decrease back pain. Stomach swelling: You may feel full during and after CAPD exchanges. This feeling may go away over time. If it does not go away, talk to your caregiver. What should I do when there is a flow problem with my peritoneal dialysis catheter? When the dialysate is flowing into your abdomen during an exchange (inflow), the flow may slow down or even stop. When the dialysis is draining out of your abdomen during an exchange (outflow) this may also be a problem. The dialysate should take about ten minutes to flow into your abdomen. The dialysate should take less than 45 minutes to drain out of your abdomen. Inflow or outflow problems may mean that your catheter is blocked, or that the tube has moved out of the right place. If the inflow or outflow of the dialysate is slow, you may try the following: o Put in 10 to 20 ml of dialysate or saline solution into the catheter using a syringe. Hold the catheter and syringe in one hand. Use your other hand to firmly push the dialysate out of the syringe, through the catheter, and into your abdomen. This may push out the blood clot or move whatever is blocking your catheter. After doing this process a few times, use the syringe to try and pull fluid out gently. If fluid comes out, the catheter is no longer blocked. If this does not help, your caregiver may need to put medicine through the catheter that breaks down blood clots. If the inflow of the dialysate is fast but there is no outflow, you may try the following: o Change your position while doing your exchanges. You may sit up, lie down, or lie on your side. You may even lie with your head down and your feet up. Changing your position may make the dialysate flow out more easily. If this does not help, disconnect the end of the tubing that is attached to your catheter. Use a syringe to gently suck the dialysate out of your abdomen. Do not pull on your catheter. It may move your catheter out of place even more. You may also start bleeding if you pull on it. If the flow does not get faster, call your caregiver.
- 14. 14 What diet changes may I need to make while I am doing peritoneal dialysis exchanges? You may lose weight and become weak when you are doing CAPD exchanges. You may not feel like eating. Your body may lose protein and other nutrients that you need to be healthy. You may need to increase the fiber in your diet by eating more vegetables and fruits. Fiber helps you have regular, soft bowel movements (stools), and helps prevent constipation. Decreasing the amount of salt in your diet may decrease your blood pressure. Ask your caregiver what diet is best for you, and for more information about it. Your caregiver will ask you to limit the amount of liquids you drink. Your caregiver will tell you how much to drink each day. Write down how much liquid you drink each day. Measure the amount of urine you pass each time you go to the bathroom. Show this information to your caregiver when you have follow-up visits. He will tell you if you have too much or too little fluid in your body, and what to do to correct it. How and when are the bandages around my peritoneal dialysis catheter changed? Your caregiver will change your bandages every week for the first two weeks. On the third week, your bandages may need to be changed more often. When your exit site is healed up, you may need to change your bandages every day. A healed exit site is pink in color, and at least 13 millimeters in size (smaller than a dime). The area should not be painful. Change your bandages as follows: Collect your supplies: o Sterile (clean and new) medical gloves. o Medical mask. o New bandages. o Soap and fresh water. o Solution for removing old bandages and cleaning your skin. Ask your caregiver what solution is best to use. o Medical tape. Wash your hands: Use soap and water to wash your hands. Scrub them for at least 15 seconds. Dry your hands well with a clean towel or new paper towel. Put on your mask and gloves: Put on your mask, making sure that it covers both your nose and your mouth. This will help prevent germs from your nose or mouth going on your exit site. Put on your gloves. Do not touch anything other than the bandage and your supplies when your gloves are on. Avoid moving your catheter: Do not pull or twist your catheter when changing your bandages. Make sure that your catheter stays in its place. Remove old bandages: Use a sterile solution to carefully remove old bandages from the exit site. Pour the solution over bandages that are stuck on your exit site to loosen them. If there is a scab (dried up skin or blood), do not pull on it. Take off the bandage very slowly. Look for pus, fluid, or blood coming from the exit site. If you see these things, call your caregiver. If the area is painful, call your caregiver.
- 15. 15 Clean your wound, catheter, and skin: Wipe the exit wound, catheter, and skin around the catheter with a sterile solution. Pat the area dry with a clean bandage. Cover your catheter and the exit site with bandages: Covering your catheter when you are not using it may help it stay in place. This may help stop the catheter from bending and kinking, or being pulled out. Use several layers of bandages to cover the exit site and the skin around your catheter. Hold the bandages in place with tape. Can I bath or shower while I have a peritoneal dialysis catheter? You cannot take a bath or shower until two weeks after your catheter was placed. Getting your exit site wet may delay healing. Use a washcloth, soap, and water to wash your skin. When the exit site heals, your caregiver may let you take a shower. If you take baths, do not let the exit site go under the water. Leave the bandages on until after your bath, and then put on new bandages. After your exit site has fully healed, you may swim in the ocean or chlorinated swimming pools. Dry the exit site right after swimming. Avoid using hot tubs, and swimming in rivers or ponds. What else can I do to help prevent infection at the catheter exit site? Keep your catheter held in the right place: Ask your caregiver how to tape your catheter to your body. This may help prevent the catheter from twisting and being moved or pulled out. Change your bandages as ordered by your caregiver: Germs may grow on the exit site and on old bandages. Change your bandages every day, or as often as your caregiver has told you to. You may need to keep your exit site covered with bandages for six months to a year. Take antibiotic (germ-killing) medicine as ordered: This medicine helps prevent or treat infection. When will my peritoneal dialysis catheter be removed? Your catheter can be used for up to two years if it is not blocked or damaged. Your caregiver may need to remove it if you get an infection. He may replace it when it is cut, clogged, or damaged. It will be removed if you need to have hemodialysis instead of PD. Your caregiver will remove it if you do not need to have dialysis anymore. When should I call my caregiver? Call your caregiver if: Pus or fluid is draining out of the exit site. The dialysate that drains out of your abdomen looks cloudy. The exit site is bigger than it used to be. There is no dialysate flowing out of your abdomen during an exchange, even after changing positions and using a syringe. You have a fever (high body temperature) or chills. You have dull pain in your abdomen while doing a dialysis exchange. There is a new bump that has grown in your abdomen since you have started doing CAPD exchanges. Your catheter exit site is red, tender or painful. You have questions about CAPD or your catheter. When should I seek immediate help? Seek care immediately or call 911 if: You have hard, painful bowel movements and the stool is hard to pass. You have stomach pain, and you are vomiting (throwing up). You have trouble breathing while doing your exchanges. Your catheter has a crack or hole in it, or it has come part or all of the way out of your abdomen.
