DIGESTIVE SYSTEM
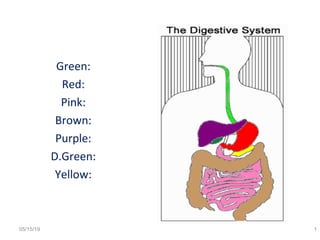
- 2. How’d you do? 05/15/19 2 • Green: Esophagus • Red: Stomach • Pink: Small Intestine • Brown: Large Intestine • Purple: Liver • D.Green: Gall Bladder • Yellow: Pancreas
- 4. 05/15/19 4
- 5. • The GI tract (gastrointestinal tract) The alimentary canal – Mouth – Pharynx – Esophagus – Stomach – Small intestine – Large intestine – Anus • The accessory digestive organs Supply secretions contributing to the breakdown of food – Teeth & tongue – Salivary glands – Gallbladder – Liver – Pancreas 05/15/19 5
- 6. Processes of Digestive system 1. Ingestion 2. Secretion 3. Mixing and propulsion (pushing forwards). 4. Mechanical and Chemical Digestion 5. Absorption 6. Elimination
- 7. • Ingestion – Taking in food through the mouth • Propulsion (movement of food) – Swallowing – Peristalsis – propulsion by alternate contraction &relaxation • Mechanical digestion – Chewing – Churning(agitation/shaking) in stomach – Mixing by segmentation • Chemical digestion – By secreted enzymes • Absorption – Transport of digested end products into blood and lymph • Defecation – Elimination of indigestible substances from body as feces 05/15/19 7
- 8. 05/15/19 8
- 9. Basic Four layer Arrangement of tissues of GI tract • Four layers from deep to superficial Mucosa Submucosa Muscularis Serosa 05/15/19 9
- 10. Histology of alimentary canal wall Same four layers (esophagus to anal canal) 05/15/19 10
- 11. 1.Mucosa (Innermost) 05/15/19 11 1. Layer of epithelium (Innermost) 2. Layer of connective tissue (Lamina propia) 3. Layer of smooth muscle (Muscularis mucosae)
- 12. • Epithelium: Mouth, pharynx, esophagus and anal canal : Nonkeratinised squamous epth.(protective functn) Stomach and intestine: Columnar epithelium (Secretory function) Tight junctions firmly seal neighbouring simple columnar (Restricts leakage between the cells) Rate of renewal of GI tract epithelial cells is rapid. Among epithelial cells are exocrine cells(secrete mucus &fluid in the lumen) and endocrine (secrete hormones) 05/15/19 12
- 13. • Lamina Propria: Aerolar connective tissue, contains blood and lymphatic vessels. Supports epithelium and binds it to muscularis mucosa Also contains majority of cells of MALT(Mucosa associated lymphatic tissue) Contains immune system cells. MALT is present all along GI tract, especially in Tonsils, S.I, Appendix and L.I 05/15/19 13
- 14. • Muscularis Mucosae: Thin layer of smooth muscle fibres. Mucous membrane of stomach and small intestine has many small folds (Digestion and Absorption) Movement of muscularis mucosae ensures that all absorptive cells are exposed to contents of GI tract. 05/15/19 14
- 15. 2. Sub mucosa 05/15/19 15
- 16. Submucosa is made up of Aerolar connective tissue. It binds mucosa to the muscularis. It contains many blood vessels, glands and lymphatic tissue. It has presence of submucosal plexus (extensive network of neurons) 05/15/19 16
- 17. 3. Muscularis 05/15/19 17 Two layers of smooth muscle responsible for peristalsis and segmentation • Inner circular layer (circumferential) – Squeezes – In some places forms sphincters (act as valves) • Outer longitudinal layer: shortens gut
- 18. 05/15/19 18
- 19. • Muscularis: Muscularis of mouth, pharynx and superior and middle part of esophagus contains skeletal muscle. (voluntary swallowing) Also forms external anal sphincter (permits voluntary control of defecation) Rest of tract, muscularis consists of smooth muscle generally found in 2 sheets, inner sheet of Circular fibres and outer longitudinal fibres. Between the layers of muscularis is second plexus- mysenteric plexus. (major nerve supply to the gastrointestinal tract and controls GI tract motility ) 05/15/19 19
- 20. Serosa : Outermost Layer 05/15/19 20 Portion of GI tract that are suspended in abdominopelvic cavity have superficial layer called serosa Composed of areolar connective tissue and simple squamous epithelium also called visceral peritoneum Esophagus lacks serosa, instead single layer of aerolar connective tissue called adventitia forms superficial layer of the organ.
