Pharmacology
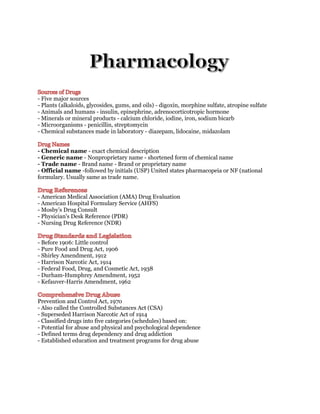
- 1. - Five major sources - Plants (alkaloids, glycosides, gums, and oils) - digoxin, morphine sulfate, atropine sulfate - Animals and humans - insulin, epinephrine, adrenocorticotropic hormone - Minerals or mineral products - calcium chloride, iodine, iron, sodium bicarb - Microorganisms - penicillin, streptomycin - Chemical substances made in laboratory - diazepam, lidocaine, midazolam - Chemical name - exact chemical description - Generic name - Nonproprietary name - shortened form of chemical name - Trade name - Brand name - Brand or proprietary name - Official name -followed by initials (USP) United states pharmacopeia or NF (national formulary. Usually same as trade name. - American Medical Association (AMA) Drug Evaluation - American Hospital Formulary Service (AHFS) - Mosby’s Drug Consult - Physician's Desk Reference (PDR) - Nursing Drug Reference (NDR) - Before 1906: Little control - Pure Food and Drug Act, 1906 - Shirley Amendment, 1912 - Harrison Narcotic Act, 1914 - Federal Food, Drug, and Cosmetic Act, 1938 - Durham-Humphrey Amendment, 1952 - Kefauver-Harris Amendment, 1962 Prevention and Control Act, 1970 - Also called the Controlled Substances Act (CSA) - Superseded Harrison Narcotic Act of 1914 - Classified drugs into five categories (schedules) based on: - Potential for abuse and physical and psychological dependence - Defined terms drug dependency and drug addiction - Established education and treatment programs for drug abuse
- 2. - Schedule I - Heroin - High abuse potential - No accepted medical use - Schedule II - Opium, morphine - High abuse potential - Accepted medical uses - Schedule III - Codeine, hydrocodone - Less abuse potential than drugs in schedules I and II - Accepted medical uses; may lead to some physical dependence or high psychological dependence - Schedule IV - Barbital, diazepam - Lower abuse potential than schedule III drugs - Accepted medical uses; may lead to limited physical or psychological dependence - Schedule V - Some OTC meds - Low abuse potential compared to schedule IV drugs - Accepted medical uses; may lead to limited physical or psychological dependence - In 1973 the Drug Enforcement Agency (DEA) became the sole drug enforcement organization in the U.S. - Food and Drug Administration - Public Health Service - Federal Trade Commission - Canadian drug control - International drug control - Therapeutic effects - Desirable drug actions - Side effects - Undesirable or harmful drug actions - Drug interaction with other drugs- Can produce unpredictable effects - Drug actions are biochemical interaction between drug and tissue components ➔ A drug that interacts with a receptor to stimulate a response is known as an agonist. ➔ A drug that attaches to the receptor but does not stimulate a response is called antagonist.
- 3. Pharmaceutical Phase - Pharmaceutics - Science of dispensing drugs - Dissolution - Rate at which a solid drug goes into solution after ingestion. More rapid rate of dissolution = more quickly drug is absorbed Pharmacokinetic Phase - Pharmacokinetics - How the body handles a drug over a period of time • Absorption • Distribution • Biotransformation • Excretion Drug Absorption - Movement of drug molecules from site of entry to general circulation - Variables affecting drug absorption ▪ Nature of the absorbing surface ▪ Blood flow to the site of admin ▪ Solubility of the drug ▪ PH of the drug environment ▪ the Drug concentration ▪ The form of the drug dosage o Absorbing surface o Blood flow to the administration site o Drug solubility o pH o Drug concentration o Dosage form ➔ All drugs must be in solution to cross the cell membranes to achieve absorption. The term dissolution refers to the rate at which a solid drug goes into a solution after ingestion. The faster the rate of dissolution, the faster the absorption.