- 16. 16 4. What is the Peritoneal Dialysis Before dialysis was available, total kidney failure meant death. Today, people with kidney failure can live because of treatments such as dialysis and kidney transplant. What is dialysis? Dialysis is a way of cleaning your blood when your kidneys can no longer do the job. It gets rid of your body's wastes, extra salt and water, and helps to control your blood pressure. Are there different types of dialysis? There are two kinds of dialysis. In hemodialysis, blood is pumped out of your body to an artificial kidney machine, and returned to your body by tubes that connect you to the machine. In peritoneal dialysis, the inside lining of your own belly acts as a natural filter. Wastes are taken out by means of a cleansing fluid called dialysate, which is washed in and out of your belly in cycles. How does peritoneal dialysis work? A soft plastic tube (catheter) is placed in your belly by surgery. A sterile cleansing fluid is put into your belly through this catheter. After the filtering process is finished, the fluid leaves your body through the catheter. There are two kinds of peritoneal dialysis: Continuous Ambulatory Peritoneal Dialysis (CAPD) Automated Peritoneal Dialysis (APD) The basic treatment is the same for each. However, the number of treatments and the way the treatments are done make each method different. CAPD is "continuous," machine-free and done while you go about your normal activities such as work or school. You do the treatment by placing about two quarts of cleansing fluid into your belly and later draining it. This is done by hooking up a plastic bag of cleansing fluid to the tube in your belly. Raising the plastic bag to shoulder level causes gravity to pull the fluid into your belly. When empty, the plastic bag is removed and thrown away. When an exchange (putting in and taking out the fluid) is finished, the fluid (which now has wastes removed from your blood) is drained from your belly and thrown away. This process usually is done three, four or five times in a 24-hour period while you are awake during normal activities. Each exchange takes about 30 to 40 minutes. Some patients like to do their exchanges at mealtimes and at bedtime. APD differs from CAPD in that a machine (cycler) delivers and then drains the cleansing fluid for you. The treatment usually is done at night while you sleep. What kind of peritoneal dialysis is best? The type of peritoneal dialysis that is best for you depends on your personal choice and your medical condition. Your doctor will help you to choose the one that is best for you. What are the pros and cons about being on peritoneal dialysis? Some doctors feel that CAPD and APD have several benefits when compared to hemodialysis. With continuous dialysis, you can control extra fluid more easily, and this may reduce stress on the heart and blood vessels. You are able to eat more and use fewer medications. You can do more of your daily activities and it is easier to work or travel.
- 17. 17 However, there are some people for whom peritoneal dialysis may not be appropriate. The abdomen or belly of some people, particularly those who are morbidly obese or those with multiple prior abdominal surgeries, may make peritoneal dialysis treatments difficult or impossible. Peritonitis (infection of abdomen) is an occasional complication although should be infrequent with appropriate precautions. When making a decision about the type of treatment, you should take into consideration that peritoneal dialysis is usually a daily process, similar to the working of the kidney and may be more gentle with fluid removal from the body. Peritoneal dialysis is an effective form of dialysis, has been proven to be as good as hemodialysis. Peritoneal dialysis is not for everyone. People must receive training and be able to perform correctly each of the steps of the treatment. A trained helper may also be used. How are treatments paid for? All types of dialysis are expensive, but, for most patients, the federal government now pays 80 percent of all dialysis charges, while private insurance or state medical assistance pays the rest. 5. Dialysis physicochemical principles Anatomy of the peritoneum The peritoneal membrane is a semi-permeable membrane that lines the abdominal wall (parietal peritoneum) and covers the abdominal organs (visceral peritoneum). The membrane is a closed sac in males. The fallopian tubes and ovaries open into the peritoneal cavity in females. The size of the membrane approximates the body surface area (1-2 m2). There are about 100 cc of transudate that is contained in the cavity in normal individuals. A. Blood Supply The parietal peritoneum derives its blood supply from the arteries in the abdominal wall. This blood drains into the systemic circulation. The visceral peritoneum is supplied by blood from the mesenteric and coeliac arteries which drain into the portal vein. B. Lymphatics Subdiaphragmatic lymphatics are responsible for 80% of the drainage from the peritoneal cavity. The drainage is then absorbed into the venous circulation through the right lymph duct and the left thoracic lymph duct. A balance of solutes and fluid in the interstitial tissue is maintained by absorption of fluid from the peritoneal cavity. The average lymphatic rate of absorption in the PD patient is 0.5-1.0 ml/min. Factors that affect the rate of absorption are respiratory rate, posture, and intra-abdominal pressure. Physiology of the Peritoneum The peritoneal membrane is a complex heterogenous, semi-permeable membrane with multiple pores. The early models of peritoneal membrane transport included multiple sites of resistance to the flow of solutes across the membrane. These included the capillary fluid film overlying the capillary endothelium, the capillary endothelium per se, the endothelial basement membrane, the interstitium, the mesothelial cells and the fluid overlying the peritoneal membrane. Newer concepts such as the Three Pore Model suggest that the