- 21. Peritoneum • Largest Serous membrane of the body • Layer of simple squamous epithelium with underlying aerolar connective tissue. • Peritoneum: 1. Parietal (lines the wall of abdominopelvic cavity) 2. Visceral (covers some organs in the cavity) Space between parietal and visceral portion of peritoneum is peritoneal cavity contains serous fluid. Some organs lie on the posterior abdominal wall and are covered by peritoneum only on their anterior surfaces. Such organs are retro(behind)peritoneal (kidneys and pancreas)05/15/19 21
- 22. 05/15/19 22
- 24. Mouth: Oral or buccal Cavity • Formed by Cheeks, hard palate and soft palate and tongue. • Cheeks: Form lateral walls of the oral cavity. Covered externally by skin and internally by mucous membrane. (nonkeratinised squa ep) • Buccinator muscles and connective tissue between skin and mucous membrane. • Lips or labia are fleshy folds surrounding opening of the mouth- orbicularis muscle. • Inner surface of each lip is attached to corresponding gum by midline fold of mucous membrane called labia frenulum 05/15/19 24
- 25. Function: During chewing, contraction of buccinator muscles in the cheeks and orbicularis oris muscle in the lips helps keep food between upper and lower teeth. Also assist in speech. Vestibule: of the oral cavity is space bounded externally by cheeks and lips and internally by gums and teeth. Fauces is opening between oral cavity and pharynx. Hard Palate: Anterior portion of the roof of the mouth. Formed by maxillae and palatine bones covered by mucous membrane. Bony partition between oral and nasal cavity. 05/15/19 25
- 26. Soft Palate: Posterior portion of the roof of the mouth. Arch shaped muscular partition between oropharynx and nasopharynx. Hanging from the free border of soft palate is conical muscular process called uvula. Function: During swallowing, the soft palate and uvula are drawn upward, closing off nasopharynx and preventing swallowed food to enter the nasal cavity. Video 05/15/19 26
- 27. • Lateral to the base of uvula are 2 muscular folds that run down lateral sides of soft palate. 1. Palatoglossal arch: Anterior, extends to the side of base of tongue 2. Palatopharyngeal arch: Posterior, extends to the side of pharynx Palatine tonsils are situated between the arches. 05/15/19 27
- 29. Gland that secretes a secretion called as saliva into oral cavity. Function: 1.Keeps the mucous membranes of mouth and pharynx moist 2. Cleanses mouth and teeth 3. Lubricates, dissolves and begins chemical breakdown of food 05/15/19 29
- 30. • Salivary Gland lies beyond oral mucosa, drains saliva into ducts and leads to oral cavity. 3 pairs of major salivary gland: 1.Parotid (near to ear) Inferior and anterior to ear Each secrete saliva into oral cavity via parotid duct that pierces Buccinator muscle to open into vestibule opposite upper molar teeth. 2. Submandibular gland (Floor of mouth) Medial and partly inferior to the body of mandible Submandibular ducts run under mucosa on either side of midline of the floor of mouth and enter the oral cavity lateral to lingual frenulum 05/15/19 30
- 31. • Sublingual glands: (Beneath the tongue): Superior to Submandibular glands. Sublingual duct open into the floor of mouth in the oral cavity. Structure of salivary glands: Consists of several lobules made from acini ( the functional unit of the exocrine pancreas)lined with secretory cells. Secretions poured into ductules, which join to form large ducts leading into mouth. Diagram 05/15/19 31
- 32. 05/15/19 32
- 33. Composition of Saliva • 99.5% water, 0.5% Solutes (Na+ , K+ , Cl- , HCo3- , PO4- ) , dissolved gases, various organic substances urea, uric acid, mucus, IGA, lysozyme, salivary amylase • Water: Dissolves food, sensed by gustatory receptors (Digestion begins) • Chloride: Activates salivary amylase • Bicarbonates and phosphate ions: Buffers acidic food. • Salivary pH: 6.35 to 6.85 05/15/19 33
- 34. • Urea & Uric acid: helps to remove waste in saliva • Mucus: Lubrication of food • IGA: Prevents attachment of microbes, cannot penetrate the epithelium • Lysozyme: Kills bacteria Salivation is controlled by Autonomic nervous system Parasympathetic stimulation promotes continuous secretion of saliva Sympathetic stimulation dominates during stress, results in dryness of mouth 05/15/19 34
- 35. 05/15/19 35 Salivary glands (stops saliva secretion) Body is dehydrated Dryness of mouth Sensation of thirst
- 36. Tongue • Skeletal muscle covered by mucous membrane consists of intrinsic and extrinsic muscles. • Extrinsic muscles: originates outside the tongue and insert in the connective tissue of tongue. • Hypoglossus, genioglossus, styloglosssus muscles Function: Extrinsic muscles move tongue from side to side and in and out to maneuver(careful movemt) food for chewing , shape the food, force food to the back of the mouth for swallowing and hold the tongue in position.05/15/19 36
- 37. • Instrinsic Muscles: originates inside and insert in connective tissue. • These muscles alter the shape and size of the tongue for speech and swallowing. • Longitudnalis superior, Longitudnalis inferior, transversus linguae and verticalis linguae muscle • Lingual frenulum: Fold of mucous membrane in the midline of undersurface of the tongue. Aids in limiting the movement of the tongue posteriorly. 05/15/19 37
- 38. Tongue • The upper surface and the lateral surface of the tongue are covered with papillae, projections of lamina propia covered with non keratinised squamous epithelium. • Papillae contains taste buds, contain receptors for touch and also increases the friction between tongue and food making it easier for tongue to move food in the oral cavity. • Lingual glands in the tongue secrete mucous and serous fluid containing lingual lipase 05/15/19 38
- 39. Four varieties of papillae 05/15/19 39 1.Vallate: Inverted V shaped. Towards the base of the tongue. Between 8-12 2.Fungiform: Situated at the edges. More than Vallate in number. 3. Filliform: Situated in the anterior 2/3 rd of the tongue. Smallest and numerous 4. Foliate: small trenches, lateral margins
- 41. Functions of the tongue • Mastication(chewing) • Deglutition (swallowing) • Speech(ability to speak) • Taste 05/15/19 41
- 42. TEETH • Accessory digestive organ embedded in the sockets of the alveolar ridges of the mandible and maxillae. • Alveolar processes covered by gingivae (gums) which extend slightly into each socket. • Each individual has 2 set of dentitions, the temporary or deciduous teeth and the permanent. • At birth, both the sets are present in immature form. 05/15/19 42
- 43. • There are 20 temporary teeth, 10 in each jaw. • Dentition consisting of 32 teeth is usually completed by 24th year. Structure of a tooth: Shape of different teeth vary but the structure is the same. 05/15/19 43
- 44. 05/15/19 44
- 45. 05/15/19 45
- 46. Structure of the Tooth 05/15/19 46
- 47. Structure of tooth consists of: 1. The Crown: Part which protrudes from the gum 2.The Root: The part embedded in the bone 3. The neck: The slightly narrowed region where the crown merges with the root In the centre of the tooth is the pulp cavity containing blood vessels, nerves and lymph vessels. Surrounding there is a hard ivory like substance called dentine. Outside the dentine of the crown is a thin layer of hard substance , the enamel05/15/19 .47
- 48. • The root of the tooth is covered with substance resembling bone called cement which fixes the tooth in the sockets • Pulp cavity lies with in crown filled with pulp, connective tissue containing blood vessels, nerves and lymphatic vessels. • Narrow extensions of pulp cavity called root canals run through the root of the tooth. • Each root canal has an opening at its base (apical foramen) through which blood, lymphatic vessels and nerves extended. 48
- 49. • Blood vessels bring nourishment and nerve provide sensation, lymphatic offers protection. Function: • Incisors and Canine : Cutting teeth • Premolars and Molars: Broad surfaces, grinding and chewing. 05/15/19 49
- 50. Pharynx • Mouth Throat (Pharynx) Composed of skeletal muscle and lined by mucous membrane. It is divided into 3 parts: Nasopharynx: Functions only in respiration Oropharynx Muscular contraction of Laryngopharynx these areas help to propel food into esophagus05/15/19 50