- 4. - Mode affects the rate of onset of action - May affect the therapeutic response - Drugs are given for local or systemic effects - Topical - Enteral - Pulmonary - Parenteral Enteral Route - Drugs administered along GI tract - Oral - Rectal - Nasogastric - Safe, convenient, economical - Least reliable and slowest route - Food contents - Emotional state - Physical activity Oral Absorption - Rich blood supply, little absorption in mouth - Nitroglycerin and some hormones administered by sublingual or buccal routes - Rapidly dissolve in salivary secretions Gastric Absorption - Length of time a drug remains in the stomach varies depending on: - pH of the environment - Gastric motility - stomach movement Absorption in the Small Intestine - Rich blood supply and large absorption area - Most drug absorption occurs in the upper portion of the small intestine Rectal Absorption - Effective for some medications - Vascular surface area capable of drug absorption - Erratic absorption may occur from: - Rectal contents - Local drug irritation - Uncertainty of drug retention - No hepatic alteration on first pass through body
- 5. - Subcutaneous - Intramuscular - Intravenous - Intradermal - Intraosseous - Endotracheal Subcutaneous Administration - An injection beneath skin into connective tissue or fat beneath dermis - Used for small volumes of drugs (<0.5 mL) that do not irritate tissue - Absorption rate is slow - Can provide sustained effect Intramuscular Administration- Injection given into skeletal muscle - Absorption occurs more rapidly than SC injection - Greater tissue blood flow Intravenous Administration - An injection given directly into the bloodstream - Bypasses absorption process - Almost immediate effect - Most IV drugs are administered slowly to help prevent adverse reactions Intradermal Administration - TB Skin test - Injection just below the epidermis - Primarily used for allergy testing and to administer local anesthetics Intraosseous Administration - An injection directly into the bone marrow cavity through an IO infusion system - Agents circulate via bone’s medullary cavity - Time from injection to onset of action similar to venous route Endotracheal Administration - Generally through an ET tube - Drug delivery into the pulmonary alveoli - Systemic absorption via lung capillaries - Absorption almost as rapid as IV route - Usually reserved for situations in which an IV line cannot be established - Adult ET medications include: - Lidocaine (Xylocaine) - Epinephrine (Adrenalin) - Atropine - anticholinergic - Naloxone (Narcan) Pulmonary Route - Drugs given by gas or fine mist (aerosol) - Absorption in blood is rapid due to: - Large surface area - Rich alveolar capillary network - Produces primarily local effects
- 6. - Occasionally unwanted systemic effects Topical Route - Patches - Drugs applied topically to skin and mucous membranes - Usually rapidly absorbed to produce a local effect - Only intact skin surfaces used to prevent systemic effects - Massaging skin promotes drug absorption Drug Distribution - Transport of a drug through the bloodstream to body tissues and site of action - Distribution rate depends on capillary permeability to drug - Cardiac output and regional blood flow affectrate and extent of distribution Drug Reservoir - Drugs accumulate at storage sites, form reservoirs by binding to specific tissues - Two types of drug reservoirs: - Plasma protein binding - Tissue binding Blood-Brain Barrier - Single layer of capillary endothelial cells - Line blood vessels entering the CNS - Permits only lipid-soluble drugs to be distributed into brain and CSF • e.g., general anesthetics and barbiturates - Drugs poorly soluble in fat have trouble passing this barrier - Cannot enter the brain • e.g., many antibiotics Placental Barrier - Membrane layers separate blood vessels of mother and fetus - Not permeable to many lipid-insoluble drugs - Provides some protection to the fetus - Allows passage of certain non-lipid-soluble drugs • Steroids, narcotics, anesthetics, and some antibiotics - Can affect developing embryo or neonate if give to pregnant mother Biotransformation - Process by which the drug is chemically converted to a metabolite (usable form) - Purpose is to "detoxify" a drug and render it less active - Liver is primary site of drug metabolism - If drug metabolism is delayed, drug accumulation and cumulative drug effects may occur Excretion - Elimination of toxic or inactive metabolites - Organs of excretion - Kidneys - Intestine - Lungs - Sweat and salivary glands - Mammary glands Excretion by Kidneys - Can be excreted in urine unchanged or as metabolite of its previous form - Renal excretion - Passive glomerular filtration - no energy involved - Partial reabsorption - Active tubular secretion - particles are being pushed - energy is expended