- 18. 18 major resistance to peritoneal transport is in the capillary endothelium and its basement membrane. The Three Pore Model is a theoretical model validated by clinical observations1,2. It suggests that the peritoneal capillary is the critical barrier to trans-peritoneal transport. Solute and water transport across the peritoneal capillary is mediated by pores of three different sizes. Large pores (100-200 A) exist in small numbers and constitute < 0.1% of all pores. The transport macromolecules and anatomically are identified as clefts between endothelial cells. Small pores (40-60 A) are more numerous and believed to transport small solutes and water. Ultra-small or transcellular pores (4-6 A) are water channels or aquaporin-1. They are numerous and resemble the water channels present in red blood cells and renal
- 19. 19 proximal tubules. They transport water only (sieving) and are present in the endothelial cells of the peritoneal capillaries. During ultrafiltration in PD, and unlike HD, solutes do not move across the membrane in direct proportion to their concentration in blood. Sodium is held back or sieved at the aquaporin barrier while water moves through. Sieving makes ultrafiltration a less effective form of convective solute transport. Click image to enlarge The semi-permeable peritoneal membrane allows solutes and water to be transported from the vascular system to the peritoneal cavity and vice versa through diffusion. Diffusion is the process of solutes moving from an area of higher concentration to an area of lower concentration, which is the case when dialysate is instilled into the peritoneal cavity. Actually, solutes move randomly in both directions, but there is simply more solute moving from the high to low concentration side than in the opposite direction. Eventually, the concentrations become equal on both sides of the membrane. This is termed equilibrium. The movement of solute molecules is random and driven by thermal energy. This energy is proportional to absolute temperature (degrees Centigrade above -273). This thermal energy is transferred to kinetic energy which is the multiple of mass and velocity. Since this energy is the same for different sized molecules at the same temperature, the larger molecules must move more slowly in order to have the same energy as the smaller molecules. Thus, the diffusive rate depends on molecular weight.
- 20. 20 Solute transport is influenced by the membrane permeability and size, characteristics of the solute, the volume of dialysate instilled, and blood flow to the membrane. Solute transport can be increased by maximizing the contact of dialysis solution with the membrane by placing the patient in a supine position or increasing the exchange volume. Osmosis is the movement of water across a semi-permeable membrane from an area of low solute concentration to an area of high solute concentration. The hydrostatic pressure gradient and the osmotic gradient between the blood and the dialysis solution influence osmosis. Click image to enlarge Increasing the dextrose concentration of dialysis solution enhances fluid removal by increasing the osmotic gradient between the plasma and the peritoneal fluid. The higher the dextrose concentration, the higher the fluid removal. The osmotic gradient is always greatest at the beginning of the dialysis exchange. As osmotic equilibration is achieved, the gradient decreases. Some reabsorption of fluid occurs when dialysate dwells beyond the point of equilibration. Alternatively, a glucose polymer can be used instead of glucose. The polymer is not absorbed, so the fluid removal is sustained. This process is called colloid osmosis. Click image to enlarge There is a significant amount of protein lost in dialysate. The amount lost varies from patient to patient but averages between 5-8 gm/day. Protein loss stabilizes and remains relatively constant unless the patient experiences peritonitis, then the protein loss increases during the infection. It is very important that protein intake be adequate in the PD patient. Daily protein requirements average 1.2-1.5 gm/kg of body weight. Other substances lost in dialysate are amino acids, water-soluble vitamins, hormones and some medications. Substances that are absorbed from dialysis solution into the systemic circulation include dextrose and calcium. The increased concentration of dextrose in dialysis solution causes dextrose to move into the systemic circulation.