- 51. • Esophagus (eating gullet):- is a collapsible muscular tube- 25 cms long and about 2cms in diameter and lies in the median plane in the thorax in front of the vertebral column behind trachea and the heart Continues with pharynx above and just below diaphragm it forms the stomach It passes between muscle fibres of the diaphragm behind central tendon at the level of 10 th thoracic vertebra 05/15/19 51
- 52. • Immediately, the esophagus has passed through the diaphragm, it curves upwards before opening into the stomach. • This sharp angle is believed to be one of the factors which prevents the regurgitation of gastric contents into esophagus • The upper and lower ends of esophagus are closed by the sphincter muscles • Upper sphincter prevents air passing into esophagus during inspiration and aspiration of esophageal contents • Lower esophageal sphincter prevents reflux of acid, gastric contents into esophagus05/15/19 52
- 53. Structure: Four layers of tissue: Outer Adventitia: Consists of elastic fibrous tissue. Proximal third is lined by stratified squamous epithelium. Distal third by columnar epithelium. The middle third is lined by a mixture of the two. Function of Pharynx and esophagus: Formation of bolus Food is masticated by teeth, moved around by tongue and muscles of cheeks, mixed with saliva and formed into soft mass for swallowing 05/15/19 53
- 54. Swallowing(Deglutition) occurs in 3 steps: 1.Mouth is closed and voluntary muscles of tongue and cheeks push the bolus backward into the pharynx 2.The muscles of pharynx are stimulated by a reflex action initiated in the walls of Oropharynx and coordinated in medulla and lower pons in the brain stem. Contraction of muscles propel the bolus down into the esophagus. Soft palate rises up and closes off the Nasopharynx, the tongue and pharyngeal fold blocks the way back into mouth. 05/15/19 54
- 55. 3.Presence of bolus in pharynx stimulates a wave of peristalsis which propels the bolus through esophagus to the stomach. Stomach: J shaped enlargement of GI tract situated in the epigastric, umbilical and left hypochondriac region of the abdomen. It serves as a mixing chamber and holding reservoir . Digestion of proteins and triglyceride starts and the semisolid bolus is converted to a liquid and certain substances are absorbed. 05/15/19 55
- 56. • Anatomy of stomach Cardia: Surrounds the superior opening of the stomach Fundus: Rounded portion superior to and to the left of the Cardia Body: Inferior to the Fundus is the large portion of stomach Pylorus: Region of stomach that connects to duodenum 05/15/19 56
- 57. • Pyloric Antrum: Connects to the body of stomach • Pyloric Canal: Leads to duodenum When the stomach is empty, the mucosae lies in large folds called rugae.(wrinkles) Pylorus communicates with duodenum of small intestine via smooth muscle sphincter called pyloric sphincter Concave medial border is lesser curvature Convex lateral border is greater curvature 05/15/19 57
- 58. 05/15/19 58
- 59. 05/15/19 59 *** Histology of stomach
- 60. Histology of stomach Four layers of tissue that comprises the basic structure of GI are found in stomach with some modifications •Mucosa: Simple columnar cells •Lamina Propria: Aerolar connective tissue •Muscularis Mucosae: Smooth muscle Muscle layer: Consists of 3 layers of smooth muscle instead of 2 found in S.I, L.I, Esophagus. Outer layer of longitudinal fibres Middle layer of circular fibres Inner layer of oblique fibres05/15/19 60
- 61. Circular muscle is strongest in the pyloric antrum and sphincter. Arrangement of muscles allows for churning motion. Epithelial cells extend down into lamina propria, where they form columns of secretory glands called gastric glands. Secretions from gastric glands flow into each gastric pits (gastric glands open into the bottom of the narrow channel called gastric pits) and then into the lumen of the stomach 05/15/19 61
- 62. Gastric glands contains 3 types of exocrine gland cells: •Mucous neck cells: Secrete mucus •Chief cells: secrete Pepsinogen and gastric lipase •Parietal cells: Secrete Hcl and intrinsic factor needed for absorption of Vit B12 Secretion from mucus, chief and parietal cells forms gastric juice. In addition gastric glands include type of enteroendocrine cells (G cells) which secrete hormone gastrin into blood stream. 05/15/19 62
- 63. • Gastrin: Stimulates parietal cells to secrete Hcl and chief cells for Pepsinogen, contract lower esophageal sphincter, relaxes pyloric sphincter and increases stomach motility. • Composition and function of gastric juice:- Water: Liquefies food further after it is swallowed Hcl: Acidifies food and inactivates salivary amylase Kills ingested microbes, Activation of Pepsinogen 05/15/19 63
- 64. Pepsinogen: Digestion of proteins (Pepsin) Intrinsic factor: Absorption of Vit B12 Mucus: Protection from Mechanical injury by lubricating the contents of the stomach. Chemical injury: Barrier between the stomach walls and juices. Mucous cells of stomach absorb some water, ions, short chain fatty acid as well as alcohol and aspirin. 05/15/19 64
- 65. Mechanical and chemical digestion in stomach 05/15/19 65 Digestion proceeds Food enters Stomach Mixing waves pass over every 15 to 25 secs Peristalsis Maceration of food. Mixing with secretions Vigorous mixing begins at body and intensifies at pylorus Pyloric spincter is almost closed Food reaches pyrolus Most of the chyme is forced back into stomach where mixing continues Gastric emptying Mixing wave forces and moves food into duodenum *Mixing wave periodically force 3 ml of chyme into duodenum *
- 66. • Food remains in the Fundus for about an hour without becoming mixed with gastric juice. During this time, digestion with salivary amylase continues. • Churning activity mixes food with acidic gastric juices inactivating salivary amylase and activating lingual lipase which starts to digest triglycerides into fatty acids and diglycerides. • Within 2 – 4 hrs after eating , stomach empties its contents into duodenum. 05/15/19 66
- 67. Secretion of HCl: Parietal cells secrete H + ions separately in stomach lumen, the net effect is secretion of Hcl Proton pump powered H+ /K+ ATPases actively transports H+ into lumen while bringing K+ ions into the cell. At the same time, Cl- and K+ ions diffuse out into the lumen through Cl- and K+ channels Enzyme carbonic anhydrase (plentiful in parietal cells) catalyze formation of carbonic acid from H2O and CO2 05/15/19 67
- 68. • H2O + CO2 Carbonic acid dissociates and provides ready source of H+ for proton pump but also generates bicarbonate ions HCO3 - Carbonic acid dissociates and provide ready source of H+ for proton pump but also generates bicarbonate ions (HCO3 - ) HCO3 - exits the parietal cells in exchange for Cl- via Cl- / HCO3 - Antiporters in basolateral membrane next to lamina propria. HCO3 - diffuses into nearby capillaries. 05/15/19 68 H2CO3 H+ + HCO3 -
- 69. 05/15/19 69
- 70. Function of Stomach: 1. Chemical Digestion: Pepsin converts protein to polypeptides 2. Mechanical Breakdown: Churning action: Gastric juice is added and contents are liquefied. 3. Limited absorption of water, alcohol and some drugs. 4. Non specific defense against microbes due to Hcl in gastric juice 5. Production and secretion of intrinsic factor 6. Temporary storage, allowing time for digestive enzyme to act. 05/15/19 70
- 71. Acessory Organs: Not part of the path of food, but play a critical role. Pancreas , Liver, gall bladder 05/15/19 71
- 72. Pancreas Pancreas is a retroperitoneal gland 12-15 cms long,2.5 cm thick lies posterior to greater curvature of the stomach. Pancreas consists of head, body and tail and is usually connected to duodenum by 2 ducts. Head is expanded portion of the organ. Superior to and to the left of the head are central body and tapering tail Pancreas is both exocrine and endocrine gland 05/15/19 72
- 73. Exocrine Pancreas: Consists of large number of lobules made up of small alveoli, the walls of which consists of secretory cells. Each lobi is drained by a tiny duct and these unite eventually to form pancreatic duct which opens into duodenum. 05/15/19) 73
- 74. 05/15/19 74 There are two ducts; 1. Pancreatic duct (Wirsung duct) Joins common bile duct to duodenum as common duct. 2. Accessory duct (Santorini) Joins pancreas to duodenum superior to ( hepatopancreatic ampulla) common duct.