- 7. Hemodialysis - artificial kidney - filters blood - Substances completely or almost completely excreted by the normal kidney can be removed by this artificial process - Not effective for highly tissue- or protein bound drugs - Limited benefit with rapidly acting toxins Excretion by the Intestine - Drugs eliminated by biliary excretion - After liver metabolism, metabolites are carried in bile, passed into duodenum, and eliminated with feces - Some drugs are reabsorbed by the bloodstream, returned to the liver, and later excreted by the kidneys Excretion by the Lungs - Drugs that can be excreted by the lungs include: - General anesthetics - Volatile alcohols - Inhaled bronchodilators - Factors that can alter elimination via the lungs are: - Rate and depth of respiration - Cardiac output Secretion through Sweat and Salivary Glands - Sweat is unimportant means of drug excretion - Drugs excreted in saliva are usually swallowed and eliminated in the same manner as other orally administered drugs Excretion through Mammary Glands - Many drugs or their metabolites cross the epithelium of the mammary glands - Are excreted in breast milk - Breast milk is acidic (pH 6.5) - Nursing mothers are cautioned against medication use
- 8. - Age - Body mass - Gender - Environment - Time of administration - Pathological state - Genetic factors - Psychological factors Pharmacodynamics - Study of how a drug acts on a living organism - Pharmacologic response relative to the concentration of a drug at an active site in the organism Most drugs produce effects by: - Drug-receptor interaction • Agonists - helps a certain body function • Antagonists - blocks a certain body function • Affinity - between receptor site and drug • Efficacy - how well and how fast it works • Types of receptors - Drug-enzyme interaction - Nonspecific drug interaction Drug-Receptor Interaction Agonists - Drugs that bind to a receptor and cause a physiological response Antagonists- Drugs that bind to a receptor and whose presence prevents a physiological response or other drugs from binding Drug Response Assessment - Assess by observing the physiological parameters - e.g., BP, pain - Effects of some drugs cannot be monitored solely by the patient's response Plasma Level Profiles - Relationship between plasma concentration and level of therapeutic effectiveness over time - Depend on: • Rate of absorption • Distribution • Biotransformation • Excretion
- 9. Plasma Level Profiles - Therapeutic range - Concentration (dose) that provides highest probability of response - Least risk of toxicity - Some patients fail to respond to therapeutic doses - Others may develop toxicity Biological Half-Life - Time needed to metabolize or eliminate half of total amount of drug in body - A drug is considered gone from the body after five half-lives have passed - Affected by renal and hepatic function - 3-5 min half life Adenosine - 10-15 second half life Therapeutic Index - Measures relative safety of a drug - Ratio between: - Lethal dose 50 (LD 50) • Dose of a drug lethal in 50% of laboratory animals tested - Effectiveness dose (ED 50) • Dose that produces a therapeutic effect in 50% of a similar population - TI = LD 50/ED 50 - The closer the ratio to 1, the greater the danger in administering the drug to humans Drug-Receptor Interaction - Most drug actions - Chemical interaction between drug and various receptors in body - Most common form of drug action is the drug receptor interaction - Most drugs are thought to bind to drug receptors to produce their desired effect Drug Interactions - Variables influencing drug interaction: - Intestinal absorption - Competition for plasma protein binding - Drug metabolism or biotransformation - Action at the receptor site - Renal excretion - Alteration of electrolyte balance Drug-Drug Interactions - Some drug-drug interactions are dangerous - Drugs associated with significant interactions: - Blood thinners (anticoagulants) - Tricyclic antidepressants - Monoamine oxidase (MAO) inhibitors - Amphetamines - Digitalis glycosides (digoxin, lanoxin) - Diuretics - Antihypertensives
- 10. Drug Interactions - Other factors influencing drug interactions: - Drug-induced malabsorption of foods and nutrients - Food-induced malabsorption of drugs - Enzyme alterations that affect the metabolism of foods or drugs - Alcohol consumption - Cigarette smoking (birth control + smoking = pulmonary embolism) - Food-initiated alteration of drug excretion Drug Storage - Refer to local protocol - Drug potency can be affected by: - Temperature - Light - Moisture - Shelf life - Controlled medications security - behind 2 locks Components of a Drug Profile - Drug names (generic name and trade name) - Classification (mechanism of action) - Indications (When do you give it ) - Pharmacokinetics ( how it works in the body) - Side/adverse effects - Dosages - Routes of administration - Contraindications (when do you not give it.) - Special considerations (pregnant, pediatric, geriatrics) - Storage requirements Pregnancy Ratings for Drugs - Category A - Risk of fetal harm remote - Category B - Inconclusive risk in first trimester, no risk in later trimesters - Category C - Give only if potential benefit outweighs risk to fetus (MOST NARCOTICS) - Category D - Evidence of fetal risk; may be acceptable if life-threatening situation - Category X - Risk outweighs any benefit Pediatrics - Effects unpredictable in infants - Drug doses weight related - Higher doses of water-soluble drugs may be needed - Less effective blood-brain barrier in infants - Slow drug clearance, excretion - Longer half-life
