Here are the guideline-recommended treatment selection and sequencing strategies for TNBC:- For early-stage disease (stage I-III), the standard of care is anthracycline- and taxane-based chemotherapy as adjuvant or neoadjuvant therapy. This includes AC-T (doxorubicin, cyclophosphamide followed by paclitaxel or docetaxel) or TC (docetaxel and cyclophosphamide).- For patients who achieve a pathologic complete response (pCR) to neoadjuvant chemotherapy, postoperative chemotherapy is still recommended. For those who do not achieve a pCR, consideration can be given to adding carboplatin or immunotherapy to adjuvant therapy. - For
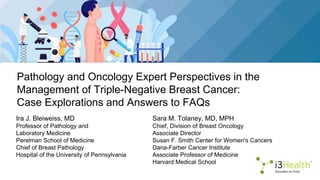
- 1. Pathology and Oncology Expert Perspectives in the Management of Triple-Negative Breast Cancer: Case Explorations and Answers to FAQs Ira J. Bleiweiss, MD Professor of Pathology and Laboratory Medicine Perelman School of Medicine Chief of Breast Pathology Hospital of the University of Pennsylvania Sara M. Tolaney, MD, MPH Chief, Division of Breast Oncology Associate Director Susan F. Smith Center for Women's Cancers Dana-Farber Cancer Institute Associate Professor of Medicine Harvard Medical School
- 2. Disclosures Ira J. Bleiweiss, MD No relevant financial relationships to disclose Sara M. Tolaney, MD, MPH Advisory board/panel: 4D Pharma, ARC Therapeutics, Artios, AstraZeneca, Bayer, BeyondSpring, Bristol Myers Squibb, Eisai, Genentech/Roche, Gilead, Incyte, Lilly, Menarini/Stemline, Merck, Myovant, Novartis, Pfizer, Reveal Genomics, Sanofi, Seagen, Umoja Biopharma, Zentalis, and Zymeworks Consultant: Aadi Bio, AstraZeneca, Blueprint Medicines, Bristol Myers Squibb, CytomX, Daiichi Sankyo, Eisai, Genentech/Roche, Gilead, Lilly, Menarini/Stemline, Merck, Novartis, OncXerna, Pfizer, Seagen, and Zetagen Grants/research support: AstraZeneca, Bristol Myers Squibb, Cyclacel, Eisai, Exelixis, Genentech/Roche, Gilead, Lilly, Merck, Nanostring, Novartis, OncoPep, Pfizer, Sanofi, and Seagen i3 Health has mitigated all relevant financial relationships
- 3. Learning Objectives TNBC = triple-negative breast cancer. Evaluate receptor and expression status for prognostication and treatment selection in TNBC Differentiate the pathological characteristics of the various types of TNBC Select optimal therapy for TNBC based on shared goals, biomarker testing, and clinical data on novel therapies Discuss strategies for timely recognition and mitigation of adverse events associated with novel TNBC therapies
- 4. Overview of TNBC: Epidemiology and Clinical Burden
- 5. Features of Triple-Negative Breast Cancer 10%-15% of all breast cancers Defined by immunohistochemistry Lacks expression of ER and PR, and low or no expression of HER2 Affected patients more often younger (<40 years old), Black May be associated with BRCA1 mutations and/or BRCA pathway dysfunction ER = estrogen receptor; PR = progesterone receptor; HER2 = human epidermal growth factor receptor 2. ACS, 2023.
- 6. TNBC Has Poorer Prognosis Than Other BC Subtypes BC = breast cancer. Foulkes et al, 2010; Dent et al, 2007; Gaedcke et al, 2007; Nofech-Mozes et al, 2009. High initial sensitivity to chemotherapy However, there are high relapse rates and higher likelihood of distant disease progression More aggressive visceral disease (liver, lung) Higher frequency of brain metastases TNBC recurrence peaks within the first 3 years after treatment The likelihood of distant recurrences postsurgery declines after 5 years The mean time to distant recurrence is approximately 2.4 years for TNBC compared with 4.4 years for ER+ patients Most deaths occur in the first 3-5 years
- 7. Testing Guidelines and Methods for Hormone (Estrogen/Progesterone) Receptors and HER2: a Pathologist’s View
- 8. What Is My Approach to Biomarker Testing? bx = biopsy. NCCN, 2023. Major pro: allows direct visual assessment of tumor by pathologist Currently: estrogen receptor/progesterone receptor (ER/PR) and HER2 assessed on every new invasive carcinoma (almost always core bx) Test multiple primaries? No, unless they have different histologies Test core bxs of lymph nodes? Yes, generally, but no guidelines I assess likelihood of positive staining based on tumor type, grade, patient age My goal: maximize chance of a positive stain, overcome heterogeneity – more likely for PR, less for ER, even less for HER2 Routine by Immunohistochemistry (IHC)
- 9. What Is My Approach to Biomarker Testing? (cont.) FISH = fluorescence in situ hybridization; chemorx = chemotherapy. NCCN, 2023; Allison et al, 2020; Wolff et al, 2023. Retest negative stains (ER, HER2) on surgical specimens Repeat testing on residual invasive tumor after neoadjuvant chemorx Current testing definition of triple-negative: Negative ER: <1% invasive tumor cells staining Negative PR: <1% invasive tumor cells staining Negative HER2: 0 or 1+ (weak staining), or 2+ with negative in situ hybridization (ISH) – note that a 2+ IHC result reflexively results in ISH testing, usually FISH Routine by IHC
- 10. But Things Are Rarely That Simple ASCO/CAP = American Society of Clinical Oncology/College of American Pathologists; RT-PCR = reverse transcriptase polymerase chain reaction. Hammond et al, 2010; Allison et al, 2020. After numerous prior changes in guidelines: 2010 ASCO/CAP guidelines: ER/PR+ if >1% tumor cells any staining. Meant to maximize antihormonal therapy, not missing patients However: this created a subclass of borderline ER cases, qualified for 21-gene testing, but 21-gene testing results often ER– by RT-PCR, meaning ? Most of these patients behaved like triple-negative Currently, 2019 ASCO/CAP guidelines created a new category, ER/PR low positive, if any intensity staining in 1%-10% of invasive tumor A Bit of ER/PR Guidelines History
- 11. Biomarker Testing: PD-L1 PD-L1 = programmed cell death ligand 1; met = metastasis. NCCN, 2023; Marletta et al, 2022. Non-bone distant metastatic triple-negative breast carcinoma: IHC testing for PD-L1, using antibody 22C3 Complicated interpretive guidelines, difficult to interpret, subjective: Staining of both tumor and inflammatory cells Often extreme intratumoral heterogeneity – overcome by staining one block from each available specimen: primary, lymph node met, distal met. Note: not validated on bone mets or on cytology Reflex Testing by IHC
- 12. What Are Caveats of Biomarker Testing? Taqi et al, 2018; Allison et al, 2020. Many factors can influence staining accuracy, including preanalytic: Time until formalin fixation Duration of formalin fixation Thickness and quality of tissue Decalcification method Staining platform used Interpretative: Invasive tumor only – sometimes difficult Semi quantitative % vs machine-read precise % Experience of interpreting pathologist Internal positive controls to assure valid test IHC
- 13. What Should the Pathology Report Include? Slide courtesy of Ira J Bleiweiss, MD. For ER/PR, should clearly state: Positive, low positive, or negative % cells staining and average stain intensity (0-3+) For HER2, should clearly state: Positive, equivocal, or negative with stain intensity (0-3+) Any ISH results: ratio of HER2 to normal control, average HER2 copy #/cell Presence or absence of adequate internal controls All above followed by required explanatory paragraph Biomarker Testing: Reporting
- 15. Pathology of TNBC Bleiweiss, personal communication, 2023; Amin et al, 2017; Handa et al, 2015. Important facts to be aware of: 1. ER status correlates strongly with nuclear grade of breast cancer, ie, little to no nuclear variation (lack of pleomorphism) = ER+ 2. Variability in nuclear size and shape tends to be ER– 3. Above depends also on age. Severe nuclear pleomorphism in older, postmenopausal patients may be ER+, while same in younger patients tends to be ER– 4. Since nuclear pleomorphism is a large determinant of grade, most triple- negative breast cancer is poorly differentiated duct (with exceptions to follow) Not Just 1 Type of Cancer
- 16. Pathology of TNBC (cont.) NOS = not otherwise specified. Images courtesy of Ira J. Bleiweiss, MD. Usual Type: Poorly Differentiated Duct, NOS ER–, PR–, HER2–
- 17. Pathology of TNBC (cont.) NOS = not otherwise specified. Images courtesy of Ira J. Bleiweiss, MD. Usual Type: Poorly Differentiated Duct, NOS Patch of ER positivity today would be called low positive
- 18. Pathology of TNBC (cont.) WT1 = Wilms' tumor gene 1. Images courtesy of Ira J. Bleiweiss, MD. Subtype: BRCA1 Mutation–Associated Patient With Breast and Ovarian Chronic inflammatory infiltrate, “medullary” features Breast Breast ER–, PR–, HER2–, WT1–
- 19. Pathology of TNBC (cont.) Images courtesy of Ira J. Bleiweiss, MD. Subtype: BRCA1 Mutation – Breast and Ovarian Ovarian primary, not metastatic breast, even higher grade Omentum Omentum-WT1 Omentum-ER
- 20. What are some unusual variants of TNBC to be aware of?
- 21. Pathology of TNBC (cont.) diff = differentiated. Images courtesy of Ira J. Bleiweiss, MD. Metaplastic Carcinoma: Duct + Squamous ± Sarcoma Chondrosarcoma Osteosarcoma Relatively chemo-resistant
- 22. Pathology of TNBC (cont.) Images courtesy of Ira J. Bleiweiss, MD. Rare Adenoid Cystic Carcinoma: GOOD Prognosis, Solid, Basaloid Variant-Worse
- 23. Pathology of TNBC (cont.) LGASC = low-grade adenosquamous. Images courtesy of Ira J. Bleiweiss, MD. Low-grade adenosquamous Rare Metaplastic GOOD Prognosis: Fibromatosis-Like, LGASC
- 24. Pathology of TNBC (cont.) Images courtesy of Ira J. Bleiweiss, MD. Special Rare Types: Secretory, Apocrine (Can Be HER2+)
- 25. What Are Caveats in the Pathology Report? Dx = diagnosis. Images courtesy of Ira J. Bleiweiss, MD. Min et al, 2013; Kim et al, 2011. Be very wary if pathology report reads: infiltrating well-differentiated duct carcinoma, ER–/PR–/HER2– Something is wrong – grade, staining, mixup, or diagnosis This core bx was called tubular carcinoma, triple-negative that does not exist Dx: microglandular adenosis Rare but benign
- 26. What Are Caveats in the Pathology Report? (cont.) Images courtesy of Ira J. Bleiweiss, MD. Marrazzo et al, 2020; Pareja et al, 2019; Kaur et al, 2022. Be very wary if pathology report reads: mucinous carcinoma, ER–/PR–/HER2– Something is wrong – grade, staining, mixup, or diagnosis Possible dx: invasive micropapillary and mucinous carcinoma or (rare) mucinous cystadenocarcinoma Remember: triple-negative breast cancer should be poorly diff with pleomorphic nuclei
- 27. What are the guideline- recommended treatment selection and sequencing strategies for TNBC?
- 28. How Do BC Subtypes Compare for Survival? Howlader et al, 2018; Bauer et al, 2007. TNBC is associated with shorter overall survival compared with other subtypes despite anthracycline + taxane therapy
- 29. Can we improve outcomes by adding immunotherapy?
