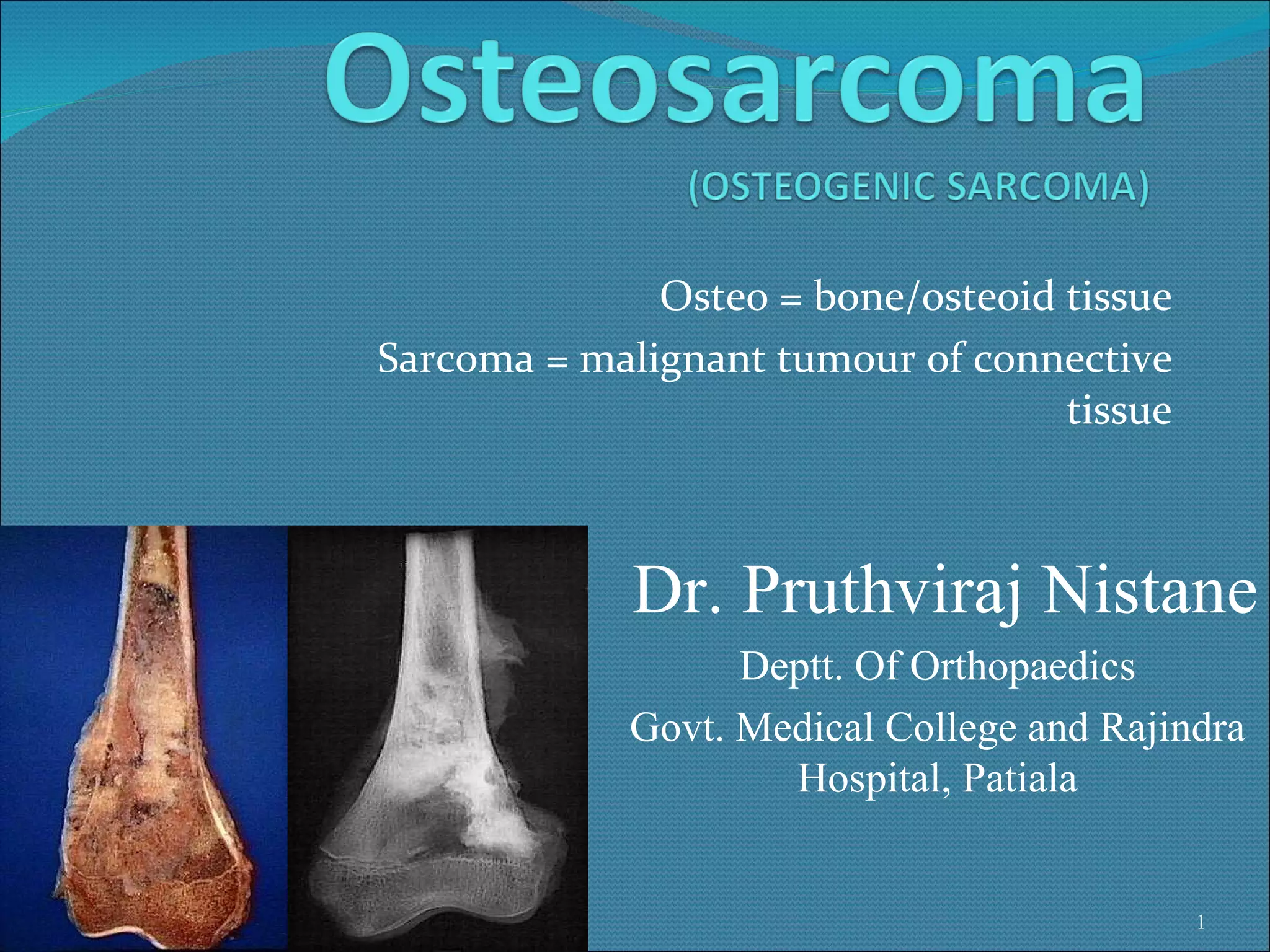
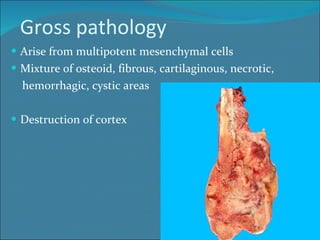
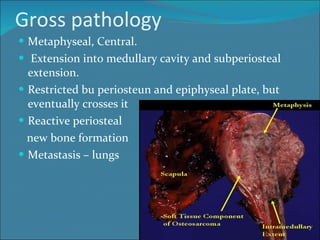
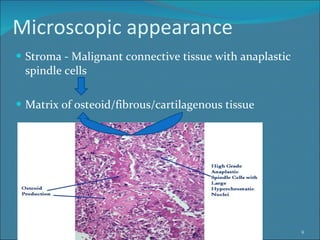
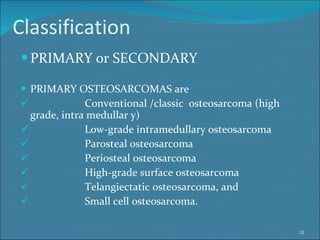
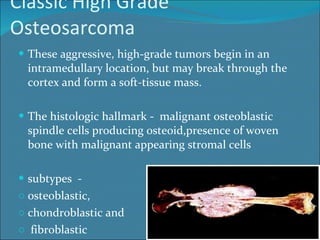
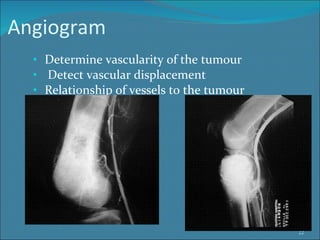
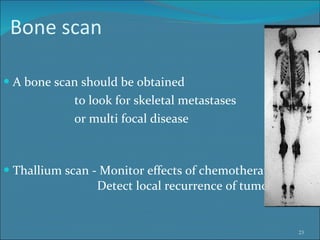
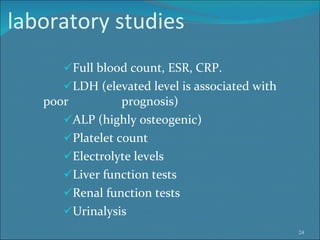
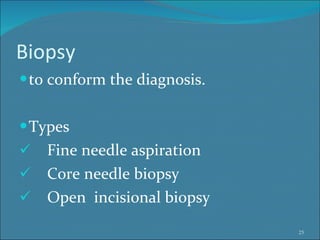
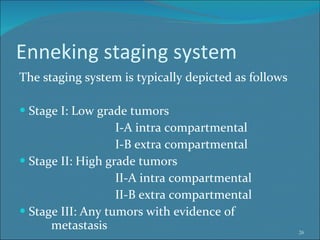
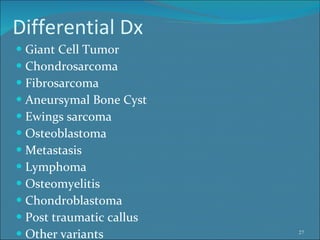
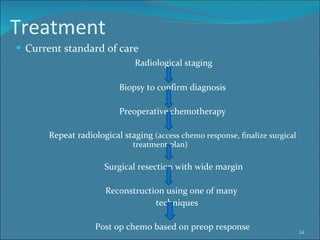
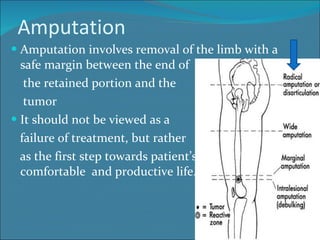
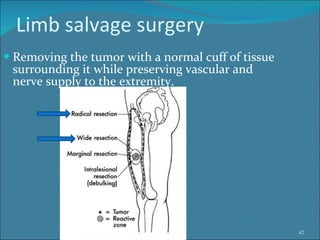
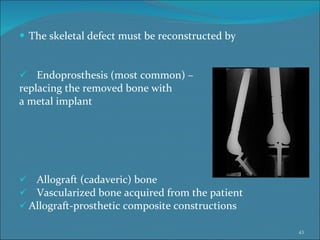
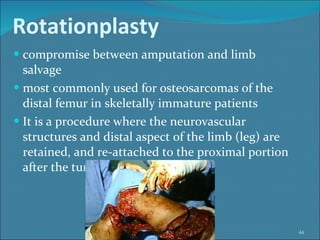
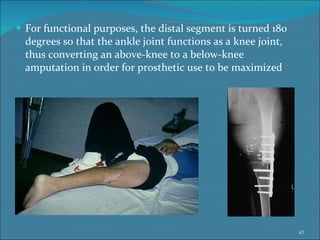
Osteosarcoma is a highly malignant bone tumor primarily affecting adolescents, characterized by spindle-shaped cells that produce osteoid. The diagnosis involves various imaging techniques and biopsies, with treatments including chemotherapy and surgical resection, often necessitating limb-sparing procedures over amputation. Prognosis is influenced by tumor grade, size, location, and presence of metastasis, with significant relapses occurring in high-grade cases.