- 11. Elderly / Geriatric - Causes of noncompliance and medication errors: - Expense - Forgetfulness or confusion - Symptoms disappear - Errors in taking medications - Noncompliance may be deliberate Drugs that Affect the Nervous System Autonomic Nervous System - Effects of many drugs depend on: - Which branch of ANS they act on - Whether the ANS branch is stimulated or inhibited by drug therapy - Norepinephrine runs the sympathetic nervous system - Acetylcholine runs the parasympathetic nervous system - CNS - Brain - Spinal cord - PNS - Cranial and spinal nerves and their branches - Connects all parts of body to CNS Acetylcholine (ACh - At junction between preganglionic fiber and synapse - At junction between postganglionic fiber and effector cell - Fibers that release ACh are known as cholinergic fibers • All preganglionic fibers of autonomic division • All postganglionic fibers of parasympathetic division Norepinephrine - Neurotransmitter between sympathetic postganglionic fiber and effector cell - Adrenergic fibers - Release norepinephrine - Most postganglionic neurons of the sympathetic division are adrenergic
- 12. Nerve Impulse Transmission Acetylcholine - combines with cholinergic receptors - Nicotinic • Excitatory response - Muscarinic • Excites or inhibits Norepinephrine - combines with alpha and beta receptors in effector organs - Binds to and activates both types of receptor molecules • More affinity for alpha receptors Epinephrine - is an adrenergic substance: - Produced by adrenal medulla - Nearly equal affinity for both receptors, alpha and beta - In tissues containing alpha- and beta-receptor cells, one type is more abundant - Has a dominating effect Classifications - Cholinergic (parasympathomimetic) (mimetic = copy/mimic) - Cholinergic blocking (parasympatholytic) (lytic = block/stops) - Adrenergic (sympathomimetic) - Adrenergic blocking (sympatholytic)
- 13. Narcotic Analgesics and Antagonists - Narcotic analgesics relieve pain - Narcotic antagonists reverse the narcotic effects of some narcotic analgesics Pain Components - Sensation of pain • Involves the nerve pathways and the brain - Emotional response to pain • Anxiety level • Previous pain experience • Age • Gender • Culture Narcotics - Contain or abstracted from opium - Morphine: Chief alkaloid of opium - Binds with opioid receptors in brain and other body organs - Alters pain perception and emotional response to pain Undesirable effects - Nausea and vomiting - Constipation - Urinary retention - Cough reflex suppression - Orthostatic hypotension - CNS depression Opioid Analgesics - Morphine (morphine sulfate) - Codeine (methylmorphine) - Hydromorphone (Dilaudid, Dilaudid-HP) - Meperidine (Demerol) - Methadone (Dolophine, Methadose) - Oxycodone (Percodan, Tylox, Percocet) - Hydrocodone (Lortab) - Propoxyphene (Darvon, Dolene)
- 14. Opioid Antagonists - “Block” opioid analgesics - Displace analgesics from receptor sites - Examples: - Naloxone (Narcan) - Naltrexone (Trexan) - Nalmefene (Revex) Opioid Agonist-Antagonists - Analgesic and antagonist effects - Pharmacokinetic and adverse effects similar to morphine - Lower dependency risk than opioids - Less severe withdrawal symptoms - May cause withdrawal symptoms in addicts Nonnarcotic Analgesics - Peripheral mechanism - Interferes with local mediators released when tissue is damaged - Mediators stimulate nerve endings - Cause pain - Nonnarcotic analgesics decrease nerve ending stimulation Anesthetics - CNS depressants - Reversible action on nervous tissue - Major categories of anesthesia: - General - Regional - Local Antianxiety Agents and Alcohol - Antianxiety agents - Reduce feelings of apprehension - Nervousness - Worry - Fearfulness
- 15. Sedative-Hypnotic Agents - Depress CNS - Calming effect - Sedatives and hypnotics differ by degree of CNS depression - Agent may be sedative and hypnotic - Depends on dose used Alcohol - CNS depressant - Can produce sedation, sleep, and anesthesia - Enhances sedative-hypnotic effects of other drugs - Blood alcohol measured (mg/dL) - Behavioral effects based on blood alcohol levels Benzodiazepines - Bind to receptors in cerebral cortex and limbic system - Actions - Anxiety reducing - Sedative-hypnotic - Muscle relaxing - Anticonvulsant - Schedule IV drugs Commonly prescribed benzodiazepines - Alprazolam (Xanax) - Chlordiazepoxide (Librium) - Clorazepate (Tranxene) - Diazepam (Valium) - Flurazepam (Dalmane) - Prazepam (Centrax) - Midazolam (Versed) - Lorazepam (Ativan) - Triazolam (Halcion)
- 16. Barbiturates - Duration of action - Ultra-short acting - Short acting - Intermediate acting - Long acting Sedative-Hypnotic Drugs - Not benzodiazepines or barbiturates - More like barbiturates than benzodiazepines - Examples - Chloral hydrate (Noctec) - Ethchlorvynol (Placidyl) - Meprobamate (Equanil, Meprospan) - Some antihistamines have sedative effects - Hydroxyzine hydrochloride (Vistaril, Atarax) Anticonvulsants - Treat seizure disorders - Mode of action not understood - Choice of drug depends on: - Type of seizure disorder - Patient's drug tolerance - Medication noncompliance common CNS Stimulants - Classified by site of action - Cerebrum - Medulla and brainstem - Hypothalamic limbic regions - Common CNS stimulant drugs - Anorexiants - Amphetamines