- 30. Combining Checkpoint Inhibition With Chemotherapy Slide courtesy of Sara Tolaney, MD. Rationale for Combining Pembrolizumab With C Chemotherapy results in: Pembrolizumab chemotherapy pCR=pathologic complete response as defined as ypT0/Tis ypN0; TNBC=triple-negative breast cancer; PAC=paclitaxel, doxorubicin, cy Tumor lysis and antigen sheddinga PD-L1 expressiond KN173 (N=60 0 20 40 60 80 100 Before chemo After chemo PD-L1+ PD-L1+ 0 10 20 30 40 50 60 70 Pembro + T/AC ± pCR rate, %
- 31. KEYNOTE-355: Study Design Pembrolizumab + Chemotherapy for Advanced, Metastatic TNBC Patient Eligibility Criteria: • Age ≥18 years • Central determination of TNBC and PD-L1 expression • Previously untreated locally recurrent inoperable or metastatic TNBC • Completion of treatment with curative intent ≥6 months prior to first disease recurrence • ECOG performance status 0 or 1 • Life expectancy ≥12 weeks from randomization • Adequate organ function • No systemic steroids • No active CNS metastases • No active autoimmune disease R 2:1 Progressive disease/cessation of study therapy Stratification Factors: • Chemotherapy on study (taxane vs gemcitabine/carboplatin) • PD-L1 tumor expression (CPS ≥1 vs CPS <1) • Prior treatment with same class chemotherapy in the neoadjuvant or adjuvant setting (yes vs no) ECOG = Eastern Cooperative Oncology Group; CPS = combined positive score. Cortes et al, 2020. Pembrolizumab + Chemotherapy Placebo + Chemotherapy
- 32. KEYNOTE-355: PFS Analysis PFS = progression-free survival; ITT = intention to treat. Rugo, Cortez et al, 2021. PD-L1 CPS ≥1 PD-L1 CPS ≥10 ITT Pembrolizumab + Chemotherapy for Advanced, Metastatic TNBC Pembro
- 33. KEYNOTE-355: Overall Survival at PD-L1 CPS ≥10 Rugo, Cortez et al, 2021. Pembrolizumab + Chemotherapy for Advanced, Metastatic TNBC n/N Events HR (95% CI) P-value (one-sided) Pembro + Chemo 155/220 70.5% 0.73 (0.55-0.95) 0.0093* Placebo + Chemo 84/103 81.6% 58.3% 44.7% 23.0 months 16.1 months 48.2% 34.0% 0 3 6 9 12 15 18 21 24 27 30 33 36 39 42 45 48 51 54 0 10 20 30 40 50 60 70 80 90 100 Time, months Percentage of Patients No. at risk 220 214 193 171 154 139 105 127 116 103 98 91 77 66 55 35 46 39 91 84 78 73 30 25 22 22 59 17 43 31 17 6 12 8 2 0 2 0
- 34. Pembrolizumab for TNBC AEs = adverse events; Pbo = placebo. Schmid et al, 2021. Immune-Mediated AEs and Infusion Reactions in Combined Phases
- 35. What about strategies that target DNA repair?
- 36. Efficacy of PARP Inhibitors PARPi = poly ADP ribose polymerase inhibitor; gBRCA = germline BRCA; TPC = treatment of physician’s choice; mo = months; ORR = objective response rate; HR = hazard ratio; CI = confidence interval; BICR = blinded independent central review; carbo = carboplatin. Robson et al, 2017; Litton et al, 2018; Díeras et al, 2020. OlympiAD Olaparib vs TPC EMBRACA Talazoparib vs TPC BROCADE3 Veliparib/carbo/paclitaxel placebo/carbo/paclitaxel PFS 7.0 mo vs 4.2 mo HR=0.58 95% CI (0.43-0.80) 8.6 mo vs 5.6 mo HR=0.54 95% CI (0.41-0.71) 14.5 mo vs 12.6 mo HR=0.705 95% CI (0.56-0.88) ORR 59.9% vs 28.8% (n=100) (n=19) BICR assessment 62.6% vs 27.2% (n=137) (n=31) Investigator assessment 75.8% vs. 74.1% (n=216) (n=106) Investigator assessment Patients With gBRCA Mutations and Metastatic Breast Cancer Critical to obtain germline testing on all metastatic breast cancer patients to see if they could be a candidate for PARPi
- 37. Safety of PARP Inhibitors Robson et al, 2017; Litton et al, 2018; Díeras et al, 2020. OlympiAD Olaparib vs TPC EMBRACA Talazoparib vs TPC BROCADE3 Velaparib/carbo/paclitaxel vs placebo/carbo/paclitaxel Grade ≥3 adverse events 36.6% vs 50.5% Hematologic: 55% vs 38% Nonhematologic: 32% vs 38% Serious: 25.5% vs 25.4% 97% vs 96% Most common with PARPi Olaparib Anemia: 16.1% vs 4.4 Neutropenia: 9.3% vs 26.4% Fatigue: 2.9% vs 1.1% Transaminitis: 1.5%-2.4% vs 1.0%-0 Headache: 1.0% vs 2.2% Talazoparib Anemia: 39.2% vs 4.8% Neutropenia: 20.9% vs 34.9% Thrombocytopenia: 14.7% vs 1.6% Vomiting: 2.4% vs 1.6% Back pain: 2.4% vs 1.6% Dyspnea: 2.4% vs 2.4% Headache: 1.7% vs 0.8% Fatigue: 1.7% vs 3.2% Veliparib + carbo/paclitaxel Neutropenia: 81% vs 29% Thrombocytopenia: 40% vs 28% Anemia: 42% vs 40% Nausea: 6% vs 4% Fatigue: 7% vs 4% Peripheral neuropathy: 4% vs 5% Diarrhea: 5% vs 3% Leukopenia: 30% vs 28% Headache: 1% vs 2% Vomiting: 4% vs 2%
- 38. TBCRC 048: Olaparib for MBC Expanded MBC = metastatic breast cancer; PALB2 = partner and localizer of BRCA2; gPALM2 = germline PALB2; sBRCA = somatic BRCA; ATM = ataxia-telangiectasia mutated; CHEK2 = checkpoint serine-threonine kinase 2; PR = partial response; SD = stable disease. Tung et al, 2020a; Tung et al, 2020b. Benefit in gPALB2 + sBRCA PALB2 N=13 sBRCA1/2 N=17 ATM & CHEK2 N=17 Germline: 9/11 PR (82%) 10/11 had tumor regression; 1 SD > 1 year Somatic: 0/2 – both SD (limited assessments) 8/16 PR (50%) 0/13 germline 0/4 somatic New cohorts are beginning for gPALB2 and sBRCA1/2 breast cancer
- 39. What about strategies that use antibody-drug conjugates?
- 40. NCCN Guidelines Recommendation SG = sacituzumab govitecan; T-DXd = trastuzumab deruxtecan; MSI-H = microsatellite instability high; TMB-H = tumor mutational burden–high. NCCN, 2023. SG and T-DXd As the Preferred Choice for Second-Line TNBC NCCN Breast Cancer Guidelines Version 4.2023: HR– and HER2– TNBC Setting Subtype/Biomarker Regimen First line PD-L1 CPS ≥10 regardless of germline BRCA mutation status Pembrolizumab + chemotherapy (albumin-bound paclitaxel, paclitaxel, paclitaxel, or gemcitabine and carboplatin (Category (Category 1, preferred) PD-L1 CPS <10 and no germline BRCA1/2 mutation Systemic chemotherapy PD-L1 CPS <10 and germline BRCA1/2 mutation mutation • PARPi: olaparib, talazoparib (Category 1, preferred) • Platinum: cisplatin or carboplatin (Category 1, preferred) preferred) Second line Germline BRCA1/2 mutation • PARPi: olaparib, talazoparib (Category 1, preferred) Any • Sacituzumab govitecan (Category 1, preferred) • Systemic chemotherapy No germline BRCA1/2 mutation and HER2 IHC 1+ or 2+/ISH-negative Fam-trastuzumab deruxtecan-nxki (Category 1, preferred) Third line and beyond Biomarker-positive (ie, MSI-H, NTRK, RET, TMB-H) Targeted agents Any Systemic chemotherapy
- 41. Sacituzumab Govitecan (SG) Trop-2 = human trophoblast cell-surface antigen 2. Vidula et al, 2017; Ambrogi et al, 2014; Goldenburg & Sharkey, 2020; Nagayama et al, 2020; Cardillo et al, 2015; Goldenburg et al, 2015; FDA, 2021. Trop-2 is expressed in all subtypes of breast cancer and is linked to poor prognosis SG is distinct from other ADCs Antibody highly specific for Trop-2 High drug-to-antibody ratio (7.6:1) Internalization and enzymatic cleavage by tumor cell not required for the liberation of SN-38 from the antibody Hydrolysis of the linker also releases the SN-38 cytotoxic extracellularly in the tumor microenvironment, providing a bystander effect Granted FDA approval for metastatic TNBC A First-in-Class Trop-2‒Directed Antibody Drug Conjugate (ADC) Humanized anti‒Trop-2 antibody • Directed toward Trop-2, an epithelial antigen expressed on many solid cancers SN-38 payload • SN-38 more potent than parent compound, irinotecan Linker for SN-38 • Hydrolyzable linker for payload release • High drug-to-antibody ratio (7.6:1)
- 42. 1) Binding 2) Internalization 3) Intracellular trafficking 4) Lysosomal degradation 5) Cell cytotoxicity 6) Bystander effect • Rapid internalization and efficient release of the the SN-38 payload intracellularly in Trop-2– expressing cancer cells and extracellularly into the into the surrounding tumor microenvironment microenvironment • Before internalization of the ADC, the linker can be cleaved at the pH of the tumor microenvironment, releasing SN-38 payload outside the targeted tumor cell • DNA damage to the targeted cell and a bystander effect on adjacent tumor cells that may not express Trop-2 Endosome Lysosome Bystander effect 1 2 4 3 5 6 6 SG Tumor cell Tumor cell Cell death due to DNA damage SN-38 Topo 1 SG Is a First-in-Class Trop-2–Directed ADC Topo 1 = topoisomerase I. Rugo et al, 2020; Kopp et al, 2023. Concentrates SN-38 Payload Intracellularly and in the Surrounding Tumor Microenvironment
- 43. ASCENT: Phase 3 Confirmatory Study mTNBC = metastatic triple-negative breast cancer; IV = intravenous; OS = overall survival; DOR = duration of response; TTR = time to response; QOL = quality of life. Bardia et al, 2021; Bardia et al, 2020; Clinicaltrials.gov, 2022. Sacituzumab Govitecan in Second-Line and Later mTNBC Primary End Point • PFS for patients without brain metastases (BMNeg) Secondary End Points • PFS for the ITT population, OS, ORR, DOR, TTR, QOL, and safety Stratification factors • Number of prior chemotherapies (2 or 3 vs >3) • Geographic region (North America vs Europe) • Presence/absence of known brain metastases (yes/no) R 1:1 Metastatic TNBC • ≥2 chemotherapies, 1 of which could be in neo/adjuvant setting provided progression occurred within a 12- month period • Patients with stable brain metastasis were allowed (N=529) Sacituzumab govitecan 10 mg/kg IV Days 1 and 8, every 21 days (n=267) Treatment of physician’s choice (n=262) Continue treatment until progression or unacceptable toxicity
- 44. ASCENT: PFS and OS for BMNeg Patients Bardia et al, 2022. The ASCENT trial demonstrated statistically significant and clinically meaningful improvement in PFS and OS over single-agent chemotherapy in the primary study population Sacituzumab Govitecan in Second-Line and Later mTNBC BICR Analysis SG (n=235) TPC (n=233) No. of events 167 150 Median PFS, mo (95% CI) 5.6 (4.3–6.3) 1.7 (1.5–2.6) HR (95% CI), P value 0.39 (0.31–0.49), P<.0001 Analysis based on final database lock confirmed the improvement in clinical outcomes over TPC: • Median PFS of 5.6 vs 1.7 months (HR 0.39, P<0.0001) • Median OS of 12.1 vs 6.7 months (HR 0.48, P<0.0001) • OS rate at 24 months of 22.4% (95% CI: 16.8-28.5) vs 5.2% (95% CI: 2.5-9.4) Progression-free survival (BICR analysis) Overall survival SG (n=235) TPC (n=233) No. of events 173 199 Median OS, mo (95% CI) 12.1 (10.7–14.0) 6.7 (5.8–7.7) HR (95% CI), P value 0.48 (0.39–0.59), P<.0001
- 45. ASCENT: Response Rates (BMNeg and ITT Population) Bardia et al, 2022. Analysis based on final database lock confirmed the improvement in clinical outcomes over TPC: Objective response rate of 35% vs 5%, P<0.0001 Clinical benefit rate of 45% vs 9%, P<0.0001 Median duration of response of 6.3 (95% CI:5.5-79) vs 3.6 months (95% CI, 2.8-not evaluable) The clinical benefit of SG over TPC observed in the ITT population was consistent with that of the BMNeg population: Objective response rate of 31% vs 4%, P<0.0001 Clinical benefit rate of 40% vs 8%, P<0.0001 Median duration of response of 6.3 (95% CI:5.5-7.9) vs 3.6 months (95% CI:2.8-NE) Sacituzumab Govitecan in Second-Line and Later mTNBC SG (n=235) TPC (n=233) ORR, n (%) 82 (35%) 11 (5%) P value P<0.0001 Best overall response, n (%) Complete response 10 (4%) 2 (1%) Partial response 72 (31%) 9 (4%) Clinical benefit rate, n (%) 105 (45%) 20 (9%) P value P<0.0001 Median DOR, mo (95% CI) 6.3 (5.5-7.9) 3.6 (2.8-NE) Median TTR, mo (range) 1.5 (0.7-10.6) 1.45 (1.3-4.2)
- 46. Approved for patients with ≥2 systemic therapies, at least 1 of them for metastatic disease BICR Analysis SG (n=33) TPC (n=32) No. of events 21 23 Median PFS, mo (95%) CI 5.7 (2.6–8.1) 1.5 (1.4–2.6) HR (95% CI) 0.41 (0.22–0.76) BICR Analysis SG (n=33) TPC (n=32) No. of events 22 24 Median OS—mo (95% CI) 10.9 (6.9–19.5) 4.9 (3.1–7.1) HR (95% CI) 0.51 (0.28–0.91) Progression-free survival 100 PFS probability (%) 80 60 40 20 0 0 3 6 9 12 15 Time (months) SG TPC Censored 33 19 8 2 1 0 32 23 16 12 6 5 2 1 0 1 SG TCP 32 3 2 1 1 0 28 8 2 2 2 2 1 1 1 1 No. of patients still at risk Overall survival OS probability (%) 0 0 Time (months) 100 80 60 40 20 3 6 9 12 15 18 21 24 27 SG TPC Censored SG TCP No. of patients still at risk 33 29 26 19 13 9 7 1 0 3231 2826 2119 1715 1311 7 7 2 4 0 0 0 32 22 12 6 5 3 1 1 1 2927 1714 10 8 5 5 5 5 2 2 1 1 1 1 0 In patients with 2L mTNBC, PFS and OS improvement was consistent with the overall study population ASCENT: Sacituzumab Govitecan PFS and OS Carey et al, 2022.