- 75. • Functions of Exocrine pancreas is to produce pancreatic juice containing enzyme to digest carbohydrates, proteins and fats. Parasympathetic stimulation increases secretion Sympathetic stimulation decreases secretion. Endocrine Pancreas: Distributed throughout the gland are the group of specialized cells called pancreatic islets of Langerhans. Islets have no ducts so hormones diffuse directly into the blood. Secrete insulin and Glucagon, somatostatin and pancreatic polypeptide05/15/19 75
- 76. Histology of Pancreas: Pancreas is made up of small clusters(group/bunch) of glandular epithelial cells. About 99 % of clusters are called acini, constitute the exocrine portion of the organ. The cell within the acini secrete pancreatic juice remaining 1% of clusters are called pancreatic islets form the endocrine portion of the pancreas. 05/15/19 76
- 77. Composition of Pancreatic juices: Pancreas produces 1.2 L to 1.5 L of pancreatic juice daily. Consists of water, some salts, sodium bicarbonate and several enzymes Sodium bicarbonate gives pancreatic juice slightly alkaline pH (7.1 – 8.2) that buffers acidic gastric juices in the chyme, stops activation of pepsin from the stomach and creates proper pH for activation of enzymes in S.I 05/15/19 77
- 78. Enzymes: 1.Pancreatic amylase (Starch Digesting) 2.Trypsin (Protein digesting) Chymotrypsin, Elastase, carboxypeptidase 3. Pancreatic lipase (Lipid digesting) 4. Ribonuclease and Deoxyribonuclease (Nucleic acid digesting Trypsin is secreted in inactive form-Trypsinogen. Pancreatic acinar cells secrete a protein Trypsin inhibitor which combines with Trypsin formed accidently in the pancreas and block its enzymatic activity.05/15/19 78
- 79. • In the lumen of small intestine, it encounters an activating brush border enzyme (Brush border enzymes are the digestive enzymes located in the membrane of microvilli on intestinal epithelial cells) called enterokinase which splits off part of Trypsinogen molecule to form Trypsin. • In turn Trypsin acts on chymotrypsinogen, procarboxy peptidases and Proelastases to produce Chymotrypsin, carboxypeptidase and Elastase respectively. 05/15/19 79
- 80. Liver: Largest and heaviest gland in the body. It is situated in upper part of abdominal cavity. Its upper surface and anterior surfaces are smooth and curved and fit the under surface of the diaphragm. Its posterior surface is irregular in outline. Liver has four lobes: 1.Largest right lobe 2. Smaller left lobe The other two, the caudate and quadrate lobes are seen on the posterior surface05/15/19 80
- 82. Liver is enclosed in a thin inelastic capsule and incompletely covered by a layer of peritoneum. Peritoneum forms supporting ligaments attaching liver to the inferior surface of the diaphragm. It is held in position partly by this ligament and partly by the pressure of organs in the abdominal cavity. 05/15/19 82
- 83. 1.Portal Fissure: is the posterior surface of the liver where various structures enter and leave the gland 2.Portal Vein: Carrying blood from stomach, spleen, pancreas and small intestine and large intestine •Hepatic artery : carrying arterial blood •Right and left hepatic ducts carrying bile from liver to gall bladder. 05/15/19 83
- 84. Histology of liver 05/15/19 84
- 85. 05/15/19 85
- 86. Structure: The lobe of the liver are made up of tiny functional units called lobules. Liver lobules are hexagonal in shape and are formed by cubical shaped cells, the hepatocytes arranged in pair of columns radiating from central vein. Between 2 pairs of the column cells are sinusoids (A liver sinusoid is a type of sinusoidal blood vessel (with fenestrated, discontinuous endothelium) that serves as a location for mixing of the oxygen-rich blood from the hepatic artery and the nutrient-rich blood from the portal vein) containing blood from tiny branches of the portal vein and hepatic artery. This arrangement allows arterial blood and portal venous blood to mix and come in contact with the liver cells. 05/15/19 86
- 87. Amongst the cells lining the sinusoids are hepatic macrophages(Kupffer cells) whose function is to ingest and destroy worn out blood cell and any foreign particles present in the blood flowing through the liver. Blood drains from the sinusoids into central vein. These then join with the veins from the other lobules forming larger veins which leave liver and empty into inferior vena cava. Bile Canliculi run between the columns of liver cells. These canliculi join up to form larger bile canals until eventually they form the right and left hepatic ducts which drain bile from liver.05/15/19 87
- 88. Functions of liver:*** 1. Carbohydrate metabolism: Liver has an important role in maintaining plasma glucose levels. After meal, when glucose level rises, glucose is converted to glycogen for storage under influence of insulin. Glucose levels falls, hormone glucagon stimulates conversion of glycogen into glucose again keeping glucose levels in the normal range. 05/15/19 88
- 89. 2. Fat metabolism: Stored fat is converted into fat, which can be used by the tissues to provide energy, synthesizes cholesterol to bile salts, synthesize lipoproteins, transports fatty acids, TGs and cholesterol to and from body cells. 3. Protein Metabolism: Deamination of amino acids: Removes nitrogenous portion of amino acids. Urea formed is excreted in urine. Breakdown of nucleic acid to form uric acid. 05/15/19 89
- 90. • Trasamination: Removes the nitrogenous portion of amino acids and attaches it to other carbohydrate molecule forming non essential amino acids. Synthesis of plasma and most blood clotting factors from amino acids 4. Breakdown of erythrocytes and defense against microbes carried out by the phagocytic hepatic macrophages in sinusoids 5. Detoxification of drugs and noxious substances e.g., Alcohol, Penicillin 05/15/19 90
- 91. 6. Processing of hormones: Insulin, glucagon,aldosterone chemically alter/excrete thyrohormone and steroid hormone. 7. Secretion of Bile: Hepatocytes secrete constituent of bile (bile salt) 8. Storage of Glycogen, fat soluble vitamins A, D, E, K, Iron, copper, some water soluble vitamins 9. Activation of Vit D: Skin, liver and kidney synthesize active form of Vit D 05/15/19 91
- 92. • Composition of bile:- 500 ml of bile is secreted by liver daily. Consists of water, mineral salts, mucus, bile pigments mainly bilirubin, bile salts, cholesterol Bile acids, cholic, chenodeoxycholic acid are synthesized by hepatocytes from cholesterol conjugated with either glycine or laurine and then secreted into bile as Na+ and K+ salts In small intestine , they emulsify fats aiding their digestion. In terminal ileum, most bile salts are reabsorbed and return to liver in the portal vein.05/15/19 92
