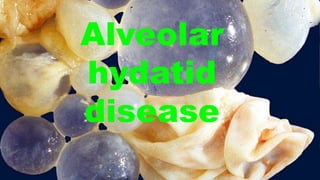
Alveolar hydatid disease
- 3. •
- 4. • Hydatid cyst disease (HCD) is caused by Echinococcus, a cestode of the Taeniidae family. An Echinococus is composed of a specialized attachment organ, the scolex, which contains a hook and suckers, a neck, and two to six reproductive segments (proglottids). Echinococcus is a few millimeters in length, rarely over 7 mm. Hydatidosis is characterized by the development of water cysts inside the liver, lung, and other visceral organs. Echinococcus oligarthrus is an extremely rare cause of human echinococcosis.
- 5. • Human echinococcosis (hydatidosis or hydatid disease) is caused by the larval stages of cestodes (tapeworms) of the genus Echinococcus. Echinococcus granulosus causes cystic echinococcosis (CE), the most frequently encountered pathogen in humans. Echinococcus multilocularis causes alveolar echinococcosis (AE), which is a rare pathogen in humans and the cause of a more disseminated form of alveolar HCD. Echinococcus vogeli causes polycystic echinococcosis. Echinococcus oligarthrus is an extremely rare cause of human echinococcosis. • Echinococcus oligarthrus is the cause of polycystic echinococcosis and found in Central Asia and South America. In general,
- 6. • These parasites in humans are particularly localized in the liver (75%) and the lungs (5% to 15%), but they can develop in other organs as well, causing significant clinical problems. The reason for their more common presence in the liver is due to the capture of the embryos in the sinusoids of the liver. An asymptomatic cyst is more common in the liver than in the lungs. • Unilocular hydatid disease usually manifests as a slow growing mass. Cysts in unconfined locations can attain a large size without interfering in vital functions, but small cysts in some locations may produce a significant mechanical compression of vital structures
- 7. • Based on the morphologic findings, cysts may be classified as the following: • type 1—simple cysts with no internal architecture; • type 2—cysts with daughter cysts and a matrix; • type 2a—round daughter cysts at the periphery; • type 2b—larger irregular-shaped daughter cysts almost occupying the entire volume of the mother cysts; • type 2c—oval masses with scattered calcifications and occasional daughter cysts; • type 3—calcified, or dead, cysts; and • type 4—complicated, or perforated, cysts.
- 8. •
- 9. •
- 11. • Fluid resuscitation (saline 0.9%) 500 mL per 500 mL (with a total of 1500 mL) and IV boluses of ephedrine (30 mg total) allowed only a slight improvement (NIP: 69/43 mmHg). Epinephrine boluses (100 μg to a total of 300 μg) were administered and relayed by continuous infusion (0.08 μg/ kg/min) via a central venous catheter. This therapeutic has stabilized the hemodynamic status (NIP: 109/56 mmHg and HR: 90 beats/min) and so continue the surgery. A bolus of 200 mg of hydrocortisone was administered. No need for additional bolus of epinephrine or an increase in infusion rate were required for the rest of the surgery. After removing of surgical draping, presence of skin signs all over the body has attracted attention of the team [Figures 1 and 2]. Diagnosis of anaphylactic shock was then strongly suspected
- 12. •
- 13. • CLINICAL FINDINGS Alveolar hydatid disease may show clinical manifestations similar to that of a slow-growing malignant tumor in the liver. The unilocular hydatid cyst is a slow- growing mass, which grows in the liver about 1 cm a year. Once the eggs pass the stomach, embryos are released and pass through the intestinal wall to reach the tributary veins of the liver, where they undergo vesicular transformation and develop into hydatids. If they pass the obstacle of the liver, they are arrested in the lung, where they can also become hydatids.
- 14. • If they have the capacity to pass beyond the lung, they can lodge in any organ. It has been shown that eggs can reach the lung via lymphatic vessels, by passing the liver through the ductus thoracicus. There is also evidence that the disease can be transmitted through the bronchi. Also, it has been theorized that extraparenchymal and intrathoracic hydatids may develop inside of the chest wall via transmission of the lymphatics of the chest wall.
- 15. • The parasite may destroy the liver parenchyma, bile ducts, and blood vessels, resulting in symptoms of biliary obstruction, portal hypertension, and necrosis of the central portion of the cyst with abscess formation. The growth of the germinal membrane into blood vessels produces metastasis in almost any organ, but they are more commonly found in the lungs and brain.3 Any necrotic mass located in the liver must include Echinococcus multilocularis in the differential diagnosis, especially for patients from suspected regions
- 16. •
- 17. • About 75% of infected individuals develop one or more cysts in the liver, and the right lobe of the liver is affected more often than the left.15 Cysts may also develop in the lungs, kidneys, spleen, brain, and musculoskeletal system. In most of the reported series, the lower lobes of both lungs are affected more often than the upper lobes.16 Cysts are usually solitary but may also be bilateral 19 When the embryo is arrested at an organ, the second larval stage (metacestode) starts. The natural course of this stage is a progressive growth. However, some cysts are reported to remain in a static position for years.20 Parenchymal tissue elasticity defines the growth rate of the cyst. It has been claimed that cysts grow faster in lungs than livers because the lung is softer and more elastic than the liver.