- 17. Psychotherapeutic Drugs - Psychotherapeutic drugs include - Antipsychotic agents - Antidepressants - Lithium - Treat psychoses and affective disorders - Schizophrenia, depression, and mania - Neurotransmitters in CNS affecting emotion: - Acetylcholine - Norepinephrine - Dopamine - Serotonin - Monoamine oxidase CNS and Emotions - Alterations in neurotransmitter levels associated with changes in mood and behavior - Drug therapy alleviates symptoms - Temporarily modifies unwanted behavior Antipsychotic Agents - Schizophrenia (primary use) - Tourette syndrome - Senile dementia associated with Alzheimer disease - Antipsychotic (neuroleptic) drugs block CNS dopamine receptors Classifications - Phenothiazine derivatives - Butyrophenone derivatives - Dihydroindolone derivatives - Dibenzoxapine derivatives - Thienbenzodiazepine derivatives - Atypical agents
- 18. Antidepressants - Treatment of affective disorders (mood disturbances) - Depression - Mania - Elation - Tricyclic antidepressants and MAO inhibitors are prescribed for depression - Lithium is preferred treatment for mania - Newer classes of antidepressants (second-generation drugs) have been developed - Examples - Bupropion (Wellbutrin) - Fluoxetine (Prozac) - Trazodone (Desyrel) - Sertraline (Zoloft) - Paroxetine (Paxil) Tricyclic Antidepressants - Increase levels (block reuptake) of norepinephrine and serotonin - Examples - Imipramine (Tofranil) - Amitriptyline (Elavil) MAO Inhibitors - Central-acting monoamines, especially norepinephrine and serotonin are thought to cause depression and mania - Monoamine oxidase is responsible for metabolizing norepinephrine within nerve - MAO inhibitors block this enzyme, leading to increased norepinephrine levels Lithium - Alters sodium transport in nerve and muscle cells - Affects norepinephrine and serotonin - Antimanic effects are thought to result from: - Increased norepinephrine uptake - Increased serotonin receptor sensitivity
- 19. Drugs for Specific CNS-Peripheral Dysfunction - Parkinson disease - Muscle rigidity - Tremors - Suspected cause: Low dopamine levels - Huntington disease - Progressive dementia - Involuntary muscle twitching - Dopamine, acetylcholine imbalance Drugs with Central Anticholinergic Activity - Inhibit or block acetylcholine - Anticholinergic - Restore brain’s dopamine-acetylcholine balance - Examples - Benztropine (tablets and injections) - Ethopropazine hydrochloride Drugs Affecting Brain Dopamine - Three classifications - Those that release dopamine - Those that increase brain levels of dopamine - Dopaminergic agonists Skeletal Muscle Relaxants - Central acting - Baclofen (lioresal) - Cyclobenzaprine (flexeril) - Diazepam (valium) - Direct acting - Dantrolene (Dantrium) - Neuromuscular blockers - Can cause paralysis - Pancuronium (Pavulon), vecuronium (Norcuron) - Succinylcholine (Anectine)
- 20. Drugs Affecting the ANS - Autonomic drugs - Mimic or block effects of sympathetic and parasympathetic divisions of autonomic nervous system Autonomic Drugs - Cholinergic drugs - Parasympathomimetic - Mimic parasympathetic nervous system - Cholinergic-blocking drugs - Parasympatholytic - Block parasympathetic nervous system - Adrenergic drugs - Sympathomimetic - Mimic sympathetic nervous system (adrenal medulla) - Adrenergic-blocking drugs - Sympatholytic - Block actions of sympathetic nervous system (adrenal medulla)
- 21. Alpha activities - Vasoconstriction • Arterioles in the skin and splanchnic area • Pupil dilation - Relaxation of the gut Beta activities - Cardiac acceleration and increased contractility - Vasodilation of skeletal muscle arterioles - Bronchial relaxation - Uterine relaxation Alpha-Blocking Drugs (blocking the vasoconstriction) = promotes arterial vasodilation - Block the vasoconstricting effect of catecholamines - Used in certain cases of hypertension - Prevent necrosis after norepinephrine (Levophed) or dopamine (Intropin) extravasation into tissues - Limited use in prehospital setting Beta-Blocking Agents - blocks b1 (increased automaticity + contractility +HR) = decrease automaticity and contractility - HR - Block beta receptors - Selective beta 1 blockers - Metoprolol, atenolol - Treatment of hypertension, angina Nonselective beta blockers - Nadolol, propranolol, labetalol - Antianginal, antihypertensives
- 22. Cardiac Drug Terminology Chronotropic drugs - Affect heart rate Dromotropic drugs - Affect conduction velocity through the conducting tissues of the heart (AV Node conductivity) Inotropic drugs - Affect force of contraction - Positive inotropic effect (+force of contraction) - Increase contractility - Negative chronotropic effect (-hr) - Slow heart rate - Negative dromotropic effect - Slow conduction velocity Digoxin (Lanoxin) - Small therapeutic index - Side effects common
- 23. Antidysrhythmic Medications Antidysrhythmic Classes Class I Sodium Channel Blockers Class I-A - Decrease conduction velocity - Prolong electrical potential of cardiac tissue - Procainamide (Pronestyl) Class I-B - Decrease or have no effect on conduction velocity - Lidocaine (Xylocaine) Class I-C - Profoundly slow conduction - Control life-threatening ventricular dysrhythmias - Flecainide (Tambocor) Class II - Beta-blocking agents - Reduce adrenergic stimulation of the heart - Negative chronotropic effects - Decreases Blood Pressure & Decreases Heart rate - Propranolol - Metoprolol - Atenolol Class III - Potassium channel blockers - Increases contractility - Does not suppress automaticity - Has no effect on conduction velocity - Terminates dysrhythmias that result from reentry of blocked impulses - Amiodarone (Cordarone)