- 21. 21 The major factor influencing the systemic calcium absorption is the amount of ionized calcium in the plasma and in the dialysis solution. A calcium concentration of 0.8 mmol/L in dialysis solution provides an ionized calcium of 1.6 mmol/L. Half of a standard serum calcium level of 2.20 - 2.58 mmol/L is ionized when the serum albumin is normal. Thus, with an ionized calcium in dialysis solution of 1.6 mmol/L and an ionized serum calcium of 1.0 mmol/L, calcium can be absorbed into the systemic circulation. 6. Peritoneal Access Successful peritoneal dialysis technique will depend largely peritoneal good access , since a catheter operating properly and smoothly peritoneal access will ensure the survival of the dialysis technique . Improvements in this dialysis therapy are associated with advances in catheter design and implementation methods there of. These advances are due to Palmer and Quinton , creators of the modern peritoneal catheter. This tubular silicone catheter with multiple perforations distal was refined by Tenckhoff and Schecter in 1968 , who improved the design . Thus, the distal part could be straight or curled , the newest being the placement of two sleeves bioincompatible material to cause severe fibrotic reaction . Thus getting hold the catheter to the abdominal wall , preventing the passage of microorganisms around the catheter. Good access peritoneal must have the following characteristics Easy deployment and removal biocompatible material Resistant to bacterial colonization Provide high flows without pain Not deteriorate with time Let the normal function of the abdominal wall Do not change too much aesthetics Easy Care and Handling minimum maintenance No displacements Minimize complications Catheters The catheter is a soft tube and consistent , peritoneal cavity communicating with the outside , creating a unnatural entrance to this cavity. Portions of the catheter are three: intraperitoneal, intramural (subcutaneous ) and externally. Types of catheters The types of catheters are divided according to three characteristics : design, material and number of sleeves . According to the design include: straight , coiled intraperitoneal portion and intramural part cauldron handle and gooseneck. For the material: silicone and polyurethane. And they may have one or two sleeves . The straight Tenckhoff catheter one or two sleeves has been widely used . Their placement is easy. Today it tends to place catheters other design in order to improve the hydraulic function , and also flows to perform the bore outlet , the inlet flow to the catheter into the abdominal cavity . Another widely used type of catheter is the one with the coiled intraperitoneal and intramural part swan neck , forcing an exit flow in the skin , thus facilitating better hole cleaning . The polyurethane catheter Cruz has advantages and disadvantages compared to silicon : design and faster flows , but is thermolabile and is damaged most antiseptics. The intraperitoneal curl nuisance prevents high flows .
- 22. 22 The catheter implantation The peritoneal catheter to implant while an expert who knows the operation of the peritoneal dialysis. Since the peritoneal catheters placed both surgeons and nephrologists , the classification of surgical implantation techniques and medical information may be inaccurate , but for educational purposes we maintain this rating. Either maximum require aseptic techniques . Surgical Technique This technique could call her open technique of catheter implantation , since it is made by planes dissection with a 5 cm incision in skin, abdominal wall and peritoneum. Through this opening the catheter is introduced and subsequently becomes layered closure . This technique should be done in the operating room and is recommended in the situations described below , to avoid complications during implantation. Previous abdominal surgery Widespread abdominal infection prior Existence of abdominal adhesions Recurrent peritonitis and torpid Harnessing surgery for another reason Need Omentectomy On the patient's wishes The medical technology This technique of implementation is a blind , puncture , necessitating dissection of skin and subcutaneous tissue . From the rectus fascia addresses the peritoneal cavity with the new trocars , as the Y- TEC system , then the catheter with a guide . The approach to the peritoneal cavity is blind , but prior to the introduction of the catheter if available you can view laparoscope peritoneal cavity , enabling more security situations in recommending the surgical technique . From here you try calling laparoscopic technique. This method of introducing the catheter is increasingly widespread due to the advantages of the surgical technique . The disadvantage of this mixed technique (percutaneous , subcutaneous dissection , blind , laparoscopic ) is the probability of intestinal loop click on the other hand act difficult if the intestinal loop is not attached to the parietal peritoneum puncture area . Medical technical description The patient must have previous training with the following steps: Give laxatives and / or enemas for bowel Shower or body wash fasting antibiotic analgesia sedation Bladder Emptying Wash with Betadine mask Lying with head slightly elevated After general analgesia and sedation with midazolam , infiltrate skin and subcutaneous tissue with local anesthetic and epinephrine in a 2 cm from the umbilicus , and lateral flow . Dissect skin and subcutaneous tissue to the fascia of the rectus . From here to the Y- TEC system addresses peritoneal cavity , making sure not to puncture the epigastric artery . Trocar is removed and if we do laparoscopy cannula also retired , leaving the sheath . With