- 47. Clinical Benefit With SG vs TPC H-score = histochemical score. Hurvitz et al, 2021. Irrespective of Level of Trop-2 Expression in Previously Treated mTNBC Trop-2 High; H-score: 200–300 Trop-2 Medium; H-score: 100–200 Trop-2 Low; H-score: <100 SG (n=85) TPC (n=72) SG (n=39) TPC (n=35) SG (n=27) TPC (n=32) Median PFS, mo (95% CI) 6.9 (5.8–7.4) 2.5 (1.5–2.9) 5.6 (2.9–8.2) 2.2 (1.4–4.3) 2.7 (1.4–5.8) 1.6 (1.4–2.7) Median OS, mo (95% CI) 14.2 (11.3–17.5) 6.9 (5.3–8.9) 14.9 (6.9–NE) 6.9 (4.6–10.1) 9.3 (7.5–17.8) 7.6 (5.0–9.6) Overall survival Progression-free survival 0 PFS probability (%) 100 80 60 40 20 Time (months) 0 5 10 15 20 25 OS probability (%) 100 80 60 40 20 Time (months) 0 5 10 15 20 25 Events/censored SG: Trop-2 High 60/25 SG: Trop-2 Medium 26/13 SG: Trop-2 Low 19/8 TPC: Trop-2 High 47/25 TPC: Trop-2 Medium 24/11 TPC: Trop-2 Low 24/8 Events/censored SG: Trop-2 High 53/32 SG: Trop-2 Medium 22/17 SG: Trop-2 Low 20/7 TPC: Trop-2 High 64/8 TPC: Trop-2 Medium 23/12 TPC: Trop-2 Low 25/7
- 48. ASCENT-03: Study Design (NCT05382299) PD-1 = programmed cell death protein 1; gem = gemcitabine; AUC = area under curve. Clinicaltrials.gov, 2023h. Sacituzumab Govitecan vs TPC for First-line PD-L1– mTNBC Crossover to SG allowed after BICR-verified disease progression Stratification Factors: • De novo vs recurrent disease within 6-12 months of treatment in the curative setting vs recurrent disease >12 months after treatment in the curative setting • Geographic region N=540 (≤25% de novo) Key Eligibility Criteria • Previously untreated, inoperable, locally advanced, or metastatic TNBC • PD-L1– tumors (CPS <10, IHC 22C3 assay) OR PD-L1+ tumors (CPS ≥10, IHC 22C3 assay) if treated with anti– PD-(L)1 agent in the curative setting • ≥6 months since treatment in curative setting • Prior anti–PD-(L)1 agent allowed in the curative setting • PD-L1 and TNBC status centrally confirmed Treated until BICR- confirmed progression or unacceptable toxicity Long-term follow-up Sacituzumab Govitecan 10 mg/kg IV on Days 1 and 8 of 21-day cycles TPC Chemotherapy Gem + carbo: gem 1,000 mg/m2 with carbo AUC 2 IV on Days 1 and 8 of 21-day cycles Paclitaxel: 90 mg/m2 IV on Days 1, 8, and 15 of 28-day cycles Nab-paclitaxel: 100 mg/m2 IV on Days 1, 8, and 15 of 28-day cycles R 1:1
- 49. ASCENT-04: Study Design (NCT05382286) Clinicaltrials.gov, 2023g. SG + Pembro vs TPC + Pembro First-Line PD-L1+ mTNBC Key Eligibility Criteria • Previously untreated, inoperable, locally advanced, OR metastatic TNBC • PD-L1+ (CPS ≥10, IHC 22C3 assay) • PD-L1 and TNBC status centrally confirmed • ≥6 months since treatment in curative setting SG + Pembrolizumab (Pembro) SG: 10 mg/kg IV on Days 1 and 8 of 21-day cycles Pembro: 200 mg IV on Day 1 of 21-day cycles TPC Chemotherapy + Pembro Pembro dosed as above TPC: gem 1,000 mg/m2 with carbo AUC 2 IV on Days 1 and 8 of 21-day cycles OR paclitaxel 90 mg/m2 IV on Days 1, 8, and 15 of 28-day cycles OR nab-paclitaxel: 100 mg/m2 IV on Days 1, 8, and 15 of 28-day cycles Long-term follow-up Treated until BICR- confirmed progression or unacceptable toxicity Crossover to SG allowed after BICR-confirmed progression Stratification factors: • De novo vs recurrent disease within 6–12 months of treatment in the curative setting vs recurrent disease >12 months after treatment in the curative setting • Geographic region (US/Canada vs rest of world) • Prior exposure to anti-PD-(L)1 therapy N=440 R 1:1
- 50. HER2 IHC examples HER2+ HER2-low HER2– 34% to 63% of breast cancer patients considered HER2– under current guidelines express low levels of HER2 Prevalence of HER2-Low by HR Status Schettini et al, 2020. IHC 0 IHC +1 IHC +2 HR+ Disease N=2,485 TNBC N=620 IHC 0 37% IHC +1 46% IHC +2 17% IHC 0 66% IHC +1 26% IHC +2 8% HER2–
- 51. Trastuzumab Deruxtecan (T-DXd) Modi et al, 2022a. Structure and Mechanism of Action Internalization of T-DXd leads to release of the DXd payload and subsequent cell death in the target tumor cell and neighboring tumor cells through the bystander effect
- 52. DESTINY-Breast04: First Randomized Phase 3 Study Q3W = every 3 weeks. Modi et al, 2022b. Trastuzumab Deruxtecan for HER2-Low MBC Stratification factors • Centrally assessed HER2 status (IHC 1+ vs IHC 2+/ISH–) • 1 versus 2 prior lines of chemotherapy • HR+ (with vs without prior treatment with CDK4/6 inhibitor) versus HR– HR+ ≈ 480 HR– ≈ 60 R 2:1 Primary end point • PFS by BICR (HR+) Key secondary end points • PFS by BICR (all patients) • OS (HR-positive and all patients) Key Eligibility Criteria • HER2-low (IHC 1+ vs IHC 2+/ISH-– ), unresectable, and/or MBC treated with 1-2 prior lines of chemotherapy in the metastatic setting • HR+ disease considered endocrine refractory T-DXd 5.4 mg/kg Q3W (n=373) TPC Capecitabine, eribulin, gemcitabine, paclitaxel, nab-paclitaxel (n=184)
- 53. DESTINY-Breast04: PFS in HR+ and All Patients Modi et al, 2022a; Modi et al, 2022b. Trastuzumab Deruxtecan for HER2-Low MBC 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 0 20 40 60 80 100 Progression-Free Survival Probability (%) Months No. at Risk 373 365 325 295 290 272 238 217 201 183 156 142 118 100 88 81 71 53 42 35 32 21 18 15 8 4 4 1 1 0 184 166 119 93 90 73 60 51 45 34 32 29 26 22 15 13 9 5 4 3 1 1 1 1 1 1 0 T-DXd (n = 373): TPC (n = 184): HR+ No. at Risk 331 T-DXd (n = 331): 324 290 265 262 248 218 198 182 165 142 128 107 89 78 73 64 48 37 31 28 17 14 12 7 4 4 1 1 0 163 TPC (n = 163): 146 105 85 84 69 57 48 43 32 30 27 24 20 14 12 8 4 3 2 1 1 1 1 1 1 0 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 Months 0 20 40 60 80 100 Progression-Free Survival Probability (%) T-DXd mPFS: 10.1 mo TPC mPFS: 5.4 mo Hazard ratio: 0.51 95% CI: 0.40-0.64 P< 0.0001 Δ 4.7 mo Hazard ratio: 0.50 95% CI: 0.40-0.63 P<0.0001 Δ 4.8 mo TPC mPFS: 5.1 mo T-DXd mPFS: 9.9 mo All Patients
- 54. DESTINY-Breast04: OS in HR+ and All Patients mOS = median overall survival. Modi et al, 2022a; Modi et al, 2022b. Trastuzumab Deruxtecan for HER2-Low MBC No. at Risk 331 T-DXd (n = 331): 325 323319 314 309 303 293 285 280 268 260 250 228 199 190 168 144 116 95 81 70 51 40 26 14 9 8 6 6 163 TPC (n = 163): 151 145143 139 135 130 124 115 109 104 98 96 89 80 71 56 45 37 29 25 23 16 14 7 5 3 1 0 2 1 1 1 0 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 Months 0 20 40 60 80 100 Overall Survival Probability (%) T-DXd mOS: 23.9 mo TPC mOS: 17.5 mo Hazard ratio: 0.64 95% CI: 0.48-0.86 P=0.0028 Δ 6.4 mo 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 Months 0 20 40 60 80 100 Overall Survival Probability (%) No. at Risk 373 T-DXd (n = 373): 366 363357 351 344 338 326 315 309 296 287 276 254 223 214 188 158 129 104 90 78 59 48 32 20 14 12 10 8 184 TPC (n = 184): 171 165161 157 153 146 138 128 120 114 108 105 97 88 77 61 50 42 32 28 25 18 16 7 5 3 1 0 3 1 1 1 0 T-DXd mOS: 23.4 mo TPC mOS: 16.8 mo Hazard ratio: 0.64 95% CI: 0.49-0.84 P=0.0010 Δ 6.6 mo HR+ All Patients
- 55. DESTINY-Breast04: Exploratory End Points Modi et al, 2022a; Modi et al, 2022b. Trastuzumab Deruxtecan for HER2-Low MBC 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 Months 0 20 40 60 80 100 Progression-Free Survival Probability (%) No. at Risk 40 T-DXd (n = 40): 39 33 29 28 25 21 20 19 18 13 13 11 11 10 8 7 5 5 4 4 4 4 3 1 0 18 TPC (n = 18): 17 11 7 6 4 3 3 2 2 2 2 2 2 1 1 1 1 1 1 0 T-DXd mPFS: 8.5 mo TPC mPFS: 2.9 mo Hazard ratio: 0.46 95% CI: 0.24-0.89 Δ 5.6 mo 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 Months 0 20 40 60 80 100 Overall Survival Probability (%) No. at Risk 40 T-DXd (n = 40): 39 38 37 36 34 34 32 31 30 28 27 26 26 23 23 19 14 13 9 9 8 7 7 6 6 5 4 4 18 TPC (n = 18): 17 16 14 14 14 3 11 10 8 8 8 7 6 6 5 5 5 5 3 3 2 2 2 0 T-DXd mOS: 18.2 mo TPC mOS: 8.3 mo Hazard ratio: 0.48 95% CI: 0.24-0.95 Δ 9.9 mo PFS OS PFS and OS in HR– Patients
- 56. 0 10 20 30 40 50 60 Percentage 3.6 Progressive disease, % Not evaluable, % Clinical benefit rate, % Duration of response, months 7.8% 21.1% 12.5% 33.3% 4.2% 12.7% 7.5% 5.6% 71.2% 34.3% 62.5% 27.8% 10.7% 6.8% 8.6% 4.9% DESTINY-Breast04: Confirmed ORR Modi et al, 2022a; Modi et al, 2022b. Trastuzumab Deruxtecan for HER2-Low MBC Complete Response Partial Response HR+ HR– T-DXd (n=333) T-DXd (n=40) TPC (n=166) TPC (n=18) Confirmed Objective Response Rate 52.6% 50.0% 16.3% 16.7% 49.2 47.5 2.5 0.6 15.7 5.6 11.1
- 57. Determining HER2-Low Status Miglietta et al, 2021; Modi et al, 2022b; Prat et al, 2022. HER2-low status changes over time Which timepoint and what type of biopsy should be used to define a tumor as HER2-low? DESTINY-Breast04 required “adequate archived or recent tumor-biopsy specimens” Excluded: fine-needle aspirates, other cytologic specimens, decalcified bone metastases In DESTINY-Breast04, T-DXd had consistent efficacy regardless of tumor sample characteristics Biopsy Considerations DESTINY-Breast04: Median PFS by Tumor Sample Characteristics Practical Definition of HER2-Low A HER2-nonamplified tumor showing HER2-low expression on any prior specimen in course of disease Hazard Ratio (T-DXd vs TPC) Subgroup T-DXd TPC Hazard Ratio (95% CI) 0.47 (0.32-0.70) 0.50 (0.38-0.66) 0.46 (0.35-0.59) 0.57 (0.33-1.0) 0.48 (0.37-0.61) 0.57 (0.30-1.1) 0.78 (0.24-2.54) 0.44 (0.28-0.70) 0.49 (0.37-0.66) 0.54 (0.20-1.4) 4.2 5.4 5.3 3.0 5.3 4.8 6.8 4.3 5.1 2.8 9.6 10.9 10.9 7.5 10.3 9.7 7.0 11.4 9.8 6.6 Tumor Location Primary (n=196) Metastases (n=359) Specimen Type Biopsy (n=448) Excision/resection (n=108) Archival tissue (n=482) Newly obtained tissue (n=75) Specimen Collection Date 2013 and earlier (n=29) 2014-2018 (n=175) 2019 or later (n=310) Missing (n=43) mPFS, Mo 3 2 1 0
- 58. Decreasing ORR by degree of HER2 expression IHC 3+ IHC 1+ or 2+ IHC 0 DAISY Trial: Benefit Even in HER2 0 Diéras et al, 2022. Phase 2 Study T-DXd for Advanced Breast Cancer Total Cohort 1 (HER2-overexpressing) Cohort 2 (HER2–low expressing Cohort 3 (HER2-nondetected) Best overall response confirmed, n/N [95% CI] 86 / 177 (48.6%) [41.0-56.2] 48 / 68 (70.6%) [58.3-81.0] 27 / 72 (37.5%) [26.4-49.7] 11 /37 (29.7%) [15.9-47.0] Median DOR, months [95% CI] 8.5 [6.5-9.8] 9.7 [6.8-13] 7.6 [4.2-9.2] 6.8 [2.8-not reached] Median PFS, months [95% CI] 7.0 [6.0-8.7] 11.1 [8.5-14.4] 6.7 [4.4-8.3] 4.2 [2.0-5.7]
- 59. How do you choose between sacituzumab govitecan or T-DXd?