- 24. Class IV - Calcium channel blockers - Blocks inflow of calcium through cell membranes of cardiac and smooth muscle cells - Depresses the myocardial and smooth muscle contraction - Decreases automaticity and in some cases decreases conduction velocity - Diltiazem (Cardizem) Antihypertensive Medications (includes many classes with multiple mechanism of actions) Sympathetic blocking agents (sympatholytic drugs) - medications that block the sympathetic nervous system Vasodilators - Angiotensin-converting enzyme (ACE) inhibitors - Calcium channel blockers - Angiotensin II receptor antagonists Diuretics - Renal excretion of excess salt and water from the body - Used in the treatment of edema, HTN, Hormonal acne… - Lasix Thiazide diuretics - Moderately effective in lowering blood pressure - Hydrochlorothiazide (HCTZ) Loop diuretics - Short-acting agents that inhibit sodium and chloride reabsorption in loop of Henle - Furosemide (Lasix) Potassium-sparing diuretics - Less potassium loss than other diuretics - Spironolactone (Aldactone)
- 25. Sympathetic Blocking Agents - Beta-blocking agents and adrenergic inhibiting agents Beta-blocking agents - Treatment of suspected myocardial infarction, high-risk unstable angina, and hypertension • Atenolol (Tenormin), metoprolol (Lopressor) • Labetalol (Normodyne, trandate), nadolol (Corgard) Adrenergic Inhibiting Agents - Centrally acting adrenergic inhibitors - Clonidine hydrochloride (Catapres) - Peripheral adrenergic inhibitors - Doxazosin (Cardura) - Mechanism by which many of these agents work is unknown Vasodilator Drugs - Act directly on the smooth muscle walls of arterioles, veins, or both - Lower peripheral resistance and blood pressure - Arteriolar dilator drugs • Hydralazine (Apresoline) - Arteriolar and venous dilator drugs • Nitroglycerin sublingual tablet (Nitrostat) (primarily venous dilator) ~during an MI - decrease ventricular workload, increase collateral circulation Angiotensin-Converting Enzyme (ACE) Inhibitors -taking AT2 out of play, resulting in vasodilation Give Ace inhibitor after MI in order to lower SVR to lower workload of left ventricle. Angiotensin II is a powerful vasoconstrictor: - Raises blood pressure - Causes the release of aldosterone • Contributes to sodium and water retention - Inhibits conversion of angiotensin I to angiotensin II (brought about through ACE) - Renin-angiotensin-aldosterone system is suppressed - Blood pressure is lowered • Captopril (Capoten) • Enalapril, Ramipril, Lysinopril
- 26. Calcium Channel Blockers - inhibits outflux of Mg in Mg-Ca pump, slowing it down - Inhibit contractility of vascular smooth muscle - Reduce peripheral vascular resistance - Dilate coronary vessels - Verapamil (Isoptin) - Diltiazem (Cardizem) Angiotensin II Receptor Antagonists - Selectively inhibit angiotensin II receptors - Lower systolic and diastolic BP - Candesartan (Atacand) - Irbesartan (Avapro) - Losartan (Cozaar, Hyzaar) Monoamine Oxidase (MAO) Inhibitors - Block release of norepinephrine at the sympathetic junction - Interfere with vasoconstriction - Reduce peripheral vascular resistance - Decrease blood pressure - Not widely used to treat hypertension Antihemorrheological Agents - Used to treat peripheral vascular disorders caused by pathological or physiological obstruction Antihemophilic Agents Hemophilia - Hemophilia A (classic hemophilia) is caused by a deficiency of factor VIII - Hemophilia B (the “Christmas disease”) results from a deficiency in factor IX complex - Replacement therapy of the missing clotting factor can be effective in the management of hemophilia • Factor VIII (Factorate) • Factor IX (Konyne) • Anti-inhibitor coagulant complex (Autoplex)
- 27. Drugs that Affect the Blood - Drugs that affect blood coagulation may be classified as: - Antiplatelet agents - Anticoagulant agents - Fibrinolytic agents Antiplatelet Agents - Interfere with platelet aggregation - Prevention of clots, MI, stroke - Treatment of valvular disease, shunts - Include: - Aspirin - prevents thromboxin a2 release - Dipyridamole (Persantin) - Abciximab (ReoPro) What is the Clotting Cascade ➔ Whether intrinsic or extrinsic injury, a chemical called thromboxane A2 stimulates platelet aggregation and localized vasoconstrictor. Produces more prothrombin, which stimulates thrombin release, which produces fibrinogen (a sheet of fibrin) that cleaves into the fiber network. When we're done with the clot, we release plasminogen which changes into plasmin which eats the fiber network. TPA - tissue plasminogen activator. Fibrinolytics (eats fiber)(-ase) Anticoagulants -works on clotting cascade instead of inhibiting thromboxin A2 - Used to prevent intravascular thrombosis - Decreases blood coagulability Examples - Heparin (Liquaemin) - Coumadin (Warfarin) Fibrinolytic Agents - Used to dissolve clots after formation - Used for some acute myocardial infarcts - Used in some stroke patients - Examples - Streptokinase - Tissue plasminogen activator (t-PA) - Reteplase (Retavase) - Alteplase (Activase) - Tenecteplase (TNKase)