- 93. • The enterohepatic circulation ensures the large amounts of bile salts enter small intestine daily from relatively small bile acid pool. • Bilirubin is one product of hemolysis of erythrocytes by hepatic macrophages in liver and by other macrophages in spleen and bone marrow. • Bilirubin is insoluble in water and is carried in the blood bound to albumin. • In hepatocytes, it is conjugated with Glucuronic acid and becomes water soluble before excretion in bile. 05/15/19 93
- 94. • Bacteria in the intestine change the form of bilirubin excreted as stercobilin in faeces and urobilinogen in urine. • Jaundice is caused by excess blood bilirubin. BILE DUCT: Right and left hepatic ducts form common hepatic duct by joining just outside the portal fissure. Hepatic duct passes downwards, where it joined at an acute angle by cystic duct from gall bladder05/15/19 94
- 95. • Cystic duct and hepatic duct merge forming common bile duct which passes down wards behind the head of pancreas. Structure: Walls of bile ducts: same layers as GI. In the cystic duct, the mucous membrane lining is arranged in irregular circular folds, which have its effect of a spiral valve. Bile passes cystic duct twice, once on the way in gall bladder and again when it is expelled from the gall bladder in the common bile duct and then on to the duodenum.05/15/19 95
- 97. • Gall bladder is a pear shaped sac attached to the posterior surface of the liver by connective tissue. It has fundus or expanded end, a body or main part and a neck which is continuous with cystic duct. • Structure: Same layers as GI with some modifications. Peritoneum covers only the inferior surface Gall bladder is in contact with the right lobe of the liver and is held in place by visceral peritoneum of the liver 05/15/19 97
- 98. •Muscle layer: additional layer of oblique muscle fibre •Mucous membrane displays small rugae when the bladder is empty that disappears when it is distended with bile. •Functions: •Reservoir of bile •Concentration of bile by upto10 or 15 folds, by absorption of water through the walls of the gall bladder •Release of stored bile 05/15/19 98
- 99. • Muscle wall of gall bladder contracts, bile passes through the bile duct to duodenum • Contraction is stimulated by Hormone cholecystokinin, secreted by duodenum Presence of fat and acid chyme in the duodenum. 05/15/19 99
- 100. Small Intestine *** 05/15/19 100
- 101. Small Intestine Most digestion and absorption of nutrients occurs in long tube called small intestine. Its length alone provides a large surface area for digestion and absorption and that area is further increased by circular folds, Villi, microvilli. It begins at the pyloric sphincter of the stomach, coils through the central and the inferior part of the abdominal cavity and eventually opens into the large intestine. 05/15/19 101
- 102. Anatomy of Small Intestine: Small intestine is divided into 3 regions: Duodenum, the shortest region, It starts at pyloric sphincter of stomach and extends until it merges with jejunum Jejunum: Abt 3 ft long and extends to ileum Ileum: The final and longest region of the small intestine, joins the large intestine at smooth muscle sphincter 05/15/19 102
- 103. 05/15/19 103
- 104. 05/15/19 104
- 105. Histology of Small Intestine: Walls of small intestine is composed of the same four layers that make up most of GI tract 1.Mucosa: Composed of a layer of epithelium, lamina Propia and muscularis mucosae Epithelial layer: simple columnar cells containing many cells: 1.Absorptive cells of epithelium digest and absorb nutrients in the intestinal Chyme 2.Mucus secreting goblet cells are also present in epithelium 05/15/19 105
- 106. 3. The SI mucosa, contains deep crevices lined with glandular epithelium, cells lining the crevices form intestinal glands (Crypts of Liberkuhn) and secrete intestinal juices 4. Besides absorptive cells and goblet cells , the intestinal glands also contain paneth cells and endo endocrine cells. Paneth cells secrete lysozyme, a bactericidal and are capable of Phagocytosis. 05/15/19 106
- 107. Three types of enteroendocrine cells are found in intestinal glands of the SI S cells, CCK cells, K cells which secrete hormone secretin, cholecystokinin or CCK and glucose dependant insulin tropin peptide respectively Lamina Propia of the small intestine mucosae contains Aerolar connective tissue and has abundance of MALT. Solitary lymphatic nodules are most numerous in the distal part of the ileum. Group of lymphatic nodules referred to as aggregated lymphatic follicles(Peyers patch) are also present in ileum 05/15/19 107
- 108. • Muscularis mucosae of SI consists of smooth muscle • Sub mucosa of duodenum contains duodenal gland (Brunner's gland) which secrets alkaline mucus that neutralizes acidic chyme • Muscularis: Smooth muscles Inner: circular, Outer: Longitudinal Except for the major portion of duodenum, the serosa (Visceral peritoneum ) completely surrounds the SI 05/15/19 108
- 109. Structural features include circular folds, Villi and microvilli Circular Folds: Folds of mucosa and sub mucosa. These enhance absorption by increasing the surface area and causing the chyme for spiral rather than move in straight line as it passes through the SI. Villi: Villi are finger like projections of mucosa. Larger number of villi vastly increases the surface area of the epithelium available for absorption and digestion. Each villus is covered by epithelium and has a core of lamina propia embedded in connective tissue of lamina 05/15/19 109
- 110. • Embedded in tissue of lamina propia are an arterioles and venules and blood capillaries. • Nutrients absorbed by the epithelial cells covering the villus pass through the walls of the capillaries to enter blood or lymph. • Besides circular folds and villi, S I also have microvilli, which are the projections of the apical membrane of the absorptive cells when viewed from the microscope. Microvilli are too small to be seen individually instead they form fuzzy line called brush border extending into the lumen of SI 05/15/19 110
- 111. • Brush border structure has several digestive functions Intestinal juice and Brush Border enzyme: 1 -2 lits intestinal juice provide the medium that aids in absorption of substance from the chyme Several absorptive cells of intestine synthesize digestive enzymes , dextrinase, Maltase, Sucrase, Lactase. 2 types of nucleotide digesting enzymes, nucleosidases and phosphatases 05/15/19 111