- 60. Both SG and T-DXd (HR– Patients) Can Improve PFS Bardia et al, 2021; Modi et al, 2022a; Hurvitz et al, 2022; Modi et al, 2022b. SG (n=235) TPC (n=233) Median PFS, months (95% CI) 5.6 (4.3−6.3) 1.7 (1.5-2.5) HR (95% CI), P value 0.41 (0.32−0.52),P<0.0001 T-DXd mPFS:8.5 mo 5.6 mo 月 TPC mPFS:2.9个 T-DXd (n=40): TPC (n=18): HR: 0.46 95% CI, 0.24-0.89 In the main study population of ASCENT and HER2–low expression mTNBC of DB-04, both SG and T-DXd can significantly improve PFS compared with TPC, but only a small part of mTNBC population in DB-04 is used for exploratory analysis of survival end points. Therefore, it is used to generate hypotheses, and the results need to be interpreted carefully DESTINY-Breast04: PFS (HR– Patients) ASCENT: PFS (Primary Study Population) Primary end point Exploratory end point HR almost consistent in ASCENT and DB-04, even lower in ASCENT
- 61. SG (n=235) TPC (n=233) Median OS, months (95% CI) 12.1 (10.7–14.0) 6.7 (5.8-7.7) HR (95% CI), P value 0.48 (0.38–0.59), P<0.0001 OS(%) SG TPC Censored T-DXd mOS: 18.2 mo 月 9.9 mo TPC mOS:8.3 mo HR:0.48 95% CI: 0.24-0.95 In the main study population of ASCENT and HER2–low expression mTNBC of DB-04, both SG and T-DXd can significantly improve OS compared with TPC, but only a small part of mTNBC population in DB-04 is used for exploratory analysis of survival end points. Therefore, it is used to generate hypotheses, and the results need to be interpreted carefully DESTINY-Breast04: OS (HR– Patients) ASCENT: OS (Primary Study Population) Both SG and T-DXd (HR– Patients) Can Improve OS Bardia et al, 2021; Modi et al, 2022a; Hurvitz et al, 2022; Modi et al, 2022b. HR in ASCENT and DB-04 is almost consistent
- 62. SG (n=235) TPC (n=233) Treatment-emergent adverse event a Any grade e % Grade 3, % Grade 4, % Any grade, % Grade 3, % Grade 4, % Hematologic Neutropeniab 63 34 17 43 20 13 Anemia 35 8 0 24 5 0 WBC count decreased 13 7 1 10 4 1 Febrile neutropenia 6 5 1 2 2 <1 Gastrointestinal Diarrhea 59 11 0 12 <1 0 Nausea 57 2 <1 26 <1 0 Vomiting 29 1 <1 10 <1 0 Other Fatigue 45 3 0 30 5 0 Alopecia 46 0 0 16 0 0 ASCENT DESTINY-Breast04 • The most common grade 3-4 TEAEsa in the SG arm were neutropenia and diarrhea, which were manageable and did not interrupt treatment due to treatment- related neutropenia and diarrhea. Neutropeniaa was the most common serious TEAEs reported with T-DXd in DB-04 • Alopecia occurred in 46% of SG-treated patients and 38% of T-DXd-treated patients reported alopecia in DB-04 ASCENT vs DESTINY-Breast04 aTreatment-emergent adverse event is defined as an adverse event with the start date on or after the date of the first dose of study treatment and up to 30 days after the date of the last dose of the study treatment. bNeutropenia is combined “neutropenia” and “neutrophil count decreased.” Bardia et al, 2022; Rugo, Tolaney, et al, 2021; Modi et al, 2022a. Treatment-Emergent Adverse Events (TEAEs)
- 63. DESTINY-Breast04: Trastuzumab Deruxtecan aThe median time to ILD/pneumonia onset for T-DXd patients was 129.0 days (range, 26-710). bA total of 17 patients (4.6%) in the T-DXd group reported. Left ventricular dysfunction; 1 patient initially presented with decreased ejection fraction and subsequently developed heart failure. cBoth heart failure patients recovered. dProvided information refers to full DESTINY-Breast04 study population. ILD = interstitial lung disease. Modi et al, 2022a. Adverse Events of Special Interest Adjudicated as Drug-Related ILD/Pneumonitisa N (%) Grade 1 Grade 2 Grade 3 Grade 4 Grade 5 Any Grade T-DXd (n=371) 13 (3.5%) 24 (6.5%) 5 (1.3%) 0 3 (0.8%) 45 (12.1%) TPC (n=172) 1 (0.6%) 0 0 0 0 1 (0.6%) Left Ventricular Dysfunctionb N (%) Grade 1 Grade 2 Grade 3 Grade 4 Grade 5 Any Grade Ejection Fraction Decreased T-DXd (n=371) 1 (0.3%) 14 (3.8%) 1 (0.3%) 0 0 16 (4.3%) TPC (n=172) 0 0 0 0 0 0 Cardiac Failurec T-DXd (n=371) 0 1 (0.3%) 1 (0.3%) 0 0 2 (0.5%) TPC (n=172) 0 0 0 0 0 0 8% of patients in the T-DXd arm had grade 2 or 3 ILD There were 3 T-DXd–related deaths due to ILD in DB-04
- 64. TROPiCS-02: Efficacy by HER2 IHC Status aHER2-low defined as IHC1+ or IHC2+ and ISH–/unavailable. Rugo HS, Bardia A et al, 2022; Marmé et al, 2022. Sacituzumab Govitecan in Metastatic Breast Cancer ITT SG (n=272) TPC Median PFS, mo (95% CI) 5.5 (4.2–7.0) 4.0 (3.1–4.4) HR (95% CI) 0.66 (0.53–0.83), P=0.0003 SG (n=149) TPC (n=134) Median PFS, mo 6.4 4.2 HR (95% CI) 0.58 (0.42–0.79), P<0.001 SG (n=101) TPC (n=116) Median PFS, mo 5.0 3.4 HR (95% CI) 0.72 (0.51–1.00), P=0.05 PFS Probability (%) 0 0 2 4 6 8 10 12 Time (months) 14 16 18 20 22 101 116 53 39 20 14 7 3 1 1 1 1 0 TPC No. of patients at risk SG 64 50 27 20 9 4 3 2 1 1 0 10 20 30 40 50 60 70 80 90 100 SG TPC Censored PFS Probability (%) 0 0 2 4 6 8 10 12 Time (months) 14 16 18 20 22 149 134 65 43 16 8 4 1 0 0 0 0 0 TPC No. of patients at risk SG 99 77 50 38 22 16 8 7 5 5 2 10 20 30 40 50 60 70 80 90 100 SG TPC Censored 0 0 3 6 9 12 Time (months) 15 18 21 24 272 148 82 44 22 12 6 3 0 271 105 41 17 4 1 1 0 TPC No. of patients at risk SG 10 20 30 40 50 60 70 80 90 100 PFS Probability (%) SG TPC Censored HER2 IHC0 HER2-Lowa Within the HER2-low population, median PFS with SG vs TPC for the IHC1+ and IHC2+ subgroups was 7.0 vs 4.3 (HR, 0.57) and 5.6 vs 4.0 (HR, 0.58) months, respectively Median PFS in a sensitivity analysis of the HER2-low subgroup did not show any differences compared with the ITT population SG Improved PFS vs TPC in HER2 IHC0 and HER2-Low Groups, Consistent With Outcomes in the ITT Population
- 65. ASCENT vs DESTINY-Breast04: Quality of Life HRQOL = health-related quality of life. aAssessed in patients who received ≥1 dose of study drug. For global health status and functional scales, a higher score indicates better quality of life. For symptom scales, a lower score indicates better quality of life. *P<0.05. **P<0.01. Loibl et al, 2021; Ueno et al, 2022. Primary Health-Related of Life Domains EORTC C30a Change from Baseline, (95% CI) SG (n=235) TPC (n=233) Difference Minimum Difference Global Health Status/Quality Life 0.66 (-2.21, 3.53) -3.42 (-6.77, -0.08) 4.08 (0.82, 7.35)* -4 Physical Functioning 1.31 (-1.38, 3.99) -4.39 (-7.52, -1.26) 5.69 (2.63, 8.76)** -5 Role Functioning -2.24 (-6.13, 1.65) -7.83 (-12.41, -3.25) 5.59 (1.13, 10.05)* -6 Fatigue 1.97 (-1.20, 5.13) 7. 13 (3.40, 10.87) -5.17 (-8.81, -1.52)* +5 Pain -8.93 (-12.57, -5.30) -1.89 (-6.18, 2.40) -7.04 (-11.24, -2.85)** +6 • In ASCENT, SG demonstrated statistically significant and/or clinically meaningful improvements relative to baseline in all main HRQOL domains over TPC arm • In DB-04, T-DXd showed no significant differences vs the TPC arm in global health status/QOL or fatigue Fatigue Global Health Status/QOL DESTINY-Breast04 Quality of Life ASCENT Quality of Life
- 66. • SG has demonstrated efficacy in the ITT population of patients with mTNBC in a dedicated phase 3 study regardless of HER2 status • T-DXd has shown preliminary efficacy data in a small subset of patients with mTNBC in an exploratory analysis of 58 patients • Due to differences in patient populations, direct comparisons between any of the study end points cannot be made ASCENT DESTINY-Breast04 Population size Patients with mTNBC: N=529 Of patients with centrally assessed HER2 status: HER2-IHC 0 = 70% (293/416), 149 treated with SG HER2-low = 30% (123/416), 63 treated with SG Patients with mTNBC (n=58; 40 treated with T-DXd); subset of study population of patients with HER2-low disease (N=557) Statistical considerations Efficacy in patients with mTNBC is the primary end point of the study Efficacy in patients with mTNBC is an exploratory end point Efficacy Statistically significant and clinically meaningful improvements in PFS, OS, and ORR with SG versus TPC regardless of HER2– subtype Numerical improvements in PFS, OS, and ORR with T-DXd versus TPC Implications for mTNBC SG has demonstrated efficacy in all mTNBC patients including those with HER2-low and those with HER2- IHC 0 disease T-DXd has demonstrated efficacy only in patients with HER2-low ASCENT vs DESTINY-Breast04 mTNBC Subset Bardia et al, 2021; Modi et al, 2022b; Hurvitz et al, 2022; Modi et al, 2022a. Efficacy Overview
- 67. Which ongoing investigations with immunotherapies or targeted therapies do you feel have the greatest potential to impact future practice in TNBC?