- 18. • Negative intrathoracic pressure may be another reason for faster growth in lung tissue. The embryo and cyst have a tendency to grow faster in pediatric lungs, based on the more common findings of giant cysts in children.21 Most of the patients are 20 to 60 years old, with a peak incidence in the third decade. There may be patients with involvement in multiple sites, most frequently the liver followed by the lungs. The clinical diagnosis of alveolar hydatid disease is more difficult than that of unilocular hydatidosis and the condition may often be mistaken for carcinoma of the lung
- 19. • Clinical findings depend on the perforated or intact status, size, location, and invasion and migration of the cysts. Intact cysts may be diagnosed with the symptoms of cough, dyspnea, and chest pain. Ruptured cysts may cause the expectoration of cyst contents, productive cough, fever, repetitive hemoptysis, and anaphylactic shock (Fig. 87.4). Hydatoptysis, or the expectoration of fluid from the cyst or membranous tissues of the cyst, was observed in 29% of the patients in one series.22 Although it has been reported to be a very rare cause of pulmonary nodules, this finding is not uncommon in endemic regions. In fact, in an article published by a Spanish group in the early 1980s, this presentation of the disease has been reported as the most common cause of solitary pulmonary nodules.22 Although the most common findings depend on the studies,
- 20. • the most common symptoms are cough (62%), chest pain (56%), expectoration (42%), fever (32%), vomica (26%), hemoptysis (25%), and dyspnea (24%).16 Anaphylactic shock may also occur (10%) in patients.16 Other uncommon presentations of lung hydatid disease include severe ascites, peripheral edema, and heart failure, which occurs in the event of severe chronic pulmonary hypertension and embolization into the pulmonary artery
- 21. • An acute occurrence of pleuritic chest pain and an increasing shortness of breath may signal acute pulmonary embolism due to a hydatid cyst.24 Biloptysis and pneumonia may be signs of bronchobiliary fistula due to liver hydatid cysts, which may indicate its penetration of the diaphragm and presence in lung tissue.25 When the cysts are located at the diaphragmatic surfaces of the lung, abdominal pain is likely to occur. Rupture of the cyst in the pleural space may cause pneumothorax and the presenting syndrome may be dyspnea and chest pain. In this case, anaphylactic shock and empyema in untreated patients may be unavoidable. Due to the fast expansion of the cysts in pediatric patients, hypoxemia and development failure may occur.
- 23. • A 42-year old male presented with liver hydatid cyst complicated by broncho-biliary fistula presented with coughing bile. Axial and coronal computed tomography scan images using liver window (A) and standard soft tissue window (B-D) show intercommunicating multiple liver cystic lesions with internal non-enhancing septations and peripheral calcifications within hepatic segments 8 and 7. The right lower lobe lung cystic lesion (asterisks) contains multiple air foci indicating bronchial communication with evidence of wide communication with the hepatic cystic lesion through the diaphragmatic defect (dashed arrows in A and C). A calcified hepatic lesion near the porta hepatis represents a healed hydatid cyst (arrow in D).
- 24. •
- 25. • A 48-year old male with mediastinal hydatid cyst presented with acute chest pain. A: Axial image of enhanced computed tomography angiogram shows a complex cystic lesion with thick wall (white arrows) that is predominately located in the left side of the posterior mediastinum with evidence small calcifications at the periphery of the lesions at the site of abutment with descending thoracic aorta. There is adjacent pleural effusion (white asterisk) and enhancing left lower lobe atelectasis (white asterisk); B, C: Axial and coronal T2 weighted images show a complex cystic lesion with thick dark rim (arrows) abutting the descending thoracic aorta with multiple peripheral daughter cysts of higher signal intensity compared to the intermediately hyperintenese matrix of the mother cyst. Magnetic resonance imaging findings are highly suggestive of hydatid cyst, likely primary given absence of evidence of lung and liver hydatid disease.
- 27. • An 82-year-old female with pulmonary artery hydatid cyst embolism presented with shortness of breath. A, B: Coronal images of enhanced computed tomography scan show right main pulmonary artery intraluminal cystic filling defects causing expansion and near occlusion of the artery with extension into the right interlobar pulmonary artery (white arrows). There is hepatic hydatid cyst with internal septation and daughter cysts and scattered wall calcifications (black arrows); C: Coronal image of T1 weighted magnetic resonance angiography confirms the presence of filling defect of low signal intensity within the right pulmonary artery and low signal intensity liver lesion (asterisks) with no evidence of contrast enhancement; D: Axial T2 weighted image with fat saturation shows right main pulmonary artery intra-luminal cystic filling defects of high signal intensity with septations suggestive of daughter cysts (arrow). Left pleural effusion is noted.