- 23. 23 the stents increase the inlet to the peritoneal cavity , thereby facilitating introduction of the guide catheter and leave the internal dacron below the fascia . It checks the operation of the catheter with 500-1000 ml of dialysis solution . After verification of the proper functioning of the catheter are given points crown around the entrance hole in the abdominal wall . Depending on the type of catheter is made with the subcutaneous tunnel and the hole tunneling out of the catheter with a 4 mm punch , leaving the outer sleeve diameter of 2 cm from it. The variety introduced by Moncrief catheter burial for 20 days and then dig part of it, there is no data that provide the benefits of this technique. Catheter care in the postoperative period should be: the immobilization of the catheter, wound cures every 2-3 days , cleaning the hole , prophylactic antibiotic therapy for 1 week and periodic washing . Dialysis is the process of removing fluid and waste products from the body, a function usually performed by the kidneys, through artificial means. Two types of dialysis: hemodialysis and peritoneal dialysis. Peritoneal dialysis accomplishes the removal of waste and excess fluid by using the abdominal lining, called the peritoneal membrane, as a filter a membrane across which fluids and dissolved substances (electrolytes, urea, glucose, albumin and other small molecules) are exchanged from the blood. Peritoneal dialysis is similar in principle to hemodialysis. Both of these forms of renal replacement therapy depend upon the passive movement of water and dissolved substances (solutes) across a semipermeable membrane. This process is called diffusion. The direction of movement of solute is determined by the relative concentration on each side of the membrane, so that a substance goes from the side of greater to lesser concentration. Contraindication Peritoneal dialysis is contraindicated in patients withhypercatabolism because adequate clearance of uremic toxins cannot be achieved with this method of dialysis. Peritoneal adhesions and scarring are also contraindications. Caution should be used when prescribing peritoneal dialysis for patients with a history of ruptured diverticuli, respiratory disease, recurrent peritonitis (infection of the peritoneum), abdominal malignancies, severe vascular disease, back problems, and those who are obese. 7-Complication of the Peritoneal Dialysis Peritoneal dialysis (PD) is not always trouble-free. Patients may experience both psychological and physical problems, discussed below. Responsibility Some kidney patients get tired of the responsibility of doing their peritoneal dialysis every day. If this is a problem, talk to your peritoneal dialysis nurse who may be able to help you incorporate more flexibility into your routine. Body image Some peritoneal dialysis patients find it difficult to accept a permanent PD catheter. They worry that the catheter may affect their sexual activity and their relationship with their partner. Peritoneal dialysis nurses can help with tips on how to disguise the PD catheter. Peritoneal dialysis tends to stretch the abdomen, giving it a rounded appearance. Keeping fit and doing exercises to strengthen the abdominal muscles will help counteract this. PD nurses can give advice on suitable exercises. Fluid overload
- 24. 24 Fluid overload occurs when there is too much fluid in the body. It is characterised by a sudden increase in body weight, swollen ankles, and/or shortness of breath. Generally dialysis patients need to restrict their fluid intake to prevent fluid overload. Peritoneal dialysis patients, however, have more flexible fluid allowances than haemodialysis patients. Dehydration Dehydration occurs when there is too little fluid in the body. It can be caused by excess fluid loss due to diarrhoea or sweating. It is characterised by dizziness, feeling sick, or a sudden decrease in weight. Dehydration is far less common than fluid overload in dialysis patients. Discomfort Some PD patients find that having the dialysis fluid in their abdomen is uncomfortable. They feel full or bloated. Others suffer from backache or experience shoulder pain, especially when draining in or out. Very rarely, some patients experience discomfort when fresh fluid is drained in. Renal units can give advice on how to minimize or avoid discomfort. Poor drainage One of the most common problems with peritoneal dialysis, especially among new patients, is poor drainage of the dialysis fluid. The most common causes are: 1. Constipation - The pressure of the peritoneal dialysis fluid in the abdomen can cause movement of the bowel to slow down, increasing the likelihood of constipation. Constipation can cause the bowels to press against the catheter and interrupt drainage. It can also displace the catheter inside the peritoneal cavity. To avoid constipation, peritoneal dialysis patients may need to change their diet. In some cases, the patient's doctor may prescribe a laxative. 2. Catheter displacement - Sometimes the PD catheter moves into the wrong position. It may "float" back into the right place naturally. If not, a minor operation or manipulation under X-ray may be required to correct its position. Leaks In some patients, the peritoneal dialysis fluid leaks out around the catheter exit site. If this occurs, it may be necessary to decrease the volume of fluid in each exchange or stop peritoneal dialysis temporarily and have haemodialysis for a short period of time until the leak has resolved. Occasionally, it may be necessary to place a new catheter at a different site. In some people, fluid leaks into the genitals and causes swelling. In men, this is called scrotal leak. If this occurs, peritoneal dialysis must be temporarily stopped until the leak has healed and a period of temporary haemodialysis may be required. Exit-site infections An infected exit site is inflamed, red, sore, and discharges pus. It can be treated with antibiotics. Occasionally, the infection spreads inward, following the catheter tube along the "tunnel" through the abdominal wall. This type of infection is called a tunnel infection. If this occurs, it may be necessary to remove the catheter and put a new one in. A temporary period of haemodialysis may be required. Prevention of infections is extremely important. Patients need to follow the procedures covered during the initial PD training in order to care for their exit site. Good hygiene, and keeping the catheter taped down on the skin to protect the catheter, can significantly reduce the chances of getting an infection. Hernia A hernia is the protrusion of an organ (most commonly the bowel) through muscle wall, causing swelling. Sometimes a hernia may be undetected at the time a peritoneal catheter is