- 68. SG’s DLT is neutropenia, while DS-1062’s DLTs are maculopapular rash and stomatitis/mucosal inflammation DS-1062 has a substantially longer half-life than SG (≈5 days vs 11-14 hours), enabling a more optimal dosing regimen DS-1062 has a drug-to-antibody ratio of 4 for optimized therapeutic index Circulating free payload is negligible due to high stability of the linker, thereby limiting systemic exposure or nontargeted delivery of the payload High-potency membrane-permeable payload (DXd) that requires Trop2- mediated internalization for release Datopotamab Deruxtecan (Dato-DXd) DLT = dose-limiting toxicity. Nakada et al, 2019; Okajima et al, 2021; Ocean et al, 2017; Sands et al, 2018; Spira et al, 2021; Lisberg et al, 2020; Heist et al, 2019. Trop2 ADC in Development
- 69. TROPION-PanTumor01: Study Design RECIST = response valuation criteria in solid tumors; NSCLC = non–small cell lung cancer; SCLC = small cell lung cancer; CRPC = castration-resistant prostate cancer. Bardia et al, 2023. Dato-DXd in Advanced TNBC Key Eligibility Criteria • Advanced/unresectable or metastatic HR– /HER2– (IHC 0/1+ or IHC2+/ISH–) breast cancer • Relapsed or progressed after local standard treatments • Unselected for Trop-2 expression • Age ≥18 years (US) or ≥20 years (Japan) • ECOG PS 0-1 • Measurable disease per RECIST v1.1 • Stable, treated brain metastases allowed NSCLC (0.27 to 10 mg/kg IV Q3W) TNBC 8 mg/kg IV Q3W (n=2) 6 mg/kg IV Q3W (n=42) HR+/HER2– breast cancer 6 mg/kg IV Q3W (n=41) Other tumor types (SCLC, bladder, gastric, esophageal, CRPC, pancreas) Primary end points • Safety • Tolerability Secondary end points • Efficacy • Pharmacokinetics • Antidrug antibodies
- 70. TROPION-PanTumor01: Efficacy ORR by BICR All patients: 32% Topo I inhibitor–naive patients: 44% mDOR 16.8 months in both groups mPFS All patients: 4.4 months Topo I inhibitor–naive patients: 7.3 months mOS All patients: 13.5 months Topo I inhibitor–naive patients: 14.3 months AEs: most common TEAEs: stomatitis (73%), nausea (66%), vomiting (39%) Dato-DXd in Advanced TNBC Antitumor Tumor Responses by BICR Bardia et al, 2023.
- 71. TROPION-Breast 02: Study Design ICC = investigator’s choice chemotherapy; Q4W = every 4 weeks; DFI = disease-free interval. Dent et al, 2022. Dato-DXd vs Chemo in 1L mTNBC Not Candidate for Anti–PD-(L)1 Therapy TROPION-Breast02 is a phase 3, open-label, randomized study of 1L dato-DXd vs chemotherapy in patients with locally recurrent inoperable or metastatic TNBC who are not candidates for anti-PD-(L)1 therapy N=600 R 1:1 Primary end points • PFS by BICR per RECIST v1.1 • OS Secondary end points • ORR and DOR by BICR per RECIST v.1.1 • PFS by investigator assessment per RECIST v1.1 • PFS2 Stratification factors • Geographic location • DFI history • PD-L1 status Key Eligibility Criteria • Adults with histologically or cytologically documented locally recurrent inoperable or metastatic TNBC • No prior chemotherapy or targeted systemic therapy for locally recurrent inoperable or metastatic breast cancer • ≥1 measurable lesion (≥10 mm) per RECIST v1.1 that has not been previously irradiated • ECOG PS 0-1 • A recent (<3 months prior to screening) formalin-fixed, paraffin- embedded metastatic (excluding bone) or locally recurrent inoperable tumor sample • Not a candidate for PD-(L)1 inhibitor therapy, defined as: Patients whose tumors are PD-L1– Patients whose tumors are PD-L1+, but have o Relapsed after prior PD-(L)1 inhibitor therapy for early- stage breast cancer o Comorbidities precluding PD-(L)1 inhibitor therapy o No regulatory access to PD-(L)1 inhibitor therapy • Eligible for 1 of the listed ICCs (ie, paclitaxel, nab-paclitaxel, capecitabine, carboplatin, or eribulin mesylate) ICC Q3W or Q4W as per protocol directions (paclitaxel, nab-paclitaxel, capecitabine, eribulin mesylate, or carboplatin Dato-DXd 6 mg/kg IV Day 1 Q3W
- 72. Patritumab Deruxtecan GI = gastrointestinal. Li et al, 2017; Ocana et al, 2013; Krop et al, 2022; Corti et al, 2021. HER3 is expressed in 30.3%-75.1% of breast cancers; overexpression is associated with poor prognosis Patritumab deruxtecan: novel ADC targeting HER3 with topoisomerase I inhibitor payload capable of bystander antitumor effects Phase 1/2 trial of patritumab deruxtecan at 1.6-8.0 mg/kg (dose escalation/finding) or 4.8-6.4 mg/kg IV Q3W (dose expansion), with median follow-up of 31.9 months (range: 15-56 months) Phase 1/2 Trial in HER3-Expressing MBC Patritumab deruxtecan is active regardless of HER3 expression 6.6% had treatment-related ILD, including 1 grade 5 ILD (0.5%) Most common TEAEs were GI and hematologic toxicities Nausea: 68.8%-80.6% Platelet count decrease: 60.4%-71.4%; neutrophil count decrease: 62.5%-66.3% Parameter HR+/ HER2– (n=113) TNBC (n=53) HER2-+ (n=14) HER3 status High and low High High Confirmed ORR, % 30.1 22.6 42.9 Median DOR, months 7.2 5.9 8.3 Median OS, mo 14.6 14.6 19.5 Median PFS, months 7.4 5.5 11.0
- 73. Phase 3 Trial Treatment Arm(s) Population Primary Completion 1L ASCENT-03 (NCT05382299) Sacituzumab govitecan vs TPC Metastatic TNBC (N=540) May 2027 ASCENT-04 (NCT05382286) Sacituzumab govitecan + pembrolizumab vs TPC + pembrolizumab Inoperable/metastatic TNBC (N=440) February 2027 DESTINY-Breast09 (NCT04784715) T-DXd ± pertuzumab vs taxane/trastuzumab/pertuzumab HER2-positive MBC (N=1,134) March 28, 2025 TROPION-Breast02 (NCT05374512) Dato-DXd vs TPC Inoperable/metastatic TNBC ineligible for ineligible for PD-1/PD-L1 therapy (N=600) December 3, 2025 Select Ongoing Phase 3 Trials of ADCs in TNBC Clinicaltrials.gov, 2023h; Clinicaltrials.gov, 2023g; Clinicaltrials.gov, 2023i; Clinicaltrials.gov, 2023a.
- 74. SG Dato-DXd ADC2 T-DXd T-DXd Dato-DXd ADC1 T-DXd ADC Y ADC X Critical Question: How Will ADCs Work in Sequence?
- 75. Performance of Serial ADCs Abelman et al, 2023. Subgroup Analysis of Patients Receiving T-DXd, SG Only ADC1 ADC2
- 76. Key Eligibility Criteria • Confirmed unresectable locally locally advanced or metastatic metastatic disease • History of HER2-low breast cancer (any prior primary or or metastatic tumor) defined defined as IHC 1+ or 2+/ISH– 2+/ISH–non-amplified • Most recent pathology: HER2 HER2 IHC 0 or HER2-low • Measurable disease • No prior Topo-I inhibitor–- based therapy TRADE-DXd CBR = clinical benefit rate; TTOR = time to overall response. Patients who received T-DXd/dato-DXd as ADC off-study were allowed to enroll on ADC1 cohorts. TReatment of ADC-Refractory Breast CancEr with Dato-DXd or T-DXd ADC1 ADC2 Primary end point • ORR Secondary end points • PFS • OS • CBR • TTOR • DOR Baseline pre-ADC1 biopsy Post-C2 on-ADC1 biopsy Baseline pre-ADC2 biopsy Optional post-ADC2 biopsy Crossover to ADC2 at progression Crossover to ADC1 at progression R 1:1 T-DXd 0-1 prior lines HR+ (Arm A) HR– (Arm B) Dato-DXd 0-1 prior lines HR+ (Arm C) HR– (Arm D) Dato-DXd 1-2 prior lines HR+ (Arm E) HR– (Arm F) T-DXd 1-2 prior lines HR+ (Arm G) HR– (Arm H) Treat until disease progression or unacceptable toxicity = Tumor assessments + blood collection Q9W
- 77. BRCAm = BRCA-mutant; dMMR = deficient mismatch repair. NCCN, 2023. 1L 2L 3L PD-L1+: Chemo + pembrolizumab PD-L1–: Taxane or platinum Sacituzumab govitecan High TMB, MSI-H/dMMR: Pembrolizumab HER2-low: T-DXd BRCAm: Olaparib or talazoparib Eribulin, capecitabine, gemcitabine, navelbine Potential Future Strategies Dato-DXd HER3+ : Patritumab deruxtecan Sacituzumab govitecan Where ADCs Fit Into Treatment of Metastatic TNBC
- 78. Other Strategies in TNBC PI3Ki = phosphoinositide 3-kinase inhibitor. Clinicaltrials.gov, 2023c; Clinicaltrials.gov, 2023b; Clinicaltrials.gov, 2023d; Clinicaltrials.gov, 2023e; Clinicaltrials.gov, 2023f; Clinicaltrials.gov, 2023j; Doi et al, 2022; Hamilton et al, 2023; Meric-Bernstam et al, 2022; Meisel et al, 2022; Ono et al, 2022. Targeted strategies Akt inhibition: awaiting data from CAPItello-290 Mutant-selective PI3Ki: Loxo (LOXO-783), Relay (RLY-2608), Scorpion (STX-478), and others Other immunotherapy strategies AdvanTIG-211 (ociperlimab/tislelizumab), PRESERVE-2 (trilaciclib) Novel ADCs Novel targets: B7-H3 (DS-7300), B7H4 (XMT 1660, AZD8205), LIV1 (ladiratuzumab vedotin), Nectin-4 (enfortumab vedotin)
- 80. T-DXd and Sacituzumab Govitecan in Breast Cancer CINV = chemotherapy-induced nausea and vomiting; LVEF = left ventricular ejection fraction; DDIs = drug-drug interactions; UGT1A1 = uridine-diphosphate glucuronosyltransferase 1A1. Enhertu® prescribing information, 2022; Rugo, Bianchini, et al, 2022; Trodelvy® prescribing information, 2023. Administration Considerations Consideration T-DXd Sacituzumab Govitecan Premedication CINV: 3-drug combination regimen (dexamethasone + 5-HT3 receptor antagonist + NK1 receptor antagonist) Infusion reactions: premedicate with antipyretics, H1 and H2 blockers; consider corticosteroids for those those with prior infusion reactions CINV: 2- to 3-drug combination regimen (eg, dexamethasone + either 5-HT3 or NK1 receptor antagonist) Some institutions may use only ondansetron Starting dosage 5.4 mg/kg IV Q3W until progressive disease/unacceptable toxicity 10 mg/kg IV QW on Days 1 and 8 of 21-day cycles until progressive disease/unacceptable toxicity Dose reductions First: 4.4 mg/kg Second: 3.2 mg/kg Third: discontinue First: 25% dose reduction Second: 50% dose reduction Third: discontinue Key toxicities managed dose modifications ILD/pneumonitis, nausea, neutropenia, neutropenia, thrombocytopenia, LVEF Neutropenia, nausea, vomiting, diarrhea, any other high-grade/persistent AEs DDIs Very limited/not clinically meaningful Avoid coadministering UGT1A1 inhibitors or inducers