- 28. •
- 29. • Pericardial hydatid cyst. A, B: Axial and coronal contrast enhanced computed tomography images show a partially peripherally calcified cystic lesion (white arrows) along the inferior aspect of the heart and within the pericardial sac (dashed arrows) with mild mass effect and displacement of the right ventricle (black arrow). Small pleural effusions and ascites are shown (asterisks).
- 30. •
- 31. •
- 32. •
- 33. • DIAGNOSIS The combination of radiologic and serologic findings may enable successful diagnosis. As most of the patients are asymptomatic, incidental radiologic findings are common. Differential diagnoses include tuberculoma, peripheral carcinoma, and other lesions producing spherical formation in the lungs. Transthoracic needle aspiration biopsy (TTNAB) is never recommended when there is a hydatid cystic disease (HCD) in the differential diagnosis. TTNAB may cause rupture and spillage of the fluid contained in the cyst therefore resulting in anaphylactic shock.
- 34. • Bronchoscopy is unnecessary in patients with typical clinical and radiologic pictures, but may be considered in the case of an atypical presentation. When bronchoscopy is performed, it has been reported to detect pathologic findings at a rate of 70%, which mostly involves a whitish endobronchial lesion mimicking endobronchial tuberculosis with a caseous lesion.26 When a cyst becomes infected before or after rupture, the clinical findings may resemble unresolved pneumonia, tuberculosis, and an abscess or tumor of the lung
- 35. • Uncomplicat ed and intact, or unperforated , cysts may be diagnosed as round or oval-shaped lesions with regular fine margins.
- 36. • An oval- shaped, well- defined and rounded homogeneous density mass is observed in left lung. Chronic cough.
- 37. •
- 38. •A well-defined round shaped pleural based mass lesion is seen in the left side of the chest, It shows homogeneous opacity with smooth margins and no matrix of calcification detected, the findings are in favor of hydatid cyst (CT chest with contrast was recommended).
- 39. •A well-defined oval shaped large intra-pleural cystic lesion with numerous daughter cysts inside is seen in the left side of the chest. It showed fluid CT density, smooth margin, hypodense content relative to the capsule with a thin enhancing capsule, picture highly in favor of an uncomplicated pleural hydatid cyst. Both lungs clear with normal pulmonary vascular markings, no focal lesion. Normal mediastinum with normal mediastinal vasculature, no mass or enlarged LN.
- 40. • Axial C+ arterial phase Axial lung window
- 41. • Coronal
- 42. • The patient underwent thoracotomy and the findings of numerous cystic lesions within the pleura confirming the diagnosis of hydatid cysts.
- 43. • Two dense rounded well- defined shadows projected over the middle zones, one on each side. No signs of complicated pulmonary hydatid cyst. • Hila and mediastinum appear normal. • Both costophrenic angles are clear. • The heart is normal in size and shape.
- 44. • Presentation • Chronic cough with right hypochondrial pain since long time. Multiple well defined opaque cysts are seen within the right hemithorax. Some of them appear disintegrated.
- 45. • Unilocular cysts are seen with daughter cysts inside, they are the hall mark of hydatid disease.
- 46. •
- 47. • Hepatic hydatid cyst • Presentation • Abdominal • pain
- 48. • An oval-shaped, well-defined and rounded homogeneous density mass is observed in left lung. • Presentation • Chronic cough.
- 49. • Presentation • A 10 year old boy presented with cough.
- 50. Cyst wall crumpled and floating within uncollapsed pericyst that produce the water-lilly sign.
- 51. • Hepatic and pulmonary hydatid cysts • Presentation • Dyspnea Multiple hepatic cystic lesions are noted, with a larger cyst in the right lung.
- 52. • Presents with cough and hemoptysis. Large cavity with an air fluid level in left lung.
- 53. • Large cyst with an air-fluid level and crumpled laminated membrane lying dependently
- 54. •
- 55. • Large cyst with thick wall is seen at right upper lobe , another small cystic lesion also noted at lower lobe of the same side
- 56. •
- 57. • Hepatic, splenic and pulmonary hydatid cysts Multiple hepatic cysts with a large splenic cyst are seen. A complicated cyst also is noted at medial lobe of right lung. Small mass-like lesion also is detected at lower lobe of left lung.
- 58. • Radiographic features • CT • Generally, chest CT scan features include 2: • multiple or solitary cystic lesion (most common) • diameter of 1-20 cm • unilateral or bilateral • predominantly found in the lower lobes • Radiographic and CT features may differ in complicated and uncomplicated cysts. • Uncomplicated cysts are characterized by: • round or oval masses with well-defined borders • enhancement after contrast injection • hypodense content relative to the capsule • Complicated cysts may show: • meniscus sign or air crescent sign • cumbo sign or onion peel sign • water-lily sign • consolidation adjacent to the cyst (ruptured cyst)
- 59. • MRI • T1: hypointense • T2: hyperintense • The cyst capsule is hypointense on T2 weighted image (hypointense rim sign), isointense on T1 weighted images, and shows mild postcontrast enhancement. The folded membranes within cysts are T2 hypointense 8. • Ultrasound • Double-layered wall in univesicular cysts and a double- layered septum in cases of multivesicular cysts ( wall sign) 9 • Other less common thoracic hydatid manifestations include invasion of the mediastinum 4, pericardium, chest wall 5, cardiovascular system, or inferior vena cava 6.