- 25. 25 put in. This may become a problem later as the constant pressure of dialysis fluid on the hernia may cause it to become bigger and painful. Surgery may be required to correct the problem. In some cases haemodialysis may be needed for a short time to allow healing after the operation. Alternatively, small volume PD exchanges may be recommended. Until patients have healed completely, they should not lift heavy objects. Peritonitis Peritonitis is an infection of the peritoneum, usually caused by bacteria entering through the catheter. This can happen when patients touch the open ends of the connections between the bag of dialysis fluid and the catheter. Sometimes, even though everything is kept clean, an infection can get into the abdomen from the outside. The chances of getting peritonitis are greatly reduced by following correct dialysis exchange procedures. Peritonitis infections are not that common. On average, patients can expect to get less than one attack of peritonitis every year. Some patients never get one. Peritonitis is easy to recognise. Dialysis fluid is normally clear. Peritonitis makes it cloudy. Some patients also experience abdominal pain and fever. Adding antibiotics to fresh dialysis fluid is the method of treatment. Some patients are shown how to do this at home. Occasionally, a patient may get several attacks of peritonitis in a row. When this happens, the PD catheter may need to be replaced and the abdomen 'rested' by not using peritoneal dialysis for 4 to 6 weeks. During this time, the patient usually needs to have haemodialysis until PD is resumed. Repeated attacks of peritonitis may damage the peritoneum and reduce the efficiency of the dialysis. If this happens, the patient will have to change to haemodialysis for long-term treatment. 8- Indication and Contraindications INDICATIONS Pediatric peritoneal dialysis can be used mainly in situations of renal failure, primary or secondary source (eg cardiac surgery ) and in other situations. Oligoanuria acute renal failure ( urine output less than 0.5 cc / kg / h ), which does not respond to diuretics and may be accompanied by positive balance : Hypervolemia hypertension HF pleural effusion anasarca Electrolyte disturbances and blood pH produced or not by acute renal failure : severe metabolic acidosis hyperkalemia , hypernatremia , hypercalcemia elevated BUN uremic encephalopathy ( accompanied by stupor, coma or convulsions) Hemolytic- uremic syndrome severe hypothermia Acute intoxication by toxic dialyzable through the peritoneum . (Table 1 : Types of toxic dialyzable through the peritoneum ) It is considered that when it is dialyzable toxic water soluble and has little affinity for plasma proteins . Soluble toxic or they bind tightly to plasma proteins are not adequately dialyzed by this method TOXIC non-dialysable TOXIC dialyzable
- 26. 26 CONTRAINDICATION No absolute contraindications , but will particularly value your choice in case of: Alterations in the integrity of the wall ( omphalocele , gastroschisis ... ) Diaphragmatic hernia or diaphragm or fistula surgery pleuro -peritoneal or intraperitoneal Recent abdominal surgery Infection or abdominal wall cellulitis peritonitis Severe intraperitoneal hemorrhage Massive or rapid catabolism poisoning (not recommended because dialysis acts more slowly ) Patients in shock 9.The Type Of Dialysis There are two types of peritoneal dialysis: Continuous ambulatory peritoneal dialysis (CAPD) .With CAPD, dialysate is instilled into and drawn out of the abdominal cavity by gravity alone. No machine is needed. The dwell time for CAPD ranges from four to 10 hours. The CAPD patient usually performs four exchanges per day, including an eight-hour overnight dwell. This continuous exchange most closely resembles normal renal function, and it is also convenient because the exchanges can be performed anywhere since no equipment is required Automated peritoneal dialysis (APD). with APD there are three different scheduling methods, including : 1. continuous cyclic peritoneal dialysis (CCPD), 2. intermittent peritoneal dialysis (IPD), and 3. nightly peritoneal dialysis (NPD). Description Before peritoneal dialysis begins, patients have a catheter surgically inserted into their peritoneal cavity. The catheter is usually placed 1.2–2 in (3–5 cm) below the umbilicus. When dialysis is ready to begin, a bag of fluid (dialysate) containing sterile water, normal plasma, electrolytes, and glucose is infused into the abdominal cavity. The volume of dialysate used can range from1.5–3 qt (1.5–3 l), and the concentration of electrolytes and glucose is altered according to what the physician prescribes. The dialysate is left in the abdominal cavity for anywhere from one hour to 10 hours, depending on the type of dialysis. The period of time that the dialysate is left in the abdominal cavity is called the dwell time. At the end of the prescribed dwell time, the dialysate is drained out of the abdominal cavity through the catheter. The drained dialysate takes waste products with it. This process of instilling a bag of dialysate, dwell time, and emptying the dialysate is called an exchange. The amount and timing of exchanges performed by patients depends on the type of dialysis, the recommendation of the physician, and the lifestyle of the patient. Peritoneal dialysis works based on the principles of osmotic pressure and diffusion. Osmotic pressure is the moving of fluid toward the solution with a higher solute concentration. Diffusion is the passing of particles from an area of high concentration to an area of lower concentration. The dialysate infused into the abdominal cavity is prepared with specific concentrations of electrolytes and glucose that will draw the waste products and excess fluid across the peritoneal membrane using diffusion and osmotic pressure. The pores in the peritoneal
- 27. 27 membrane are large enough to allow the waste to pass through into the abdominal cavity, but small enough that blood cells and other protein molecules are unable to pass through The Type Of Dialysis There are two types of peritoneal dialysis: Continuous ambulatory peritoneal dialysis (CAPD) .With CAPD, dialysate is instilled into and drawn out of the abdominal cavity by gravity alone. No machine is needed. The dwell time for CAPD ranges from four to 10 hours. The CAPD patient usually performs four exchanges per day, including an eight-hour overnight dwell. This continuous exchange most closely resembles normal renal function, and it is also convenient because the exchanges can be performed anywhere since no equipment is required Automated peritoneal dialysis (APD). with APD there are three different scheduling methods, including : 4. continuous cyclic peritoneal dialysis (CCPD), 5. intermittent peritoneal dialysis (IPD), and 6. nightly peritoneal dialysis (NPD). 