- 81. T-DXd: Safety Profile aEjection fraction decrease and cardiac failure data from first interim analysis; drug-related ILD/pneumonitis from second interim analysis. ABC = advanced breast cancer. Modi et al, 2022a; Modi et al, 2022b; Hurvitz et al, 2023; Cortés et al, 2022. DESTINY-Breast04: Drug-Related TEAEs in ≥20% of Patients With HER2-Low ABC Fatigue Neutropenia Anemia Thrombocytopenia Transaminases increased Leukopenia Patients (%) Any Grade Grade ≥3 T-DXd Chemo AE of Special Interest, % DESTINY-Breast04: Low ABC DESTINY-Breast03: HER2-Positive MBCa T-DXd (n=371) TPC (n=172) T-DXd (n=257) T-DM1 (n=261) Drug-related ILD/pneumonitis Grade 1 Grade 2 Grade 3 12.1% 3.5% 6.5% 1.3% 0.6% 0.6% 0% 0% 15% 4% 10% <1% 3% 2% 1% <1% Ejection fraction decreased Grade 1 Grade 2 Grade 3 4.3% 0.3% 3.8% 0.3% 0% 0% 0% 0% 2.3% 0% 2.3% 0% 0.4% 0% 0.4% 0% Cardiac failure Grade 1 Grade 2 Grade 3 0.5% 0% 0.3% 0.3% 0% 0% 0% 0% 0% 0% 0% 0% 0% 0% 0% 0% Nausea Alopecia Vomiting Decreased appetite Diarrhea Constipation 80 60 40 20 0 20 40 60 73 5 24 0 48 8 42 5 33 14 51 41 38 0 33 0 34 1 10 0 33 8 23 5 29 2 16 1 24 5 9 1 24 3 23 8 23 6 31 19 22 1 18 2 21 0 0 13 Safety profile of T-DXd was consistent across trials and disease settings n=3 grade 5 drug-related ILD/pneumonitis cases with T- DXd occurred in DESTINY-Breast04 All other AEs of special interest noted above were grade ≤3 in both trials
- 82. Stankowicz et al, 2021; Rugo, Bianchini et al, 2022. Premedicate with 3-drug regimen for CINV (eg, dexamethasone + 5-HT3 receptor antagonist + NK1 receptor antagonist) Onset may be delayed: provide patient with take-home antiemetics (eg, dexamethasone, ondansetron) Manage with antiemetics, dose reductions; withhold if high-grade until resolved to grade ≤1 Managing Clinically Significant Nausea and Vomiting With T-DXd
- 83. Managing ILD/Pneumonitis With T-DXd CT = computed tomography; ID = infectious disease; CBC = complete blood count; BAL = bronchoalveolar lavage; PFT = pulmonary function test; PK = pharmacokinetic; PCP = pneumocystis jirovecii pneumonia. Swain et al, 2022; Enhertu® prescribing information, 2022. Monitor Urge patients to immediately report cough, dyspnea, fever, and/or new or worsening respiratory symptoms Monitor for signs/ symptoms of ILD Promptly investigate evidence of ILD Evaluate patients with suspected ILD by radiographic imaging and assess as follows Consider earlier scans to assess response and monitor for ILD For grade 1 (asymptomatic): Hold until resolved to grade 0 For grades 2-4 (symptomatic): Permanently discontinue Dose Interruptions Recommended starting dose First dose reduction Second dose reduction Do not reescalate T-DXd dose after dose reduction is made 5.4 mg/kg 4.4 mg/kg 3.2 mg/kg Further dose reduction needed Permanently discontinue Confirm Assessments should include: High-resolution CT Pulmonologist consult; if indicated, ID consult Blood culture and CBC; other blood tests as needed Consider bronchoscopy and BAL if indicated/feasible PFTs and pulse oximetry Arterial blood gases, if indicated As soon as ILD suspected, collect 1 blood sample for PK assessment, if feasible Rule out other causes of ILD (eg, progression, PCP infection, other drugs, radiotherapy) All ILD events should be followed until resolution and after drug discontinuation Corticosteroid Treatment For grade 1 (asymptomatic): Consider corticosteroid treatment (≥0.5 mg/kg prednisolone) For grade ≥2 (symptomatic): Promptly initiate systemic corticosteroid treatment (≥1 mg/kg prednisolone or equivalent) for ≥14 days followed by taper for ≥4 weeks Resume Therapy (Grade 1 Only) If resolved in ≤28 days from onset: Maintain dose If resolved >28 days from onset: Reduce dose 1 level
- 84. Sacituzumab Govitecan: Safety Profile Rugo, Bardia, et al, 2022; Bardia et al, 2021. Safety profile consistent in HR+/HER2– MBC (TROPiCS-02) and mTNBC (ASCENT) No treatment-related cardiac failure or LVEF observed Alopecia often observed at higher rates in real-world practice Counsel patients on hair loss Offer wig prescription TRAEs, n (%) SG (n=268) TPC (n=249) All Grade Grade ≥3 All Grade Grade ≥3 Hematologic Neutropenia 188 (70%) 136 (51%) 134 (54%) 94 (38%) Anemia 91 (34%) 17 (6%) 62 (25%) 8 (3%) Leukopenia 37 (14%) 23 (9%) 23 (9%) 13 (5%) Lymphopenia 31 (12%) 10 (4%) 25 (10%) 8 (3%) Febrile neutropenia 14 (5%) 14 (5%) 11 (4%) 11 (4%) Gastrointestinal Diarrhea 152 (57%) 25 (9%) 41 (16%) 3 (1%) Nausea 148 (55%) 3 (1%) 77 (31%) 7 (3%) Vomiting 50 (19%) 1 (<1%) 30 (12%) 4 (2%) Constipation 49 (18%) 0 36 (14%) 0 Abdominal pain 34 (13%) 2 (1%) 17 (7%) 0 Other Alopecia 123 (46%) 0 41 (16%) 0 Fatigue 100 (37%) 15 (6%) 73 (29%) 6 (2%) Asthenia 53 (20%) 5 (2%) 37 (15%) 2 (1%) Decreased appetite 41 (15%) 1 (<1%) 34 (14%) 1 (<1%) Neuropathy 23 (9%) 3 (1%) 38 (15%) 6 (2%) TROPiCS-02: Key TRAEs With SG vs TPC in HR+/HER– MBC
- 85. Managing Neutropenia With Approved ADCs ANC = absolute neutrophil count; G-CSF = granulocyte colony stimulating factor. Tolaney, personal communication, 2023 Rugo, Bianchini, et al, 2022; Enhertu® prescribing information, 2022; Trodelvy® prescribing information, 2023; Rugo, Tolaney, et al, 2022; Fleming et al, 2021; Spring et al, 2021. T-DXd Educate on potential for neutropenia, usually low grade Consider G-CSF prophylaxis if history of prior neutropenic complications Monitor regularly and withhold if ANC <1,000/µL or neutropenic fever Manage with G-CSF; dose reductions for grade 4 neutropenia or grade 3 febrile neutropenia Educate on potential for severe neutropenia Monitor regularly and withhold if ANC <1,500/µL on Day 1 or <1,000/µL on Day 8, or neutropenic fever Manage with G-CSF and dose reductions for grade 4 lasting ≥7 days or grade ≥3 febrile neutropenia When making dose reductions, consider patient’s bone marrow reserve, age, frailty, etc Use anti-infective treatment for febrile neutropenia Suspect UGT1A1*28 genotype if prolonged neutropenia unresponsive to treatment Sacituzumab Govitecan G-CSF for SG-Related Neutropenia—Consider Either: 1. Short-acting G-CSF on Days 2-4 and long-acting G- CSF on Day 9, or 2. Just long-acting G-CSF on Day 9
- 86. Managing Diarrhea With Sacituzumab Govitecan Fleming et al, 2021; Rugo, Tolaney et al 2022; Trodelvy® prescribing information, 2023; Spring et al, 2021. Educate patients about potential for severe diarrhea and about loperamide before first dose Prophylaxis not recommended unless prior history of diarrhea For early diarrhea of any severity, administer atropine For late diarrhea, rule out infectious etiologies and administer loperamide Manage with fluids, electrolyte substitution, dose reductions; withhold for grade ≥3 until resolution
- 88. Case Study 1: Ms. KQ 56-year-old woman presented with de novo metastatic TNBC with a left- sided breast mass, ipsilateral enlarged axillary lymph node, and liver and lung metastases Breast and ipsilateral lymph node = ER–, PR–, HER2 1+ Biopsy of the liver confirmed metastatic TNBC Her tumor was found to be PD-L1+ Germline genetic testing did not reveal a BRCA mutation She received first line paclitaxel + pembrolizumab and had a good response, but after 8 months, developed disease progression with growth of liver metastases
- 89. Case Study 1: Ms. KQ (cont.) Image courtesy of Ira Bleiweiss, MD. PD-L1+
- 90. Case Study 1: Ms. KQ (cont.) a. Olaparib b. Carboplatin c. Sacituzumab govitecan d. Trastuzumab deruxtecan e. Capecitabine What Therapy Do You Recommend?
- 91. Case Study 1: Ms. KQ (cont.) a. Olaparib b. Carboplatin c. Sacituzumab govitecan d. Trastuzumab deruxtecan e. Capecitabine What Therapy Do You Recommend?
- 92. Case Study 2: Ms. TL L = left; FNA = fine needle aspiration; ddAC-T = dose-dense doxorubicin/cyclophosphamide/paclitaxel. 36-year-old woman initially presented with 3.5-cm L breast mass with an enlarged axillary lymph node 2 years ago Breast biopsy revealed ER–, PR–, HER2 1+ invasive ductal carcinoma FNA was positive for malignant cells She received preoperative ddACT chemotherapy At surgery, she was found to have a partial CR
- 93. Case Study 2: Ms. TL Image courtesy of Ira Bleiweiss, MD. HER2 0
- 94. Case Study 2: Ms. GB Image courtesy of Ira Bleiweiss, MD. HER2 1+
- 95. Case Study 2: Ms. TL (cont.) AST = aspartate aminotransferase; ALT = alanine transaminase. Germline genetic testing was done, and she was found to have a BRCA1 mutation 2 years after surgery, she was found to have elevated transaminases (AST 75 U/L, ALT 80 U/L), and imaging revealed liver metastases Biopsy of the liver was consistent with her breast primary, ER–, PR–, HER2 1+ PD-L1 testing was done with 22C3 yielding CPS >10
- 96. Case Study 2: Ms. TL (cont.) Image courtesy of Ira Bleiweiss, MD. Primary TNBC, Extensive Necrosis
- 97. Case Study 2: Ms. TL (cont.) Image courtesy of Ira Bleiweiss, MD. PD-L1+ ?
- 98. Case Study 2: Ms. TL (cont.) Image courtesy of Ira J. Bleiweiss, MD. Liver Biopsy
- 99. Case Study 2: Ms. TL (cont.) Image courtesy of Ira J. Bleiweiss, MD. PD-L1–
- 100. Case Study 2: Ms. TL (cont.) Image courtesy of Ira Bleiweiss, MD. Original Axillary Node +
- 101. Case Study 2: Ms. TL (cont.) Image courtesy of Ira Bleiweiss, MD. PD-L1+
- 102. Case Study 2: Ms. TL (cont.) a. Olaparib b. Carboplatin c. Sacituzumab govitecan d. Trastuzumab deruxtecan e. Paclitaxel f. Carboplatin/gemcitabine/pembrolizumab What Therapy Do You Recommend?
- 103. Case Study 2: Ms. TL (cont.) a. Olaparib b. Carboplatin c. Sacituzumab govitecan d. Trastuzumab deruxtecan e. Paclitaxel f. Carboplatin/gemcitabine/pembrolizumab What Therapy Do You Recommend?