- 60. • Chest computed tomography (CT) provides the best radiologic study. Hydatid cysts generally appear as unilocular, thin-walled cysts in the lung fields. Intact cysts may provide 3 to 18 HU density whereas perforated cysts may have a higher HU due to the occurrence of fibrosis. Differential diagnosis includes benign and malignant lung abscess. Daughter cysts and calcification are rarely seen in the chest CT of patients. Magnetic resonance imaging (MRI) may have diagnostic superiority if the cyst is located at the basal part of the right lower lobe and may clarify whether these cysts originate from the dome of the liver or dumb-bell-shaped cysts. Although pneumoperitoneum has been used for differential diagnosis of such cysts in previous years, MRI, chest CT, and ultrasonography (US) currently provide better diagnosticy
- 61. •
- 62. •
- 63. •
- 64. • MICROBIOLOGY AND SEROLOGY Findings of scolices at the sputum examination may be diagnostic in patients with perforated hydatid cysts. • Most of the serologic tests have been used in the diagnosis of HCD caused by Echinococcus granulosus. Previously, laboratory diagnosis was based on the Casoni intradermal or the Weinberg complement fixation tests, which have been discontinued clinically due to their lower sensitivity and specificity. Serologic tests are used only to confirm the diagnosis provided by chest imaging studies Alternatively, the indirect hemagglutination antibody (IHA) test may be considered more sensitive compared to the above-mentioned tests, as suggested by Garabedian and Kagan.27,28 However, IHA has limitations like false positivity in the presence of other helminthic infection, cancer, and chronic immune complex disease.
- 65. • The most sensitive test to HCD is reported to be immunoglobulin G enzyme–linked immunosorbent assay (ELISA) test with a sensitivity of 85.3%.26 Data show that ELISA is superior to IHA in sensitivity for the initial screening of suspected HCD cases.27 Laboratory tests are recommended in either highly suspected cases or postoperative follow-up situations. It has been reported that antibody production increases during the first 4 to 6 weeks after surgical intervention, followed by a decrease during the next 12 to 18 months. 26 In patients with recurrent HCD, the antibody levels may remain similar to the preoperative levels.
- 66. •
- 68. •
- 69. • Eosinophilia is present in 10% to 30% of the cases and the number of eosinophils increases when the cyst ruptures.26 Assay performance depends on the nature of the test and the antigen used; it is also associated with the characteristics of the disease in the involved organs, the number of cysts, and the presence of any cystic complications.31,32 • Recently, several studies have demonstrated that synthetic peptides and recombinant antigens derived from the two major components of the cystic fluid, antigen B (AgB) and Ag5, have been previously proposed for use as reproducible antigens to improve test reliability; indeed, they allow better standardization.33,34 • The p176 antigen derived from AgB is a 38-mer corresponding to the N-terminal extension of the subunit AgB8/1.35 An ELISA using p176 has demonstrated good performance for diagnosis of HCD, with sensitivities between 74% and 80% and specificities between 79% and 93%.35 However, data on serologic diagnosis of lung HCD are scarce, and the published p176 studies do not allow estimations of its sensitivity or provide further details for pulmonary cases
- 70. • TREATMENT The treatment of echinococcosis relies on surgery and/or chemotherapy depending on a variety of factors: size, location, viability status, interaction between the expanding parasite and adjacent host tissue, potential complications related to the rupture of the hydatid cyst, associating bacterial or fungal infections, and spillage of protoscolices.36,37 Radical excision of the cystic mass represents the traditional and most effective treatment strategy. • For inoperable cases, chemotherapy with benzimidazoles, albendazole, mebendezol, and heterocyclic pyrazinoisoquinoline derivative praziquental, all remain valuable options.37 • Percutaneous treatment options have been offered to liver hydatid cysts, but this treatment has never been an option for the treatment of lung hydatid cysts due to the possibility of anaphylactic reactions.
- 71. • Medical treatment with benzimidazoles is valuable in patients with smaller hydatid lesions, with disseminated disease—including secondary lung or pleural hydatosis—with poor surgical risks, and when there is intraoperative spillage of hydatid fluid.38,39 Medical treatment and aspiration technique for large cysts, in the same fashion as in the liver, fail to give durable and safe outcomes in pulmonary hydatid disease.