- 28. Hemostatic Agents - Hasten clot formation to reduce bleeding - Systemic hemostatic agents • Control rapid blood loss after surgery by inhibiting fibrinolysis - Topical hemostatic agents • Control capillary bleeding during surgical and dental procedures Blood and it’s Components Replacement therapies - Whole blood (rarely used) - Packed red blood cells - Fresh-frozen plasma - Plasma expanders (Dextran) - Platelets - Coagulation factors - Fibrinogen - Albumin - Gamma globulins Antihyperlipidemic Drugs - Hyperlipidemia: Excess lipids in plasma - Used in conjunction with diet and exercise to control serum lipid levels - Examples - Atorvastatin (Lipitor) - Cholestyramine (Questran) - Niacin (Nicobid) - Pravastatin (Pravachol) - Lovastatin (Mevacor) - Simvastatin (Zocor)
- 29. Respiratory Medication’s Bronchodilators - Primary treatment for obstructive pulmonary disease - Asthma, chronic bronchitis, and emphysema - Classified as: - Sympathomimetic drugs - Xanthine derivatives - Many agents are administered by inhalation via a nebulizer or pressure cartridge Sympathomimetic Drugs - Nonselective adrenergic drugs - Have alpha, beta-1 (cardiac), and beta-2 (respiratory) activities - Epinephrine (Adrenalin, Asmolin) - Nonselective beta-adrenergic drugs - Have both beta-1 and beta-2 effects - Isoproterenol inhalation aerosol (Isuprel) - Selective beta-2 receptor drugs - Act primarily on beta-2 receptors in the lungs - Albuterol (Proventil, Ventolin) Xanthine Derivatives - Xanthine drugs include caffeine, theophylline, and theobromine - Actions - Relax smooth muscle (particularly bronchial smooth muscle) - Stimulate cardiac muscle and CNS - Increase diaphragmatic contractility - Promote diuresis through increased renal perfusion Other Respiratory Drugs - Prophylactic asthmatic agents - Cromolyn sodium (Intal) - Aerosol corticosteroid agents - Beclomethasone dipropionate (Vanceril inhaler, Beclovent) - Muscarinic antagonists - mucus reduction - Ipratropium (Atrovent) - Antileukotrienes - Montelukast (Singulair) Mucokinetic Drugs - Move respiratory secretions and sputum along tracheobronchial tree - Alter consistency of secretions so that they can more easily be removed from the body - Diluents (water, saline) - Expectorants (Mucomyst) - treatment of choice for Tylenol overdose
- 30. Oxygen - Treatment of hypoxia and hypoxemia - Colorless, odorless, and tasteless gas essential for sustaining life Respiratory Stimulants Direct stimulants (analeptics) - Act on medullary center of brain - Increase rate and depth of respirations Reflex respiratory stimulants - Spirits of ammonia only inhalation drug given as a reflex respiratory stimulant - Administered during cases of fainting Respiratory Depressants - Includes opium and barbiturate groups - Respiratory depression is a common side effect -respiratory distress causes hypoxia and hypercarbia - Seldom given to intentionally inhibit rate and depth of respiration Cough Suppressants - Cough is a protective reflex to expel harmful irritants - It may be: - Productive (removes airway secretions) - Nonproductive (dry and irritating) - Antitussive agents - Narcotic agents (codeine) - Nonnarcotic agents • Benzonatate (Tessalon) Antihistamines - Chemical mediator in most body tissues - Highest in the skin, lungs, and GI tract - Body releases histamine if exposed to antigen - Antihistamines compete with histamine for receptor sites - Prevent action of histamine H1 receptors - Act primarily on blood vessels and bronchioles H2 receptors - Act mainly on GI tract - Anticholinergic or atropine-like action - Primary clinical use is for allergic reactions - Also for motion sickness, sedative, antiemetic Examples - Dimenhydrinate (Dramamine) - Diphenhydramine (Benadryl) - Promethazine (Phenergan)
- 31. Serotonin - Naturally occurring vasoconstrictor - In platelets and in cells of brain and intestine - Serotonin is not administered as a drug - Has a major influence on other drugs and some disease states • Helpful in repairing damaged blood vessels • Stimulates smooth muscle contraction • Acts as a neurotransmitter in the CNS Drugs Affecting the GI System Antacids (Alka-Seltzer) - Antiflatulents (Mylicon) Digestants (Pancrease) - Emetics (syrup of ipecac) Antiemetics - Compazine, Phenergan Cytoprotective agents - Protect cells from damage - Cytotec, Carafate H2 receptor antagonists - Reduce volume and acidity of gastric acid - Zantac, Tagamet, Pepcid Proton pump inhibitors - Treat symptomatic gastroesophageal reflux disease, esophagitis - Nexium, Prevacid, Prilosec, Aciphex Drugs Affecting the Lower GI Tract Laxatives - Constipation causes: Neurological disease, pregnancy, rectal disorders, surgery, drug poisoning - Epsom salt, Dulcolax, Colace Antidiarrheals - Adsorbents (Pepto-Bismol) - Anticholinergics (Donnatal) - Opiates (paregoric) - Other (Lomotil, Imodium)
- 32. Drugs Affecting the Eye (Glaucoma - increased intraocular pressure) Antiglaucoma agents - decrease intraocular pressure - Pilocarpine, acetazolamide Mydriatic and cycloplegic agents - Treat inflammation, relieve pain - Atropine, homatropine ophthalmic solution Anti-infective/anti-inflammatory agents - Treat conjunctivitis, sty, keratitis Topical anesthetic agents - Prevent pain, rapid onset - Proparacaine HCl, tetracaine HCl Drugs Affecting the Endocrine System Drugs Affecting the Pituitary - Anterior & posterior pituitary gland hormones regulate secretion of other hormones Anterior pituitary drugs - Treat growth failure in children caused by growth hormone deficiency Posterior pituitary drugs - Treat symptoms of diabetes insipidus due to antidiuretic hormone deficiency Drugs Affecting the Thyroid - Thyroid hormone controls rate of metabolic processes - Required for normal growth and development - Parathyroid hormone regulates level of ionized calcium in blood through: - Release of calcium from bone - Absorption of calcium from the intestine - Rate of excretion of calcium by the kidneys