- 104. Case Study 2: Ms. TL (cont.) She starts on carbo/gem/pembro and has a nice response for 12 months, but then has disease progression in her liver What do you now recommend? a. T-DXd b. Sacituzumab govitecan c. Paclitaxel d. Paclitaxel + pembrolizumab e. Olaparib
- 105. Case Study 2: Ms. TL (cont.) What do you now recommend? a. T-DXd b. Sacituzumab govitecan c. Paclitaxel d. Paclitaxel + pembrolizumab e. Olaparib
- 106. Key Takeaways Triple-negative breast cancers are generally poorly differentiated duct carcinomas Rare variants of triple-negative invasive breast carcinomas exist, many of which have a good prognosis A pathology report detailing a well differentiated breast carcinoma which is triple-negative should raise a red flag as it likely incorrect and deserves investigation
- 107. Key Takeaways (cont.) Key biomarker information is needed to determine therapy recommendations in TNBC: PDL1, HER2-low, BRCAm, PALB2m, TMB, NTRK, MSI First-line therapy with chemo + pembro is standard for PDL1+mTNBC Will need to understand how to approach patients who recur after adjuvant pembro ADC + immunotherapy may become a new first-line standard ADCs currently are the second-line standard For HER2-low patients, slight preference for sacituzumab govitecan over TDXd given robust phase 3 data Sequencing ADCs is currently reasonable, but more data is needed
- 108. Questions for the Faculty? Download the Triple-Negative Breast Cancer Essentials Pocket Guide App! After scanning the QR code, follow these steps to add to your home screen: FOR IPHONE: Click the Share arrow on your screen Scroll to the bottom & click ‘Add to Home Screen’ FOR ANDROID: Click the 3 dots on your screen Click ‘Install App’ This TNBC app includes: Guideline summaries on evidence-based management of TNBC Treatment and supportive care information Answers to FAQs Further Q&As with the expert faculty
- 109. References Abelman RO, Hartley-Blossom Z, Fell GG, et al (2023). Sequential use of antibody-drug conjugate after antibody-drug conjugate for patients with metastatic breast cancer: ADC after ADC (A3) study. J Clin Oncol, 41(suppl_16):1022. DOI:10.1200/JCO.2023.41.16_suppl.1022 Allison KH, Hammond MEH, Dowsett M, et al (2020). Estrogen and progesterone receptor testing in breast cancer: ASCO/CAP guideline update. J Clin Oncol, 38(12):1346-1366. DOI:10.1200/JCO.19.02309 Ambrogi F, Fornili M, Boracchi P, et al (2014). Trop-2 is a determinant of breast cancer survival. PLoS One, 9(5):e96993. DOI:10.1371/journal.pone.0096993 American Cancer Society (2023). Triple-negative breast cancer. Available at: https://www.cancer.org/cancer/breast-cancer/understanding-a-breast-cancer-diagnosis/types-of-breast- cancer/triple-negative.html Amin MB, Edge S, Green F, et al (2017). AJCC Cancer Staging Manual. 8th ed. New York, NY: Springer. Bardia A, Hurvitz SA, Tolaney SM, et al (2021). Sacituzumab govitecan in metastatic triple-negative breast cancer. N Engl J Med, 384(16):1529-1541. DOI:10.1056/NEJMoa2028485 Bardia A, Krop I, Meric-Bernstam F, et al (2023). Datopotamab deruxtecan (Dato-DXd) in advanced triple-negative breast cancer (TNBC): updated results from the phase 1 TROPION- PanTumor01 study. Cancer Res, 83(suppl_5). Abstract P6-10-03. DOI:10.1158/1538-7445.SABCS22-P6-10-03 Bardia A, Tolaney SM, Loirat D, et al (2020). LBA17 ASCENT: a randomized phase III study of sacituzumab govitecan (SG) vs treatment of physician’s choice (TPC) in patients (pts) with previously treated metastatic triple-negative breast cancer (mTNBC). Annals Oncol ESMO, 31(suppl_4); 1149-1150. DOI:10.1016/j.annonc.2020.08.2245 Bardia A, Tolaney SM, Loirat D, et al (2022). Sacituzumab govitecan (SG) versus treatment of physician’s choice (TPC) in patients (pts) with previously treated, metastatic triple-negative breast cancer (mTNBC) [oral presention]: final results from the phase 3 ASCENT study. J Clin Oncol, 40(suppl_16); 1071-1071. DOI:10.1200/JCO.2022.40.16_suppl.1071 Bauer KR, Brown M, Cress RD, et al (2007). Descriptive analysis of estrogen receptor (ER)-negative, progesterone receptor (PR)-negative, and HER2-netative invasive breast cancer, the so- called triple-negative phenotype: a population-based study from the California cancer registry. Cancer, 109(9):1721-1728. DOI:10.1002/cncr.22618 Carey LA, Loirat D, Punie K, et al (2022). Sacituzumab govitecan as second-line treatment for metastatic triple-negative breast cancer-phase 3 ASCENT study subanalysis. NPJ Breast Cancer, 8(1):72. DOI:10.1038/s41523-022-00439-5 Cardillo TM, Govindan SV, Sharkey RM, et al (2015). Sacituzumab govitecan (IMMU-132), an anti-Trop-2/SN-38 antibody-drug conjugate: characterization and efficacy in pancreatic, gastric, and other cancers. Bioconjug Chem, 26(5):919-31. DOI:10.1021/acs.bioconjchem.5b00223
- 110. References (cont.) Clinicaltrials.gov (2022). Trial of sacituzumab govitecan in participants with refractory/relapsed metastatic triple-negative breast cancer (TNBC) (ASCENT). NLM identifier: NCT02574455. Clinicaltrials.gov (2023a). A study of dato-DXd versus investigator’s choice chemotherapy in patients with locally recurrent inoperable or metastatic triple-negative breast cancer, who are not candidates for PD-1/PD-L1 inhibitor therapy (TROPION-Breast02). NLM identifier: NCT05374512. Clinicaltrials.gov (2023b). A study of LOXO-783 in patients with breast cancer/other solid tumors (PIKASSO-01). NLM identifier: NCT5307705. Clinicaltrials.gov (2023c). Capivasertib+paclitaxel as first line treatment for patients with locally advanced or metastatic TNBC (CAPItello-290). NLM identifier: NCT03997123. Clinicaltrials.gov (2023d). First-in-human study of mutant-selective PI3K⍺ inhibitor, RLY-2608, as a single agent in advanced solid tumor patients and in combination with fulvestrant in patients with advanced breast cancer. NLM identifier: NCT05216432. Clinicaltrials.gov (2023e). First-in-human study of STX-478 as monotherapy and in combination with other antineoplastic agents in participants with advanced solid tumor. NLM identifier: NCT05768139. Clinicaltrials.gov (2023f). Phase II study evaluating the efficacy and safety of ociperlimab in combination with tislelizumab and chemotherapy as first-line treatment for participants with advanced triple negative breast cancer (AdvanTIG-211). NLM identifier: NCT05809895. Clinicaltrials.gov (2023g). Study of sacituzumab govitecan-hziy and pembrolizumab versus treatment of physician’s choice and pembrolizumab in patients with previously untreated, locally advanced inoperable or metastatic triple-negative breast cancer (ASCENT-04). NLM identifier: NCT05382286. Clinicaltrials.gov (2023h). Study of sacituzumab govitecan-hziy versus treatment of physician’s choice in patients with previously untreated metastatic triple-negative breast cancer (ASCENT- 03). NLM identifier: NCT05382299. Clinicaltrials.gov (2023i). Trastuzumab deruxtecan (T-DXd) with or without pertuzumab versus taxane, trastuzumab and pertuzumab in HER2-positive metastatic breast cancer (DESTINY- Breast09). NLM identifier: NCT04784715. Clinicaltrials.gov (2023j). Trilaciclib, a CDK 4/6 inhibitor, in patients receiving gemcitabine and carboplatin for metastatic triple-negative breast cancer (TNBC) (PRESERVE2). NLM identifier: NCT04799249. Cortés J, Kim SB, Chung WP, et al (2022). Trastuzumab deruxtecan versus trastuzumab emtansine for breast cancer. N Engl J Med, 386(12):1143-1154. DOI:10.1056/NEJMoa2115022
- 111. References (cont.) Corti C, Giugliano F, Nicolò E, et al (2021). Antibody-drug conjugates for the treatment of breast cancer. Cancers (Basel), 13(12):2898. DOI:10.3390/cancers13122898 Dent R, Cescon DW, Bachelot T, et al (2022). TROPION-Breast02: phase 3, open-label, randomized study of first-line datopotamab deruxtecan versus chemotherapy in patients with locally recurrent inoperable or metastatic TNBC who are not candidates for anti-PD-(L)1 therapy. Presented at: San Antonio Breast Cancer Symposium 2022. Abstract OT1-03-05. Dent R, Trudeau M, Pritchard KI, et al (2007). Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res, 13(15 Pt 1):4429-4434. DOI:10.1158/1078-0432.CCR- 06-3045 Diéras V, Deluche E, Lusque A, et al (2022). Trastuzumab deruxtecan (T-DXd) for advanced breast cancer patients (ABC), regardless HER2 status: a phase II study with biomarkers analysis (DAISY) [oral presentation]. Cancer Res, 82(suppl_4). Abstract PD8-02. DOI:10.1158/1538-7445.SABCS21-PD8-02 Diéras V, Han HS, Kaufman B, et al (2020). Veliparib with carboplatin and paclitaxel in BRCA-mutated advanced breast cancer (BROCADE3): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol, 21(10):1269-1282. DOI:10.1016/S1470-2045(20)30447-2 Doi T, Patel M, Falchook GS, et al (2022). DS-7300 (B7-H3 DXd antibody-drug conjugate [ADC]) shows durable antitumor activity in advanced solid tumors: extended follow-up of a phase I/II study. Ann Oncol, 33(suppl_7):S197-S224. DOI:10.1016/annonc/annonc1049 Enhertu® (fam-trastuzumab deruxtecan-nxki) prescribing information (2022). Daiichi Sankyo, Ltd. Available at: https://www.enhertuhcp.com/en Fleming PJ Jr, Karpio S, & Lombardo N (2021). Sacituzumab govitecan for treatment of refractory triple-negative metastatic breast cancer. J Adv Pract Oncol, 12(7):747-752. DOI:10.6004/jadpro.2021.12.7.8 Foulkes WD, Smith IE & Reis-Filho JS (2010). Triple-negative breast cancer. N Engl J Med, 363:1938-1948. DOI:10.1056/NEJMra1001389 Gaedcke J, Traub F, Milde S, et al (2007). Predominance of the basal type and HER-2/neu type in brain metastasis from breast cancer. Mod Pathol, 20(8):864-870. DOI:10.1038/modpathol.3800830 Goldenberg DM, Cardillo TM, Govindan SV, et al (2015). Trop-2 is a novel target for solid cancer therapy with sacituzumab govitecan (IMMU-132), an antibody-drug conjugate (ADC). Oncotarget, 6(26):22496-512. DOI:10.18632/oncotarget.4318 Goldenberg DM & Sharkey RM (2020). Sacituzumab govitecan, a novel, third-generation, antibody-drug conjugate (ADC) for cancer therapy. Expert Opin Biol Ther, 20(8):871-885. DOI:10.1080/14712598.2020.1757067
- 112. References (cont.) Hamilton EP, Chaudhry A, Spira AI, et al (2023). XMT-1660: a phase 1b trial of a B7-H4 targeted antibody drug conjugate (ADC) in breast, endometrial, and ovarian cancers. J Clin Oncol, 41(suppl_16). Abstract TPS3154. DOI:10.1200/JCO.2023.41.16_suppl.TPS3154 Hammond MEH, Hayes DF, Wolff AC, et al (2010). American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Oncol Pract, 6(4):195-197. DOI:10.1200/JOP.777003 Handa U, Kumar A, Kundu R, et al (2015). Evaluation of grading and hormone receptor immunostaining on fine needle aspirates in carcinoma breast. J Cytol, 31(1):1-5. DOI:10.4103/0970- 9371.155222 Heist RS, Sands J, Shimizu, et al (2019). First-in-human phase 1 study of DS-1062a (TROP2 antibody-drug conjugate) in patients with advanced non-small cell lung cancer {oral presentation]. 2019 International Association for the Study of Lung Cancer World Conference on Lung Cancer. Abstract MA25.10. Howlader N, Cronin KA, Kurian AW & Andridge R (2018). Differences in breast cancer survival by molecular subtypes in the united states. Cancer Epidemiol Biomarkers Prev, 27(6):619-626. DOI:10.1158/1055-9965.EPI-17-0627 Hurvitz SA, Bardia A, Punie K, et al (2022). Sacituzumab govitecan (SG) efficacy in patients with metastatic triple-negative breast cancer (mTNBC) by HER2 immunohistochemistry (IHC) status: findings from the phase III ASCENT study. Ann Oncol, 33(suppl_3):S200-S201. DOI:10.1016/j.annonc.2022.03.187 Hurvitz SA, Hegg R, Chung WP, et al (2023). Trastuzumab deruxtecan versus trastuzumab emtansine in patients with HER2-positive metastatic breast cancer: updated results from DESTINY- Breast03, a randomised, open-label, phase 3 trial. Lancet, 401(10371):105-117. DOI:10.1016/S0140-6736(22)02420-5 Hurvitz SA, Tolaney SM, Punie K, et al (2021). Biomarker evaluation in the phase 3 ASCENT study of sacituzumab govitecan versus chemotherapy in patients with metastatic triple-negative breast cancer [oral presentation]. Cancer Res, 81(suppl_4): GS3-06. DOI:10.1158/1538-7445.SABCS20-GS3-06 Kaur K, Shah A, Gandhi J & Trivedi P (2022). Mucinous cystadenocarcinoma of the breast: a new entity with broad differentials – a case report. J Egypt Natl Canc Inst, 34:9. DOI:10.1186/s43046-022-00112-9 Kim DJ, Sun WY, Ryu DH, et al (2011). Microglandular adenosis. J Breast Cancer, 14(1):72-75. DOI:10.4048/jbc.2011.14.1.72 Kopp A, Hofsess S, Cardillo TM, et al (2023). Antibody-drug conjugate sacituzumab govitecan drives efficient tissue penetration and rapid intracellular drug release. Mol Cancer Ther, 22(1):102- 111. DOI:10.1158/1535-7163.MCT-22-0375