- 72. •
- 73. • A meta-analysis consisting of 14 reports and 4,255 patients with HCD demonstrates that surgery results in excellent outcomes with an acceptable mortality rate of 1.4%.40 Similarly, perioperative morbidity was reported to be 0% to 17% among 3,433 patients who had surgical intervention.40 Accordingly, surgery provides the best cure for the treatment of hydatid disease in lungs. Medical treatment may only be reserved for patients whose disease cannot be eradicated by surgery due to dissemination or who cannot tolerate lung surgery
- 74. • dissemination
- 75. • Case presentation • A forty five year old lady presented with chronic dull aching pain with gradually increasing lump in the epigastric and pelvic region since 3 years. A well defined, firm mass of about 20 × 20 centimeters was palpable in epigastrium extending more on right hypochondrium, probably arising from left lobe of liver. A similar mass was palpable in the hypogastrium while multiple small nodular masses palpable in the right iliac fossa and lumbar region. Detailed inquest revealed a 5 year old incidence of blunt abdominal trauma, while working in her farm. The ultrasonography and CT scan (See Figure 1) showed multiple thin walled cysts of varying size involving left lobe of liver, peritoneal cavity, omentum and mesentery. Cysts showing internal septae and peripheral tiny calcific foci were also seen extending into pelvis around uterus, adnexae and retro-uterine cervical region, markedly compressing distal descending colon, sigmoid colon and rectum. Ileal loops were compressed and displaced superiorly. Serology for hydatid cyst disease was positive with ELISA test.
- 76. • Two courses of 4 weeks of Albendazole (15 mg/kg/day) were given with the interval of 1 month. The follow up after 1 month did not show any decrease in the size of the cysts and decision of laparotomy was taken. Peritoneal cavity was crammed with cysts ranging from 1 to 12 centimeters (See Figure 2). Omentum was studded with cysts (See Figure 3) which was incised and cysts were picked up (See Figure 4). A superficial cyst found in the left lobe of liver was opened with small incision and the hydatid fluid and daughter cysts were drained. After the excision of germinal membrane the cavity was masupialized. Later, the pelvic cavity was exposed and cysts adherent to adnexa, uterus, broad ligament, urinary bladder and rectum were removed. More than 250 cysts of different sizes were removed from the abdomen (See Figure 5). Patient died of anaphylactic shock within few hours of operation.
- 77. •
- 78. •
- 79. •
- 80. • The treatment of choice for localized hydatid cysts in liver or lungs is principally surgical while the therapy for disseminated peritoneal hydatidosis remains medical [5]. Therapy with albendazole or praziquantel remains the mainstay of medical therapy. After medical treatment, the hydatid cysts show gradual reduction in cyst size and number and the follow up is advisable with Ultrasonography or CT scan. In our case despite of sufficient medical treatment the cyst size and number did not reduced and hence surgery remained the final resort. Surgery can be performed with removal of the cyst after sterilizing the cyst with formalin or alcohol. However, pre- and post-operative 1-month courses of albendazole or 2 weeks of praziquantel should be considered in order to sterilize the cyst, decrease the chance of anaphylaxis, decrease the tension in the cyst wall and to reduce the recurrence rate post- operatively [6]. Intra-operatively, the use of hypertonic saline or 0.5% silver nitrate solutions before opening the cavities tends to kill the daughter cysts and therefore prevent further spread or anaphylactic reaction.
- 81. •The effect of combination therapy with albendazole and praziquantel on hydatid cyst treatment
- 82. • The standard therapy of hydatid cyst is surgery but, in nonoperable patients and multiple organ involvement, medical therapy may be more useful. The efficacy of drugs especially in short-term treatment of hydatid cyst is unknown. This study was carried out to evaluate the effect of combination therapy with albendazole and praziquantel in the treatment of hydatid diseases. In a nonrandomized quasi- experimental study, nine patients with multiple hydatid cysts were treated with albendazole (400 mg/twice a day) and praziquantel (40 mg/kg per day) twice a week for 4 weeks. This regimen was repeated for three courses with a 2-week interval between each one. The average follow-up period after treatment was 18 months. Response to treatment was assessed through the observation of the symptoms and radiologic findings (computed axial tomography scan, sonography, X-ray). Symptoms disappeared in seven (77.8%) patients and improved partially in two (22.2%) patients. Radiological assessment showed significant improvement in five (55.6%) and partial improvement in four (44.4%) patients. Combination therapy with albendazole and praziquantel is effective in the treatment of hydatid cyst and can be used as an alternative to surgery in disseminated and nonoperable cases.
- 83. • albendazole
- 85. •
- 89. •
- 90. • Aydin technique. Modified capitonnage was also performed us- ing 2–0 or 3–0 absorbable polyglactin
- 91. • Postoperative follow-up Prophylactic empirical antibiotic treatment with amoxicillin-clav- ulanic acid was initiated in all cases postoperatively. Chest tubes were removed when there was no air leak and the drainage was <100 ml in 24 h. All patients received 15 mg/kg/day albendazole treatment in 2 cycles of 15 days after discharge. A drug-free rest period of 10 days was applied between the 2 cycles. The follow- up of the patients was scheduled as 15th day after discharge, at the end of the first month and 3 months, and then every 6 months. In the first 2 follow-ups, the evaluation was made with complete blood count and liver function tests besides posteroan- terior chest radiograph and physical examination. The effect of modified capitonnage on surgical outcomes was evaluated by posteroanterior chest radiograph regarding postoperative com- plications such as prolonged air leak (>7 days), emphysema for- mation, atelectasis, residual cavity, recurrence and length of hospital stay.