- 33. Thyroid Gland Disorders Goiter - Enlargement of thyroid Hypothyroidism - Thyroid hormone deficiency Hyperthyroidism - Thyroid hormone excess Drugs to treat hypothyroidism and prevent goiters - Thyroid (Synthroid) - Iodine products - Levothyroxine Parathyroid Disorders - Hypoparathyroidism and hyperparathyroidism - Drugs to treat hyperparathyroidism - Vitamin D - Calcium supplements Drugs Affecting the Adrenal Cortex Adrenal cortex secretes steroid hormones - Glucocorticoids (cortisol) • Raise blood glucose • Deplete tissue proteins • Suppress the inflammatory reaction - Mineralocorticoids (primarily aldosterone) • Regulate electrolyte and water balance - Sex hormones • Little physiological effect under normal circumstances
- 34. Drugs Affecting the Pancreas - Hormones of the pancreas Insulin - decreases blood sugar levels - Primary hormone that regulates glucose metabolism Glucagon - increases blood sugar levels - Stimulates liver to break down glycogen so that glucose is released into the blood • Also inhibits uptake of glucose by muscle and fat cells Insulin Preparations - Rapid acting - Insulin lispro - Insulum aspart - Short acting - Regular - Intermediate acting - Lente Insulin - NPH Insulin - Long acting - Ultralente - Insulin glargine Oral Hypoglycemic Agents - Amaryl - Glucophage - Glucotrol - Micronase Oral Combination Agents - Glucovance - Metaglip - Avandamet Hypoglycemic Agents - Glucagon - Diazoxide (Proglycem) - Dextrose - Oral glucose (Glutose, Insta-Glucose)
- 35. Drugs Affecting the Reproductive System - Includes synthetic and natural substances - Hormones - Female - Male Two hormones secreted by ovary: - Estrogen - Progesterone Supplemental estrogen indicated for: - Estrogen deficiency or replacement - Treatment of breast cancer - Prophylaxis for osteoporosis in postmenopausal women Progesterone (and synthetic progestins) used to: - Treat hormonal imbalance - Treat endometriosis - Treat specific cancers - Prevent pregnancy when properly used Oral Contraceptives - Oral contraception most effective form of birth control - Commonly known as “the pill” - Combination of estrogen and progesterone that results in suppression of ovulation - Available in several different forms Ovulatory Stimulants and Infertility Drugs - Absence of ovulation (anovulation) may be a pathological condition in women with abnormal bleeding or infertility Sometimes treated with: - Gonadotropins - Thyroid preparations - Estrogen - Synthetic agents
- 36. Drugs Affecting the Male Reproductive System - Testosterone therapy - Indicated for treatment of: • Hormone deficiency (e.g., testicular failure) • Impotence • Delayed puberty • Female breast cancer • Anemia Drugs Affecting Sexual Behavior - Drugs that impair libido and sexual gratification - Includes some antihypertensives, antihistamines, antispasmodics, sedatives, tranquilizers - Drugs that enhance libido and sexual gratification - Levodopa (L-dopa) - Sildenafil (Viagra) Drugs Used in Neoplastic Diseases - Antineoplastic agents - Used in cancer chemotherapy to prevent proliferation of malignant cells • Do not directly kill tumor cells • Interfere with cell reproduction or replication Examples • Adrucil • Mustargen • Amethopterin Antibiotics - Treat local or systemic infection - Kill or suppress growth of microorganisms - Disrupt bacterial cell wall - Disturb functions of cell membrane - Interfere with cell’s metabolic functions Includes: - Penicillin - Cephalosporins and related products - Macrolide antibiotics - Tetracyclines - Miscellaneous antibiotic agents
- 37. Antifungal Drugs - Some fungi are always present in body - Mouth, skin, intestines, and vagina - Prevented from multiplying through competition from bacteria and from actions of the immune system - Infection occurs when person becomes immunocompromised - Tinactin, Diflucan, Mycostatin Antiviral Drugs - Few effective drugs to treat minor viral infections - Viral infections range from harmless (e.g., warts) to serious diseases - Often have toxic effects - Acyclovir (Zovirax) - Zidovudine (Retrovir) - Lamivudine; zidovudine (Combivir) Protease Inhibitors - Complete mechanism of action not clear - Appear to inhibit replication of retroviruses (e.g., HIV) in acute and chronically infected cells - Side effects and adverse reactions - Indinavir (Crixivan) - Ritonavir (Norvir) Analgesic-Antipyretic Drugs → Antipyretics reduce fever → Analgesic-antipyretic drugs work by reversing the effect of the pyrogen on the hypothalamus → Analgesics act on peripheral pain receptors to block activation Examples - Acetaminophen - Aspirin Nonsteroidal Anti-inflammatory Drugs - Aspirin is the prototype of the NSAIDs - Inhibit enzymes so that prostaglandins (substances that promote inflammation and pain) are not formed - Aspirin - Ibuprofen - Naproxen - Ketorolac - Celecoxib Drugs Affecting the Immunological System - Immunosuppressants - Antirejection, anticancer, corticosteroid drugs - Immunomodulating agents - Serums - Vaccines
