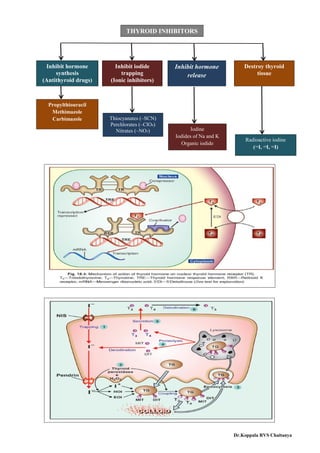
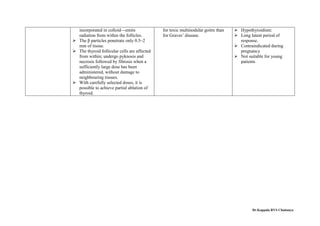
The document provides an extensive overview of thyroid hormones, including their synthesis, regulation, and pharmacological actions. It explains the roles of thyroxine (T4) and triiodothyronine (T3) in metabolism, growth, and development, as well as the effects of thyroid inhibitors and antithyroid drugs. Additionally, it details the therapeutic uses of thyroid hormones and the complications associated with their management.