- 92. •
- 94. •
- 95. • successfully contemplating a surgical technique for pulmonary hydatid disease: 1. The primary objective of the surgery is to evacuate pericyst of endocyst and its contents in toto. The cure rate and recurrence rate depend on extent of removal of cyst and its contents.2,3 There is a developing consensus that pericyst is generated in response to host response and need not essentially removed.3 2. The closure of bronchial openings within the residual cyst cavity and management of the residual cavity itself is important in order to prevent prolonged post-operative air leak and empyema formation.5 3. The lung parenchyma should be preserved as far as possible, especially in children and endemic areas, where risk of recurrence is a real concern.11
- 96. • 4. In complicated cysts resection may offer low post-operative morbidity in contrast to conservative surgery but case selection remains challenging
- 97. • 5. If the intent of surgery is to remove the cyst in intact form, it is better to stop medical therapy 6 weeks prior to surgery and if we are dealing with a ruptured, complicated cyst, it is better to start with pre-operative medical therapy, which should continue post-operatively.10,12 • 6. All of the necessary precautions should be made per-operatively to deal with accidental rupture of the cyst. Saline soaked towels are good option, which should be placed in immediate vicinity to avoid generalized contamination. If the cyst ruptures per-operatively, the spillage should be contained as much as possible and the anaphylactic shock, if occurs, should respond in most cases to steroids and octreotide infusion coupled with adequate hydration titrated with atrial pressure monitoring. post-operatively, such patients need long-term prophylaxis against the recurrence and should undergo regular surveillance
- 98. •
- 99. • Modified Barrett’s capitonnage technique, a hydatid cyst is exposed with conventional thoracotomy though 6th intercostal space (a), overlying lung parenchyma is incised (b) and the cyst is carefully dissected bluntly and is pushed out with positive pressure ventilation (c). The cyst cavity walls are gently retracted and bronchial openings are secured with non-absorbable nylon stitches (d). The cyst walls are buttressed together with interrupted nylon stitches- capitonnage (e) and finally the healthy edges of the incised lung parenchyma are re approximated with non-absorbable stitches (f).
- 100. •
- 101. • the steps of surgical evaluation may be based on (1) the selection of the order of operations based on whether the cysts are bilateral or are located in the liver and other organs such as the heart and brain; (2) the selection of incision types, including thoracotomy, median sternotomy, thoracoabdominal incisions, and video-assisted thoracoscopic surgery; (3) the timing of the surgery in relation to the use of medication; (4) the selection of intraoperative approach for the excision of the cyst; and (5) the selection of the technique for the closure of the pericystic cavity or the selection to not make any closure.
- 102. • Selection of the Order of the Operations It is always necessary to search for additional cysts in patients with liver or lung hydatid cyst. The need to undertake a combined operation on both the hemithoracic cavity and the liver may be considered. When bilateral cysts are diagnosed, the operation can be done in two stages. The first thoracotomy can be performed based on the side that appears to have a higher risk of rupture or more complicated.41 In case of accompanying cysts in the liver, lung surgery should be performed first. Likewise, in patients with hydatid disease in other organs, lung resection always represents a priority. If the liver cyst is located at the dome of the liver, a right thoracotomy and transdiaphragmatic resection may be a good option for the treatment of both sites. The decision as to which cyst should be resected first is generally based on the cyst size and its susceptibility to rupture, and disseminate, as well as the importance of the organ in which each cyst is located.42 When an intracardiac cyst is present, the operation should be performed as soon as possible; if technically possible, it should be resected with the lung cyst at the same settings through a median sternotomy. • Median sternotomy may be a good choice for the treatment of bilateral hydatid cysts when the cysts are located anteriorly. • Transsternal bilateral anterior thoracotomy may be considered for both cysts located anteriorly or posteriorly and hydatid cysts in the heart. However, it should be decided very carefully, in order to minimize pain and possible postoperative respiratory problems
- 103. • VATS treatment of HCD can be reserved for the treatment of superficial and small- to moderate-sized cysts with peripheric locations in the lung. In addition, surgeons should consider suturing rather than tissue glue for the closure of bronchial openings
- 104. • Timing of the Surgery in Relation to the Use of Medication In the last three decades, mebendazole has been widely recommended as an adjuvant treatment following the resection of cysts. After the first pilot study was published, the general recommendation was to administer mebendazole 7 to 10 days before surgery
- 105. • When the cyst is intact and there appears to be no risk for dissemination, 1 month of treatment after surgery is recommended. • When the cyst is ruptured and intraoperative dissemination is suspected, it is recommended to continue treatment for 3 to 6 months. When dissemination is confirmed and the total or partial resection of the cystic lesion is impossible, it is recommended to continue the administration of mebendazole until there is no more radiologically evident cyst. • If the intent of surgery is to remove the cyst in its intact form, stopping the medical treatment 6 weeks before surgery is reasonable. • If surgery is planned for a ruptured or complicated cyst, it is better to start the therapy in the preoperative period and continue postoperatively.