10.Nursing Care and Management General Peritoneal Information Hand Hygiene In order to help stop the spread of bacteria in the unit please carefully wash your hands or use hand sanitizer before entering the unit and after leaving.This will help keep you and keep all of our patients healthy. Food & Drinks Eating on dialysis is not recommended because it can cause a drop in blood pressure and seriously affect your treatment. Some people may wish to bring a healthy snack to eat when treatment is over. Your renal dietician can provide more information about suitable snacks. Bathroom Breaks It is best to train your body to have bowel movements before your treatment. The need to go for a bowel movement while on dialysis can have serious, harmful effects during your treatment by affecting blood pressure. Washrooms are available to use before and after treatment. If you really need to go while receiving dialysis a bedpan will be provided. If you are having constant issues with constipation or diarrhea, make sure to talk to your doctor or nurse. Predialysis: Give physical and psychological preparation to the patient Check you have signed the consent form Although Patient Take SV Urination Helping PVC catheter insertion: ECG monitoring can also be used Rinse the tubing with dialysis solution Leave the patient comfortable in a supine position TRANS DIALYSIS: Optimizing patient comfort during dialysis (implement physical comfort measures, keep the patient in regard to their development and results) Provide care as whole person
- 28. 28 Keep management and dialysis fluid drainage Using strict aseptic techniques when you add the solution or drain emptied containers Measure SV. NOTAS Catéter Permanente: Tenckhoff ,Swan ,Cruz Duración: DP = 36 – 48 hrs HD = 6 – 8 hrs Farmacología: Heparina: Prevención de coágulos de fibrina el catéter y oclusión KCL tratamiento Hipocaliemia LABORATORIO TP ( tiempo de protrombina) = 11 – 13 seg ( factor de la goagulación) TPT = Tiempo parcial tromboplastina = 25 – 35 seg The nursing care in Dialysis Pediatric Us record every child's vital signs before starting the first infusion Check the heater maintains the liquid (37 ° C) (Figure 10: Heater dialysis). Peritoneal dialysis cycles tend to have a generally lasts 60 minutes, during which the dialysis fluid is infused under gravity for the first 20 minutes, the peritoneal cavity remains in another 20 minutes and allowed to leave for the remaining 20 minutes. These times of entry, stay and departure can be adjusted by the physician according to the needs of each child. We note that increasing the residence time increases the risk of hyperglycemia by absorption of dialysate glucose. A liquid inlet too suddenly may cause effects on hemodynamic and ventilatory child, plus it can cause pain. The volume of liquid in each pass infuse is prescribed by the doctor, and usually between 30-50 cc / kg (maximum 2 liters). It is advisable to start early and 10cc/kg cycles within 24-48 hours not exceeding 20 cc / kg, to reduce the risk of hemodynamic compromise. (Photo 11: dispensing burette) It is advisable that the first exchange not remain in the peritoneal cavity set 20-30 minutes, but the drenaremos immediately. This will check if a blood vessel is injured. To facilitate entry of the liquid and the drained, keep the child lightly built. The liquid should be clear and colorless. It is relatively common for the principle is slightly bloody. In this case, will have to monitor the patient's analytical (hematocrit and coagulation) and fibrin formation which could clog the orifices Tenckhoff catheter. If the fluid is brown or brown, sospecharemos a possible perforation of the colon If urine is similar to and has the same glucose concentration than this, bladder perforation sospecharemos possible. If the liquid is cloudy, sospecharemos possible infection. We will schedule valuation and all vital signs, or whenever necessary if respiratory and hemodynamic status is unstable. Will value, and record on the sheet of dialysis the following: dialysate composition (will note any changes in the composition which is required along the process) cycle start time amount of fluid infused
- 29. 29 infusion time residence time and / or Check Out volume and characteristics of fluid drained balance schedule balance accumulated in 24 hours Water will do a strict control of the patient, recording all income (intravenous, oral or enteral ...) and losses (diuresis, gastric drainage, surgical drains ...), to take stock accumulated as accurate as possible. Daily weights if the situation permits Value the presence of pain and discomfort Analytical control: during the first 24 hours blood tests will be performed every 4-8 hours, to evaluate mainly glucose and serum potassium and other electrolytes and osmolality. day is necessary to know the state of coagulation, hematology and renal function Daily will collect a sample of peritoneal fluid for cell count (to assess the presence of erythrocytes), biochemistry (especially protein) and perform bacteriological culture (in order to make possible early detection of infection). The dialysis system was completely replaced every 72 hours. The change is made sterile technique, the same way as the initial connection. We apply the appropriate care system and Tenckhoff catheter: find the existence of kinks or obstructions in the circuit, which hinder the infusion or drainage cure the catheter insertion site every 72 hours or whenever necessary (if soiled or wet) secure the catheter to the skin safely to prevent accidental extraction (apply approximation points or similar) Pericatheter protect the skin, keeping the dry zone and using protective patches (Comfeel R type), and thus avoid the formation of pressure sores in the area which supports the Tenckhoff catheter. When the catheter is removed, we will send the tip to microbiology, together with a sample of peritoneal fluid dialyzed How to manage supplies In peritoneal dialysis, have a lot of supplies, including dialysis bags, connectors and masks. You need a wardrobe of 3 x 5 feet or wall space of 10 feet. The person who will bring supplies boxes, stack them where you want and rotate so you use the old before the new. You should keep track of their supplies and order new ones once a month. The dialysis bags can not be frozen nor should they be exposed to very hot and must be always dry. If kept in the basement or garage, it's best to stack them on a table to support them in the ground. Remember to use these bags every day, so keep them far away from the room where the treatment is carried out not convenient. How to control your care As you are the person in charge of their daily care, there are some things you learn to do to check how you are progressing. Among them: Pay attention to how you feel: You are the best judge of your energy level, the pace of your breathing, any pain or swelling. Record the amount of fluid in each exchange: Keep precise records of how much fluid treatment placed in each exchange in and going out. If you are removing all liquids (plus excess water) you should contact your nurse.