- 113. References (cont.) Krop IE, Masuda N, Mukohara T, et al (2022). Results from the phase 1/2 study of patritumab deruxtecan, a HER3-directed antibody-drug conjugate (ADC), in patients with HER3-expressing metastatic breast cancer (MBC). J Clin Oncol, 40(suppl_16); 1002-1002. DOI:10.1200/JCO.2022.40.16_suppl.1002 Li Q, Zhang R, Yan H, et al (2017). Prognostic significance of HER3 in patients with malignant solid tumors. Oncotarget, 8(40):67140-67151. DOI:10.18632/oncotarget.18007 Lisberg AE, Sands J, Shimizu T, et al (2020). Dose escalation and expansion from the phase I study of DS-1062, a trophoblast cell-surface antigen 2 (TROP2) antibody drug conjugate (ADC), in patients (pts) with advanced non-small cell lung cancer (NSCLC). J Clin Oncol, 38(suppl_15):9619. DOI:10.1200/JCO.2020.38.15_suppl.9619 Litton JK, Rugo HS, Ettl J, et al (2018). Talazoparib in patients with advanced breast cancer and a germline BRCA mutation. N Engl J Med, 379(8):753-763. DOI:10.1056/NEJMoa1802905 Loibl S, Loirat D, Tolaney SM, et al (2021). Health-related quality of life (HRQoL) in the ASCENT study of sacituzumab govitecan (SG) in metastatic triple-negative breast cancer (mTNBC). Annals of Oncol, 32(suppl_5); 457-515. DOI:10.1016/annonc/annonc689 Marletta S, Fusco N, Munari E, et al (2022). Atlas of PD-L1 for pathologists: indications, scores, diagnostic platforms and reporting systems. J Pers Med, 12(7):1073. DOI:10.3390/jpm12071073 Marmé F, Schmid P, Cortés J, et al (2022). Sacituzumab govitecan (SG) efficacy in hormone receptor-positive/human epidermal growth factor receptor 2-negative (HR+/HER2–) metastatic breast cancer (MBC) by HER2 immunohistochemistry (IHC) status in the phase III TROPiCS-02 study [oral presentation]. ESMO Congress 2022. Abstract 214MO. Marrazzo E, Frusone F, Milana F, et al (2020). Mucinous breast cancer: a narrative review of the literature and a retrospective tertiary single-centre analysis. Breast, 49:87-92. DOI:10.1016/j.breast.2019.11.002 Meisel JL, Pluard TJ, Vinayak S, et al (2022). Phase 1b/2 study of ladiratumzumab vedotin (LV) in combination with pembrolizumab for first-line treatment of triple-negative breast cancer (SGNLVA-002, trial in progress). J Clin Oncol, 40(suppl_16). Abstract TPS1127. DOI:10.1200/JCO.2022.40.16_suppl.TPS1127 Meric-Bernstam F, Oh DY, Naito Y, et al (2022). First-in-human study of the B7-H4 antibody-drug conjugate (ADC) AZD8205 in patients with advanced/metastatic solid tumors. J Clin Oncol, 40(suppl_16). Abstract TPS3153. DOI:10.1200/JCO.2022.40.16_suppl.TPS3153 Miglietta F, Griguolo G, Bottosso M, et al (2021). Evolution of HER2-low expression from primary to recurrent breast cancer. NPJ Breast Cancer, 7(1):137. DOI:10.1038/s41523-021-00343-4
- 114. References (cont.) Min Y, Bae SY, Lee HC, et al (2013). Tubular carcinoma of the breast: clinicopathologic features and survival outcome compared with ductal carcinoma in situ. J Breast Cancer, 16(2):404-409. DOI:10.4048/jbc.2013.16.4.404 Modi S, Jacot W, Yamashita T, et al (2022a). Trastuzumab deruxtecan (T-DXd) versus treatment of physician’s choice (TPC) in patients (pts) with HER2-low unresectable and/or metastatic breast cancer (mBC): Results of DESTINY-Breast04, a randomized, phase 3 study [oral presentation]. J Clin Oncol, 40(suppl 17; abstr LBA3). DOI:10.1200/JCO.2022.40.17_suppl.LBA3 Modi S, Jacot W, Yamashita T, et al (2022b). Trastuzumab deruxtecan in previously treated HER2-low advanced breast cancer. N Engl J Med, 387(1):9-20. DOI:10.1056/NEJMoa2203690 Nagayama A, Vidula N, Ellisen L & Bardia A (2020). Novel antibody-drug conjugates for triple negative breast cancer. Ther Adv Med Oncol, 12:1758835920915980. DOI:10.1177/1758835920915980 Nakada T, Sugihara K, Jikoh T, et al (2019). The latest research and development into the antibody-drug conjugate, [fam-] trastuzumab deruxtecan (DS-8201a), for HER2 cancer therapy. Chem Pharm Bull (Tokyo), 67(3):173-185. DOI:10.1248/cpb.c18-00744 National Comprehensive Cancer Network (2023). Clinical Practice Guidelines in Oncology: breast cancer. Version 4.2023. Available at: https://www.nccn.org/guidelines/guidelines- detail?category=1&id=1419 Nofech-Mozes S, Trudeau M, Kahn HK, et al (2009). Patterns of recurrence in the basal and non-basal subtypes of triple-negative breast cancers. Breast Cancer Res Treat, 118(1):131-137. DOI:10.1007/s10549-008-0295-8 Ocana A, Vera-Badillo F, Seruga B, et al (2013). HER3 overexpression and survival in solid tumors: a meta-analysis. J Natl Cancer Inst; 105(4):266-73. DOI:10.1093/jnci/djs501 Ocean AJ, Starodub AN, Bardia A, et al (2017). Sacituzumab govitecan (IMMU-132), an anti-trop-2-SN-38 antibody-drug conjugate for the treatment of diverse epithelial cancers: safety and pharmacokinetics. Cancer, 123(19):3843-3854. DOI:10.1002/cncr.30789 Okajima D, Yasuda S, Maejima T, et al (2021). Datopotamab deruxtecan, a novel TROP2-directed antibody-drug conjugate demonstrates potent antitumor activity by efficient drug delivery to tumor cells. Mol Cancer Ther, 20(12):2329-2340. DOI:10.1158/1535-7163.MCT-21-0206 Ono M, Bruce JY, Feinstein T, et al (2022). Enfortumab vedotin 202: Phase 2 study of enfortumab vedotin for previously treated advanced solid tumors, including breast cancer. Cancer Res, 82(suppl_4): OT1-02-04. DOI:10.1158/1538-7445.SABCS21-OT1-02-04
- 115. References (cont.) Pareja F, Selenica P, Brown DN, et al (2020). Micropapillary variant of mucinous carcinomas of the breast display genetic alterations intermediate between mucinous carcinomas and micropapillary carcinomas. Histopathology, 75(1):139-145. DOI:10.1111/his.13853 Prat A, Modi S, Tsurutani J, et al (2022). Determination of HER2-low status in tumors of patients with unresectable and/or metastatic breast cancer in DESTINY-Breast04. Presented at: 2022 San Antonio Breast Cancer Symposium. Abstract HER2-8. Robson M, Im SA, Senkus E, et al (2017). Olaparib for metastatic breast cancer in patients with a germline BRCA mutation. N Engl J Med, 377(6):523-533. DOI:10.1056/NEJMoa1706450 Rugo HS, Bardia A, Tolaney SM, et al (2020). TROPiCS-02: A Phase III study investigating sacituzumab govitecan in the treatment of HR+/HER2- metastatic breast cancer. Future Oncol, 16(12):705-715. DOI:10.2217/fon-2020-0163 Rugo HS, Bardia A, Marmé F, et al (2022). Sacituzumab govitecan in hormone receptor–positive/human epidermal growth factor receptor 2–negative metastatic breast cancer J Clin Oncol, 40(29) :3365-3376. DOI:10.1200/JCO.22.01002 Rugo HS, Bianchini G, Cortes, et al (2022). Optimizing treatment management of trastuzumab deruxtecan in clinical practice of breast cancer. ESMO Open, 7(4):100553. DOI:10.1016/j.esmoop.2022.100553 Rugo HS, Cortez T, Cescon DW, et al (2021). KEYNOTE-355: Final results from a randomized, double-blind phase III study of first-line pembrolizumab + chemotherapy vs placebo + chemotherapy for metastatic TNBC. Annals Oncol, 32(suppl_5); 1283-1346. DOI:10.1016/annonc/annonc741 Rugo HS, Tolaney SM, Loirat D, et al (2021). Impact of UGT1A1 status on the safety profile of sacituzumab govitecan in the phase 3 ASCENT study in patients with metastatic triple-negative breast cancer. Cancer Res, 81(suppl_4). Abstract PS11-09. DOI:10.1158/1538-7445.SABCS20-PS11-09 Rugo HS, Tolaney SM, Loirat D, et al (2022). Safety analyses from the phase 3 ASCENT trial of sacituzumab govitecan in metastatic triple-negative breast cancer. NPJ Breast Cancer, 8(1):98. DOI:10.1038/s41523-022-00467-1 Sands JM, Shimizu T, Garon EB, et al (2018). First-in-human phase 1 study of DS-1062a in patients (pts) with advanced solid tumors (AST). J Clin Oncol, 36(suppl_15). Abstract TPS2605. DOI:10.1200/JCO.2018.36.15_suppl.TPS2605 Schettini F, Chic N, Brasó-Maristany, et al (2020). Clinical, pathological and gene expression features of HER2-low breast cancer. Ann Oncol, 31(suppl_2):S24. DOI:10.1016/j.annonc.2020.03.159
- 116. References (cont.) Schmid P, Cortes J, Dent R, et al (2021). KEYNOTE-522 study of neoadjuvant pembrolizumab + chemotherapy vs placebo + chemotherapy, followed by adjuvant pembrolizumab vs placebo for early-stage TNBC: Event-free survival sensitivity and subgroup analyses [oral presentation]. 2021 San Antonio Breast Cancer Symposium. Abstract GS1-01. Spira A, Lisberg A, Sands J, et al (2021). Datopotamab deruxtecan (Dato-DXd; DS-1062), a TROP2 ADC, in patients with advanced NSCLC: updated results of TROPION-PanTumor01 phase 1 study. J Thoracic Oncol, 16(suppl_3). Abstract OA03.03. Spring LM, Nakajima E, Hutchinson J, et al (2021). Sacituzumab govitecan for metastatic triple-negative breast cancer: clinical overview and management of potential toxicities. Oncologist, 26(10):827-834. DOI:10.1002/onco.13878 Stankowicz M, Mauro L, Harnden K, et al (2021). Management of chemotherapy-induced nausea and vomiting with trastuzumab deruxtecan: a case series. Breast Care (Basel), 16(4):408-411. DOI:10.1159/000511049 Swain SM, Nishino M, Lancaster LH, et al (2022). Multidisciplinary clinical guidance on trastuzumab deruxtecan (T-DXd)-related interstitial lung disease/pneumonitis-Focus on proactive monitoring, diagnosis, and management. Cancer Treat Rev, 106:102378. DOI:10.1016/j.ctrv.2022.102378 Taqi SH, Sami SA, Sami LB & Zaki SA (2018). A review of artifacts in histopathology. J Oral Maxillofac Pathol, 22(2):279. DOI:10.4103/jomfp.JOMFP_125_15 Trodelvy® (sacituzumab govitecan-hziy) prescribing information (2023). Gilead Sciences, Inc. Available at: https://www.trodelvyhcp.com/ Tung NM, Robson ME, Ventz S, et al (2020a). TBCRC 048: phase II study of olaparib for metastatic breast cancer and mutations in homologous recombination-related genes. J Clin Oncol, 38(36):4274-4282. DOI:10.1200/JCO.20.02151 Tung NM, Robson ME, Ventz S, et al (2020b). TBCRC 048: phase II study of olaparib for metastatic breast cancer and mutations in homologous recombination-related genes [oral presentation]. ASCO Annual Meeting 2020. Abstract 1002. Ueno NT, Jacot W, Yamashita T, et al (2022). Patient-reported outcomes (PROs) from DESTINY-Breast04, a randomized phase III study of trastuzumab deruxtecan (T-DXd) vs treatment of physician's choice (TPC) in patients (pts) with HER2-low metastatic breast cancer (MBC). Annals of Oncol, 33(suppl_7); 88-121. DOI:10.1016/annonc/annonc1040 US Food & Drug Administration (2018). FDA approves talazoparib for gBRCAm HER2-negative locally advanced or metastatic breast cancer. Available at: https://www.fda.gov/drugs/drug- approvals-and-databases/fda-approves-talazoparib-gbrcam-her2-negative-locally-advanced-or-metastatic-breast-cancer
- 117. References (cont.) US Food & Drug Administration (2021). FDA grants regular approval to sacituzumab govitecan for triple-negative breast cancer. Available at: https://www.fda.gov/drugs/resources-information- approved-drugs/fda-grants-regular-approval-sacituzumab-govitecan-triple-negative-breast-cancer Vidula N, Yau C, & Rugo H (2017). Trop2 gene expression (Trop2e) in primary breast cancer (BC): Correlations with clinical and tumor characteristics. J Clin Oncol, 35(suppl_1075). DOI:10.1200/JCO.2017.35.15_suppl.1075 Wolff AC, Hammond MEH, Allison KH, et al (2018). Human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline focused update. J Clin Oncol, 36(20):2105-2122. DOI:10.1200/JCO.2018.77.8738.