- 107. • Even in patients with acute infection, lobectomy should not be considered as the first therapeutic option. In the literature, the lobectomy rate is reported to range from 0.5% to 45%.49 According to the same chapter in the previous edition of this book, the indications for lobectomy are as follows: A large cyst involving more than 50% of the lung, a cyst with severe suppurative pulmonary infection not responding to medical treatment, multiple unilobar cysts, and sequelae of hydatid disease such as fibrosis, bronchiectasis, severe hemorrhage, and destroyed lung.49 According to our experience, the size of the cyst should not indicate per se lobectomy or pneumonectomy as demonstrated in a previous report on 47 patients
- 108. • In this series, only three patients required lobectomy. In addition, pediatric and adult patients may show differences in terms of need for resection. In fact, in a retrospective review of their own series, Dincer50 and colleagues observed that the resection rate was higher in the pediatric population [1.5% in adults and 16% in children (p > 0.001)]. In their experience, the indications for parenchymal resection were giant cysts occupying the entire lobe, multiple cysts, and an unexpandable lobe after the excision of the cyst. In addition, they observed no increase in morbidity when parenchyma-saving techniques were used for cysts occupying more than 80% of a lobe. In our opinion, while segmentectomies may be acceptable in selected cases, the decision for a lobectomy must be individualized and taken by a most experienced surgeon
- 109. • The remaining lung is often functional when bronchial secretions are suctioned and the lung is inflated with higher inspiratory pressures. For this reason, even if a cyst occupies more than 50% of the lobe, the quality of parenchyma should be evaluated before proceeding to the resection with only one important exception—a massive hemoptysis.
- 110. •
- 111. • Patients with major hemoptysis, but without a preoperative definitive diagnosis, may undergo a lobectomy yielding a final pathologic result of hydatid disease. In addition, parenchyma-sparing procedures may be more complicated in case of a major hemoptysis. In our experience, two patients required a lobectomy due to massive hemoptysis whereas in additional two patients, a lobectomy was necessary due to intrapulmonary arterial hydatid disease. Even if it has not been mentioned in the literature, intrapulmonary arterial migration of the cysts that have strong attachments to pulmonary arterial intima and wall and are located at the distal part of the pulmonary arterial system may require a segmental or lobar resection
- 112. • If the intrapulmonary arterial dissection of the hydatid cysts does not reveal high-quality backflow due to an obstruction of the distal pulmonary artery (which is an important finding in our experience), a resection may be mandatory considering segmental resection as the first option.
- 113. • The preferred surgical methods in our clinic are enucleation, cystotomy, and capitonnage. We consider the enucleation technique if the dissection plane is clearly demarcated without strong adhesions, which possibly decreases the risk of rupture of the cyst (Fig. 87.14). In general, however, we perform cystotomy and aspiration. We prefer to aspirate the fluid in the cyst using a three-way stopcock attached to a 50 mL syringe and a line (Fig. 87.15A). The aspirated fluid is excreted to a bottle outside the operating field via the line (Fig. 87.15B). When the cyst is decompressed and the tension relieved, the parenchyma covering the cyst is incised and the endocyst is removed without causing spillage (Fig. 87.15C). If the cyst is located at the periphery of the lung, this procedure may be performed with VATS. In short, the contemporary surgical trend is to manage the disease with conservative surgical procedures
- 114. • FIGURE 87.13 Distal intrapulmonary arterial migration of the cysts may require anatomical resection. Our cystectomy trials from distal pulmonary arteries did not provide a backflow from the arteries due to strong attachments to pulmonary arterial intima. Then the smallest anatomical resection should be considered
- 115. •
- 116. •
- 117. • Cystotomy with capitonnage has been the most commonly performed procedure for the past 60 years with acceptable cure rates and perioperative morbidity. The literature suggests that capitonnage has been performed since 1952 with the intention to decrease the rate of empyema and postoperative prolonged airleak. However, this view has been questioned by several groups. In fact, capitonnage is reported to cause incomplete lung expansion and facilitate atelectasis.51 Unfortunately, some of those who perform only closure of the bronchial openings without a capitonnage have failed to produce better results. Accordingly, we and many authors still think that capitonnage should not be abandoned when treating deeply located intraparenchymal HCD. In this context, meticulous surgical technique is mandatory to avoid inadvertent obliteration of the neighboring bronchi. However, we prefer to close the bronchial openings only without capitonnage if the cyst is located at the fissural and diaphragmatic surfaces of the lungs
- 118. •
- 119. • Massive Hemoptysis Patients may present with severe hemoptysis. An emergency chest CT may demonstrate a parenchymal mass, often without any sign of hydatid disease (Fig. 87.17). An emergency bronchoscopy should be performed in the operating room readied to continue emergency surgery (Fig. 87.18). As a rule, these patients require a lobectomy. If a pneumonectomy is required, the most experienced surgeon should take over and, by isolating the main pulmonary artery and the pulmonary veins of the ipsilateral side, open the cavity, repair the bronchial openings and the artery through the cyst cavity, and perform the appropriate arterial treatment
- 120. •
- 121. • Cysts in the Pulmonary Artery (in the Main and Small Vessels) Cysts may migrate to the main pulmonary artery and cause embolism-like symptoms. In this setting, often a pulmonary angio-CT is diagnostic. In endemic regions, dyspnea with HCD in the lung parenchyma may be a sign for the need of an evaluation of the pulmonary arterial system. Operative planning requires cardiopulmonary bypass techniques and generally performed by the cardiac pulmonary thromboendartectomy teams. When the migrated cyst is located at the periphery of the lung in the pulmonary artery, parenchyma-saving procedures like arteriotomy and enucleation of the cyst may or may not work. At this point, lung resections may be required.