- 112. • Mechanical Digestion in SI: 2 types of movement of SI 1.Segmentation 2.Migrating motility Complexes (MMC) 05/15/19 112
- 113. Segmentation: Localized mixing contractions that occurs in portions of intestine distended by large volume of chyme. Segmentation mixes chyme with the digestive juices and brings the particles of food into contact with the mucosa for absorption. 05/15/19 113
- 114. 05/15/19 114 Contraction of circular muscle fibres in small portion of SI Muscle fibre encircles the middle of each segment contracts Finally Muscle fibre that contracts first . Relaxes Each small segment unites with the adjoining small segments Large segment is formed again Sequence repeats, chyme slowly sloshes back and forth
- 115. After most of the meal has been absorbed which lessens the distension of the wall of SI, segmentation stops and peristalsis begins Type of peristalsis occurring in SI is MMC Begins in the lower part of the stomach and pushes chyme forward along a short starch of intestine. MMC slowly migrates down the SI reaching the end of the ileum in 90 – 120 mins Chyme remains in SI for 3 – 5 hrs 05/15/19 115
- 116. Chemical Digestion in SI: Chyme entering the SI contains partially digested carbohydrates, proteins and lipids. Completion of the digestion of carbohydrates, proteins and lipids is a collective effort of pancreatic juice, bile and intestinal juice in SI Digestion of Carbohydrates: Few starches are broken down by the time chyme leaves the stomach. Those which are not broken are cleaved by pancreatic amylase. 05/15/19 116
- 117. • It acts on both glycogen and starch, has no effects on polysaccharide called cellulose, an indigestible plant fibre commonly referred as roughage. It moves through the digestive system unaffected. • Pancreatic amylase converts all the digestible polysaccharide (starches) not acted by salivary amylase to disaccharides. • Starch smaller fragments Dextrin Brush border enzymes digest disaccharides to monosaccharides05/15/19 Amylase Dextrinase Removes 1 glucose at a time
- 118. • Digestion of Protein: Protein digestion starts in stomach, where it is fragmented by the action of pepsin. Pancreatic juices contains enzymes, Trypsin, chymotrypsin, carboxypeptidase, Elastase continues to breakdown proteins into peptides (tripeptides, dipeptides and amino acids) Trypsin, Elastase, chymotrypsin cleave peptide bond between amino acid and its neighbour Carboxypeptidase splits off amino acids at caroxyl end of a peptide05/15/19 118
- 119. • It is important that they are produced in inactive form and are activated only upon arrival in the duodenum, otherwise they would digest pancreas. • Digestion of Lipids: Enzymes that split triglycerides and phospholipids are called lipases. Some lipid digestion occur in stomach, most occur in SI through activation of pancreatic lipase. Large lipid globules undergoes emulsification before it is digested in SI. Emulsification causes large lipid molecule to be broken down into 05/15/19 119
- 120. Several small globules formed provide large surface area that allows pancreatic lipases to function more effectively. Digestion of nucleic acids: Pancreatic juice contains 2 nucleases Ribonuclease : Digests RNA Deoxyribonucleases: Digests DNA Nucleotides that result from the activation of 2 nucleases are further digested by brush border enzymes called phosphatases and nucleosidases into pentoses, phosphates and nitrogenous bases.05/15/19 120
- 121. • Sucrose Sucrase Glucose+ Fructose • Lactose Lactase Glucose+ Galactose • Maltose Maltase Glucose+ Glucose • Maltotriose Maltase 3 Glucose 05/15/19 121
- 122. Absorption in SI: Passage of digested nutrients from the GI tract into blood or lymph is called absorption. All chemical and mechanical phase of digestion from mouth through the small intestine are directed towards changing food into the form that can pass through the absorptive epithelial cells lining the mucosa and into the underlying blood and lymphatic vessels. 05/15/19 122
- 123. Absorption: All carbohydrates are absorbed as monosaccharides Starch Maltose, Maltotriose, Dextrin cleaved by dextrinase. After amylase action, brush border enzymes called dextrinase acts on dextrins, clipping off one glucose unit at a time. Ingested molecules of Sucrose, lactose, maltose are acted when they reach SI. 3 brush border enzymes digest disaccharides to monosaccharides. 05/15/19 123
- 124. • Monosaccharides pass from the lumen through the apical membrane via active transport • Glucose and Galactose transported into the absorptive cells of villi via secondary active transport that is coupled to the active transport of Na+. • Transporter has binding site for one glucose and 2 Na+ ions. Unless all 3 sites are filled, neither substance is transported. • Galactose competes with glucose to ride the same transporter. As both Na+ and glucose move in the same direction it is symporter. 05/15/19 124
- 125. Fructose is transported via facilitated diffusion. Monosaccharides move out of the cells through their basolateral surface via facilitated diffusion (spontaneous passive transport)and enter the capillaries of the villi. Absorption of amino acids, Dipeptides and Tripeptides: Most proteins are absorbed as amino acids via active transport occurs mainly in duodenum and jejunum Half of amino acids are present in food, the other half comes from body itself as proteins in 05/15/19 125
- 126. Normally 95-98% of protein is digested and absorbed in SI. Some amino acids enter absorptive cells of villi via Na+ dependant secondary active transport, other amino acid actively transport by themselves. One symporter brings in Dipeptides and Tripeptides together with H+, peptides are then hydrolyzed into single amino acids inside the absorptive cells. Amino acids move out of absorptive cells via diffusion and enter capillaries of villi. 05/15/19 126
- 127. • Absorption of Lipids: Dietary lipids are absorbed via simple diffusion. Short chain fatty acids are hydrophobic but small in size and therefore can dissolve in watery intestinal chyme, pass through the absorptive cells via simple diffusion and follow same route as monosaccharides and amino acids into blood capillary of a villus 05/15/19 127
