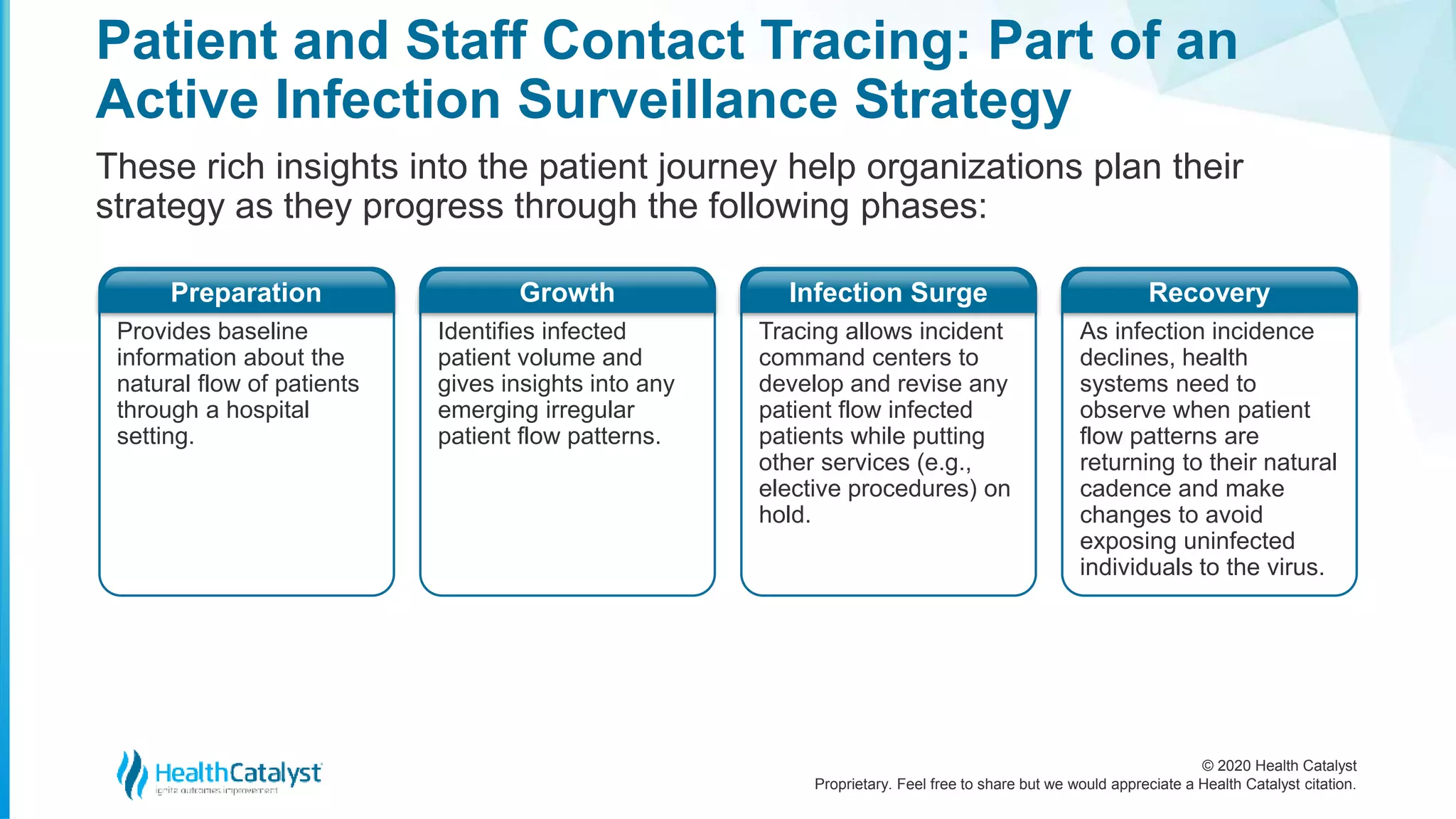
The document outlines steps for effective patient and staff contact tracing to manage the spread of COVID-19, emphasizing the importance of tracking interactions and movements to inform testing and quarantine efforts. It introduces Health Catalyst's Patient and Staff Tracker, a tool designed to enhance contact tracing by providing analytical insights into patient interactions within healthcare facilities. The document highlights the significance of integrating contact tracing into broader infection surveillance strategies for both immediate response and future preparedness in healthcare settings.