- 122. • Case Report of Hydatid Cyst in the Pulmonary Artery Uncommon Presentation: CT and MRI Findings
- 123. • An 86-year-old female patient with a history of hepatic hydatid cyst since 2012 presented in November 2016 with a history of productive cough, yellowish-green sputum with mild shortness of breath, and loss of appetite. She had no complaints of chest pain, fever, palpitations, nausea, or vomiting and did not report any change in bowel habits or urinary symptoms. The patient was from a rural area. She had a history of long-term antiparasitic medication; however, details about the indication for and type and course of therapy were not available in the medical records. On respiratory examination, the lungs were found to be clear with good air entry bilaterally; fine crepitation was noted. The patient was admitted for investigation. Sputum culture showed scanty growth of normal respiratory flora, and rhino virus was detected in nasal swab culture. Chest X-ray showed a mass-like opacity in the right lower zone, in the right paracardial area. A nonhomogenous airspace opacity was observed in the left lower lung zone associated with a small left pleural effusion that indicated atelectasis or infection as differential diagnosis. Thoracic computed tomography (CT) was performed to investigate the mass-like opacity in the right lower zone. The CT showed multiple intraluminal cystic filling defects in the right main pulmonary artery and right lobar branches, mostly pulmonary artery hydatid cysts (see Figures 1 and 2). There was one large cyst in the right lower lung lobe representing a parenchymal hydatid cyst and another large cyst existed with air in the left lower lobe representing hydatid cyst in the left lung (see Figure 3).
- 124. • There was minimal bilateral pleural effusion, more on the left side. We conducted magnetic resonance imaging (MRI) of the thorax, which confirmed the presence of the cystic lesion within the right pulmonary trunk extending to the right lower lobe, showing low signal intensity on T1 and high intensity on T2 images with septation (see Figures 4 and 5). Parenchymal hydatid cysts were noted in the bilateral lower lobes, with the presence of adjacent atelectasis and small pleural effusion on the left side (see Figure 6). Images of the upper abdomen confirmed the large hydatid cyst in the right liver lobe. Surgical intervention was discussed with the family and they decided against it. The patient was discharged on oral albendazole 400 mg twice daily and oral praziquantel 1800 mg twice weekly. After ten months, repeat CT and MRI showed mild regression in size of both, the right main pulmonary artery and left sided parenchymal hydatid cysts. Praziquantel was stopped and presently the patient is on therapy with oral albendazole 400 mg twice daily.
- 125. • (a-b) CT axial images show pulmonary artery with multiseptate hydatid cysts (red arrows), seen in the right main pulmonary artery and the lower lobar branches of the right pulmonary artery, along with other parenchymal cysts (blue arrows).
- 126. • Liver Complicated Cysts Causing Bronchobiliary Fistula Bronchobiliary fistula is an abnormal communication between the biliary and bronchial tree. It may occur as a natural complication of liver HCD and after a liver surgery for various reasons including hydatid disease of the liver.58 Bilioptysis is the most common and prominent sign in this condition. Other possible signs are cholangitis, jaundice, and cutaneous fistula.59 Bilioptysis is an uncommon finding that may cause septic or chemical injuries to the lung. The most important procedure is to stop the communication between the lung and liver. Due to the increased bile pressure and negative suction pressure of the ipsilateral thoracic cavity, bile flows toward the lung.
- 127. • The amount of bile secreted from the liver is 620 mL/day. The lung should be isolated from the bile flow either by ERCP or percutaneous techniques. ERCP shows the obstruction in the bile system and the leak. Possible techniques to overcome the obstruction are sphincterotomy alone or in combination with stenting. Octreotide may be used as an adjunct to endoscopic treatment.60 When the sepsis is recovered, the lung should be separated from diaphragm. The liver should be repaired by the liver surgeon or a drainage system should be reconstructed through the abdominal wall. Drains should be placed over the dome of the liver and under the diaphragm before the diaphragmatic closure and the appropriate lung resection (Fig. 87.19). The drains should be removed when bile drainage has completely ceased.