- 128. • Long chain fatty acids and monoglycerides are large hydrophobic and have difficulty in being suspended in watery enviornment of intestinal chyme. • Bile salts in the intestinal chyme surround long chain fatty acids and monoglycerides forming tiny spheres called miscelles • Miscelles move from the interior of SI lumen to the brush border of absorptive cells. At that point, long chain fatty acid and monoglycerides diffuse into the absorptive cells, leaving the miscelles behind in the chyme 05/15/19 128
- 129. • Miscelles also solubilises other hydrophobic molecules such as fat soluble Vit A,D, E and K , cholesterol and aids in their absorption . • Once inside absorptive cells, long chain fatty acids and monoglycerides are recombined to form triglyceride which aggregate into globules along with phospholipids and cholesterol and become coated with proteins. These spherical masses are called chylomicrons. They leave absorptive cells via exocytosis 05/15/19 129
- 130. • Chylomicrons are large, bulky and cannot enter blood capillary wall instead they enter lacteals which have larger pore size than blood capillaries. • From lacteals, chylomicrons are transported by the way of lymphatic vessels to thoracic duct and enter the blood at left subclavian vein. • After absorption , half of the chylomicrons are removed from the blood. As they pass through blood capillaries in liver and adipose tissue 05/15/19 130
- 131. • NOTE:- • Micelle is an aggregate of many molecules, from these micelles fatty acids, glycerides, sterols etc. are absorbed into the intestinal cells. ... The products of fat digestion are used for synthesizing new fats which are released by the intestinal cells into the lymph, in the form of droplets called chylomicrons. Micelles in the body allows for the absorption of molecules that are insoluble in water such as lipids. They also carry lipid soluble vitamins to the small intestine. • Chylomicrons are formed in the endoplasmic reticulum in the absorptive cells (enterocytes) of the small intestine. The villi, lined with the microvilli of the brush border, provide a lot of surface area for absorption. ... From there the chylomicrons supply the tissue with fat absorbed from the diet. 05/15/19 131
- 132. Enzymes lipoprotein lipase breakdown TG in chylomicrons and other lipoprotein into fatty acid and glycerol Fatty acid diffuses hepatocytes and adipose cells and combine with glycerol during resynthesis TGs After emulsification and absorption of lipids, 90- 95% of bile salts are reabsorbed by SI and returned by blood to the liver through hepatic portal system. This cycle of bile salts secretion by the hepatocytes into bile and reabsorption and resecretion into bile is enterohepatic circulation 05/15/19 132
- 133. Absorption of Electrolytes: Na+ ions actively transport out of absorptive cells via Na+ /K+ ATPase pumps Negatively charged ions like bicarbonate , chloride, iodide passively follow Na+ ions. Others like iron, K, Mg and phosphate are transported via active transport mechanism. Absorption of Vitamins: Fat soluble Vit A, D, E, K are absorbed via simple diffusion. Water soluble vitamins also by simple diffusion Vit B12 Plus intrinsic factor absorbed in ileum by active transport. 133
- 134. • Absorption of Water: SI absorbs about 8.3 lts of fluid out of 9.3. lts 0.9L is absorbed in LI and 0.1l lost in feces. Water absorption occurs via osmosis. Absorbed electrolytes, monosaccharides, amino acid establish conc. gradient that promotes water absorption via osmosis. 05/15/19 134
- 135. 05/15/19 135
- 136. Large Intestine • Terminal portion of GI tract • About 5 feet long and 6.5 cm in diameter, extends from ileum to anus • Rectum (short term storage which holds feces before it is expelled). • Overall function of large intestine are completion of absorption, produce certain vitamins, formation of feces and expulsion of feces from the body. 132
- 137. Large Intestine • Functions – Bacterial digestion • Ferment carbohydrates • Protein breakdown – Absorbs more water – Secretion of Vitamin K & Folic acid
- 138. Four main regions of large intestine are: Cecum, colon, Rectum and Anal Canal Opening from ileum into LI is guarded by fold of mucous membrane called ileocecal sphincter, allows material from SI to pass into LI. Hanging inferior to the ileocecal valve is cecum, a small pouch. Attached to cecum is twisted coiled tube called appendix. This open end of cecum merges with a long tube called colon which is divided into ascending, transverse, descending , sigmoidal portion. 05/15/19 138
- 139. • Rectum ,the last 20 cm of GI tract, lies anterior to the sacrum. • The terminal end of the rectum is called the anal canal • Mucous membrane of the anal canal is arranged in longitudinal folds which have network of arteries and vein . • Opening of anal canal is arranged in longitudinal folds which have network of arteries and veins • Opening of anal canal to exterior is anus guarded by internal anal sphincter (involuntary) and external anal sphincter (voluntary)05/15/19 139
- 140. Histology of LI: LI walls has 4 layers Mucosa: Simple columnar, Lamina Propia: Aerolar connective tissue, Muscularis mucosae: Smooth muscle. Epithelium contains mostly absorptive cells (water absorption) and goblet cells (Mucus secretion) Compared to SI, mucosa of LI does not have many structural adaptations. No circular folds or villi, however microvilli are present on the absorptive cells 05/15/19 140
- 141. Muscularis consists of external layer of longitudinal smooth muscle and internal layer of circular smooth muscle. Unlike other parts of GI, portions of longitudinal muscles are thickened forming three bands called tenae coli. Puckered (wrinkle)appearance of LI is because of haustra.(Series of pouches) Serosa is a part of visceral peritoneum filled with fat are attached to tenae coli called fatty appendages 05/15/19 141
- 142. Function of LI, Rectum and Anal Canal: Absorption: Contents of ileum which passes through ileocaecal valve into the caecum are fluid, even though some water has been absorbed in SI (osmosis) Absorption continues in LI until semisolid consistency of faeces is obtained. Minerals, vitamin and some drugs are also absorbed 05/15/19 142
- 143. • Microbial activity: LI is heavily colonised by certain type of bacteria which synthesize Vit K and folic acid. They include E coli, enterobacter aerogans, Streptococcus faecalis, Clostridium perfringens They may become pathogenic if transferred to another part of body. Gases in the bowel consists of some constituents of air, nitrogen, hydrogen, CO2 and methane produced by bacterial fermentation of unabsorbed nutrients especially carbohydrates. Large number of microbes are present in faeces.05/15/19 143