- 30. 30 Take your blood pressure: Measure and record your blood pressure to see if you are in the healthy range using a bracelet to take blood pressure. Keep track of your weight: You should weigh yourself every day, using the same thing to see if you are taking enough fluids. Get monthly blood tests: Your doctor will order blood tests to measure things like potassium and phosphorus in your blood and to determine if you are getting adequate peritoneal dialysis. Collect urine for analysis: You can collect all of your urine for 24 hours in a refrigerated jar and bring it to the center. The Residual Renal Function test measures how well your kidneys yet. In the first year with PD, this test should be performed every 2 months. Raise dialysate for testing: A few times a year your doctor will ask you to bring some or all of dialysate used to perform a peritoneal equilibrium test (PET, for its acronym in English). You must enter the center and make a series of exchanges, then do you draw a blood sample. The PET help to know how long to leave the fluid in your abdomen for best results. Addressing the unexpected Unexpected events that may have to deal with quite possibly should be an infection or a problem with the catheter or cycler. In their training, learn how to act when signs of infection in your catheter at the exit of the catheter or peritoneum. Call your doctor or nurse immediately if you experience: Pus, redness or swelling or if you have pain around your catheter exit or in your abdomen. Signs of an infection of the peritoneum is a murky drainage bag, abdominal cramps, pain or fever. A lump in the abdomen or pelvic area can mean a possible separation in the muscle wall (hernia). Some events that are not emergency in PD can be quite alarming though probably not harmful: A crack or break in the catheter or transfer set can leave you vulnerable to infections. If this happens, close the catheter over the crack with the clamp in the training given. Then, call your nurse or doctor. There may be blood if a small blood vessel ruptures within your peritoneum. In women, there may be blood in the drainage bag every month or so during ovulation or during a menstrual period. Very occasionally this may be a sign of aortic aneurysm. If you are concerned, call your nurse or doctor. If you enter an air bubble in the peritoneum with dialysate fluid can have a severe shoulder pain. Do not worry! Your body will absorb the air. Ask your nurse about ways that exist to make sure all the air is out before making connections. If you feel pain during drainage, changing positions can help. You can also place the machine in an area higher or lower. Talk to your nurse about your options.
- 31. 31 ANNEXES: Table I: Composition of glucose-containing dialysis solutions. Dianeal® PD1 CAPD 2-4 Gambrosol trio 10® (Baxter) (Fresenius) (Gambro) Sodium 132 134 132 mmol/l Calcium 1.75 1.75 1.75 mmol/l Magnesium 0.75 0.5 0.25 mmol/l Chloride 102 103.5 96 mmol/l Lactate 35 35 40 mmol/l Glucose 13.6-38.6 15-42.5 15.2-38.8 g/l Osmolality 340-483 358-512 353-492 mOsm/l PH 5.5 5.5 6.5
- 32. 32 Table 2 Practice Exercise DP HOJA DE DIÁLISIS PERITONEAL Name of: Nº HISTORIA: FECHA: Composición líquido Hora entrada Volumen Entrada Tiempo Permanencia Volumen Salida Balance Balance Acumulado Dialisan 15,00 80 cc 20 ´ 90cc 0cc “ “ 16,00 80 cc 20 ´ 100 cc -20 cc -20cc “ “ 17,00 80 cc 20 ´ 110 cc -30 cc -50 cc Dialisan+ 20mEq ClK 18,00 80 cc 20 ´ 70 cc +10 cc -40 cc “ “ 19,00 80 cc 20 ´ 95 cc -15 cc -55 cc
- 33. 33 References 1. Atkins D, Best D, Briss PA et al. Grading quality of evidence and strength of recommendations. BMJ 2004; 328:1490 2. Guyatt G, Gutterman D, Baumann MH et al. Grading strength of recommendations and quality of evidence in clinical guidelines. Chest 2006; 129: 174-181 3. Guyatt GH, Oxman AD, Vist GE et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008; 336:924-926 4. Guyatt GH, Oxman AD, Kunz R et al. GRADE: going from evidence to recommendations. BMJ 2008; 336: 1049-1051 5. Guyatt GH, Oxman AD, Kunz R et al. GRADE: Incorporating considerations of resources use into grading recommendations. BMJ 2008; 336:1170-1173 6. Jaeschke R, Guyatt GH, Dellinger P et al. Use of GRADE grid to reach decisions on clinical practice guidelines when consensus is elusive. BMJ 2008; 337:327-330 7. Uhlig K, MacLeod A, Craig J et al. Grading evidence and recommendations for clinical practice guidelines in nephrology. A position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int 2006; 70:2058-2065 8. Kidney Disease: Improving Global Outcomes. KDIGO clinical practice guidelines for the prevention, diagnosis, evaluation and treatment of Hepatitis C in chronic