- 144. Chemical Digestion in LI Chyme carbohydrates 05/15/19 144 Bacterial fermentation Hydrogen, Co2 and Methane gas (flatulence) Remaining Proteins Hydrogen sulphide (odour to faeces) Amino acid Indole, Bilirubin Hydrogen sulphide Bacteria decomposes Stercobilin brown colour to faeces Simpler bilirubin
- 145. Mass Movement: LI does not exhibit peristaltic movement as it is seen in other parts of the digestive tracts. At a fairly long interval a wave of strong peristalsis sweep along the transverse colon forcing its content into descending and sigmoidal colon. This is mass movement. Characteristic movement of LI is haustral churning Haustra is relaxed distended when it is filled After certain point walls contract and squeeze the content to next haustrum.05/15/19 145
- 146. • Defecation: Usually rectum is empty, mass movement forces the content of sigmoid colon into rectum, nerve endings in the walls are stimulated (stretch receptors initiates defecation reflex) • Infant defecation occurs by reflex action. Sometimes in the 2nd or 3rd year of life, the ability to override(disallow) the defecation reflex is developed i.e., brain can inhibit reflex until such time it is convenient to defecate • Receptor sensory NI sacral spinal cord Motor NI colon, rectum, anus 05/15/19 146
- 147. Defecation involves involuntary contraction of muscle of rectum and relaxation of internal anal sphincter. Contraction of abdominal muscle and lowering of diaphragm increases intraabdominal pressure and assists the process of defecation . External anal sphincter is voluntarily controlled . Whenever relaxed, defecation occurs 05/15/19 147
- 148. Phases of Digestion***: Digestive activities occur in three overlapping phases: 1.Cephalic Phase 2.Gastric Phase 3.Intestinal phase 05/15/19 148
- 149. Cephalic Phase: • Smell, sight, thought or initial taste of food activates neural centers in the cerebral cortex, hypothalamus and brain stem. • Brain stem activates facial(VII), glossopharangeal (IX) and vagus nerves. • Facial and glossopharangeal stimulates salivary gland to secerte saliva and vagus stimulates gastric glands to secerte gastric juices 05/15/19 149
- 150. Gastric Phase: • Food reaches stomach, gastric phase begins. • Neural and hormonal mechanisms regulate the gastric phase of digestion to promote gastric secretion and gastric motility. Neural regulation: Food distends the stomach which stimulates stretch receptors in its walls pH of the stomach Chyme is monitored by chemoreceptors Distended stomach and increased pH (proteins entered the stomach and buffered some stomach150
- 151. • Strch receptors and chemoreceptors are activated and a neural negative feedback is set. • From stretch and chemoreceptors nerve impulses propagate to submucosal plexus which stimulates parasympathetic and enteric neurons causes waves of peristalsis and stimulates flow of gastric juice from the gastric gland. • Peristalsis wave mixes the food with gastric juice. • Strong waves undergoes gastric emptying into duodenum • pH of stomach Chyme and distension of stomach wall lessens (Chyme passes into SI, suppressing the secretion of gastric juices 05/15/19 151
- 152. Hormonal Regulation: • Gastric secretion during gastric phase is regulated by hormone gastrin. • G cells of gastric gland release gastrin Stimuli for gastrin release: 1.Distension of stomach by chyme 2.Partially digested proteins in the chyme High pH of the chyme (Presence of food, caffeine and Ach released by parasympathetic neurons) 05/15/19 152
- 153. Gastrin stimulates 1. gastric gland to secrete large amounts of gastric juices 2. Strengthens the contraction of lower esophageal sphincter (Prevents reflux) 3. Increases motility of stomach 4. Relaxes pyloric sphincter (Gastric emptying) Gastrin is inhibited when the pH of gastric juice drops below 2.0 and stimulated when pH rises 05/15/19 153
- 154. Intestinal Phase: Begins when food enters into SI Reflexes initiated during cephalic and gastric phase, increases stomach secretion activity and motility Intestinal phase shows inhibitory effects i.e. slows the exit of chyme from stomach (Prevents duodenum from being overloaded) 05/15/19 154
- 155. • Neural Regulation: Distension of duodenum causes enterogastric reflex. Stretch receptors in the duodenal wall send nerve impulse to medulla oblongata to inhibit parasympathetic stimulation and stimulates the sympathetic nerves of the stomach. Results in decreased gastric motility, increased contraction of pyloric sphincter, decreased gastric emptying 05/15/19 155
- 156. Hormonal Regulation: Intestinal phase of digestion is mediated by two major hormones secreted by SI: CCK & Secretin 1. CCK stimulates secretion of pancreatic juice rich in digestive enzymes 2. Contraction of wall of gall bladder (bile out of gall bladder into cystic duct) 3. Relaxation of sphincter of hepatopancreatic ampulla which allows pancreatic juice and bile to flow into duodenum 4. Slows gastric emptying by promoting contraction of pyloric spincter 5. Enhances the effect of secretin 05/15/19 156
- 157. Acidic chyme entering duodenum stimulates the release of Secretin from S cells: 1.Secretin stimulates the flow of pancreatic juice rich in bicarbonate ions to buffer the acidic chyme that enters the duodenum from stomach 2.Inhibits secretion of gastric juice, promotes normal growth and maintenance of the pancreas and enhances the effect of CCK 3.Secretin causes buffering of acid in chyme that reaches duodenum and slows production of acid in stomach 05/15/19 157
Editor's Notes
- Absorption of Alcohol: The intoxicating and incaapacitating effect of alcohol depends on blood alcohol level. Alcohol absorption begins in stomach. However the surface area in SI is greater than stomach, so when alcohol passes duodenum it is absorbed rapidly. The longer alcohol is in stomach blood alcohol level rises slowly. Enzyme Alcohol dehydrogenase present in gastric mucosa, breaks down alcohol to acetaldehyde. Alcohol dehydrogenase activity is lower females than males. Also Asian males have lower level of this enzyme
- Depending on the maturity of the group, you can talk about the feces leaving via the anus. Mention the appendix at the bottom of the ascending colon and that it might have been used long ago but is not today Mention the portions of the large intestine, ascending, transverse, descending, sigmoid, and rectum (last one if the audience is mature enough)
