glaucoma and cataract.pdf
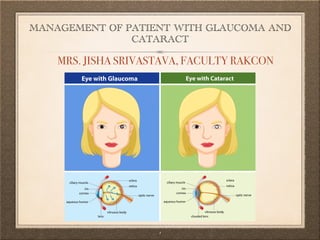
- 1. MANAGEMENT OF PATIENT WITH GLAUCOMA AND CATARACT  1 MRS. JISHA SRIVASTAVA, FACULTY RAKCON
- 2. OBJECTIVES  2 After the class the students will be able : Explain the structures and function of eye. Explain the age a ff ect on vision. Describe the de fi nition , etiology, risk factors, pathophysiology, medical management, surgical management and Nursing management of Glaucoma. Describe the de fi nition , etiology, risk factors, pathophysiology, medical management, surgical management and Nursing management of cataract. List down the health education for Glaucoma and cataract.
- 3. ANATOMY AND PHYSIOLOGY OF EYE
- 4. ANATOMY AND PHYSIOLOGY OF EYE External structures The bony orbit (eye socket) The orbit is formed from portions of the frontal, lacrimal, ethmoid, maxillary, zygomaticus, sphenoid and palatine bones.  4
- 5. ANATOMY AND PHYSIOLOGY OF EYE External structures The eyeball is moved by six ocular muscles The four rectus muscles (the medial, lateral, superior, and inferior) move the eyes horizontally and vertically. The two oblique muscles (superior and inferior) rotate the eye in circular movements to allow vision at all angles. The upper and lower eyelids are folds of skin that close to protect the anterior eyeball. When the eyelids close, they distribute tear fi lm  5
- 6. ANATOMY AND PHYSIOLOGY OF EYE External structures The elliptic space between the two open lids is the palpebral fi ssure . The corners of the fi ssure are called the canthi. The medial, or inner canthus is next to the nose; the lateral, or outer, canthus is the outside corner.  6
- 7. ANATOMY AND PHYSIOLOGY OF EYE External structures The lacrimal gland, in the upper lid over the outer canthus, produces tears that reach the eyeball through secretory ducts. Tiny openings (puncti) in both the upper and lower lids at the inner canthus direct tears to the lacrimal sac. The nasolacrimal duct directs the fl ow of tears into the nose.  7
- 8. Internal Structures The conjunctiva is a thin transparent layer of mucous membrane that lines the eyelids and covers the eyelid . The cornea is a transparent avascular structure with a brilliant, shiny surface. It is convex in shape, is about 0.5 mm thick, and acts as a powerful lens to bend and  8 ANATOMY AND PHYSIOLOGY OF EYE
- 9. Internal Structures The cornea is composed of fi ve layers. It derives oxygen from the atmosphere. A rich network of nerve fi bers in the outer layer (epithelium) produce sensation of pain whenever the fi bers are exposed or stimulated.  9 ANATOMY AND PHYSIOLOGY OF EYE
- 10. Internal Structures The sclera is the fi brous protective coating of the eye. It is white, dense, and continuous with the cornea. ln children, the sclera is thin and appears bluish because of the underlying pigmented structures. In old age, it may become yellowish from degeneration.  10 ANATOMY AND PHYSIOLOGY OF EYE
- 11. Internal Structures The uveal tract, the middle vascular layer of the eye furnishes the blood supply to the retina. The lens is a biconvex, avascular, colourless, and almost completely transparent structure, about 4 mm thick and 9 mm in diameter. The lens is surrounded by a  11 ANATOMY AND PHYSIOLOGY OF EYE
- 12. Internal Structures The vitreous body is a clear, avascular, jelly like structure, vitreous chamber. It helps maintain the shape and transparency of the eye.  12 ANATOMY AND PHYSIOLOGY OF EYE
- 13. Internal Structures Retina: The retina is a thin, semitransparent layer of nerve tissue that forms the innermost lining of the eye. It consists of 10 distinct layers of highly organized, delicate tissue. The retina contains all the sensory receptors for the  13 ANATOMY AND PHYSIOLOGY 1. Inner limiting membrane 2. Nerve fiber layer (NFL) 3. Ganglion cell layer 4. Inner plexiform layer 5. Inner nuclear layer 6. Middle limiting membrane 7. Outer plexiform layer 8. Outer nuclear layer 9. External limiting membrane 10. The layer of rods and cones
- 14. Internal Structures Optic Nerve and Neural Pathways The optic nerve is located at the posterior portion of the eye and transmits visual impulses from the retina to the brain. The head of the optic nerve (optic disc) can be Seen by ophthalmoscopic examination. The optic nerve* contains no sensory receptors (rods or cones) and represents a blind spot in the eye.  14 ANATOMY AND PHYSIOLOGY
- 15. FUNCTION OF THE VISUAL Transmission of light Visual receptors of Retina: Cones and Rods Image processing  15
- 16. The major visual changes with ageing include decreases in Visual acuity. Tolerance of glare. Ability to adapt to dark and lightPeripheral vision. Each of these decreases is related to changes in the eye structure and each a ff ects the quality and intensity of the light able to reach the retina. EFFECTS OF AGEING ON VISION  16
- 17. GLAUCOMA
- 18. DEFINITION Glaucoma is a group of ocular conditions characterised by optic nerve damage. The optic nerve damage is related to the IOP caused by congestion of aqueous humor in the eye. There is a range of pressures that have been considered “normal” but that may be associated with vision loss in some patients.  18
- 19. INCIDENCE It is estimated that at least 2 million Americans have glaucoma and that 5 to 10 million more are at risk . Older than 40 years of age, and the incidence increases with age. Men than women African American and Asian populations. There is no cure for glaucoma, but research continues  19
- 20. ETIOLOGY Glaucoma is the result of damage to the optic nerve. As this nerve gradually deteriorates, blind spots develop in visual field. Elevated eye pressure is due to a buildup of a fluid (aqueous humor) that flows throughout the inside of eye. When fluid is overproduced or the drainage system doesn't work properly, the fluid can't flow out at its normal rate and eye pressure increases. Glaucoma tends to run in families.  20
- 21. RISK FACTORS Family history of glaucoma African American race , Black, Asian or Hispanic Older age Diabetes Cardiovascular disease Migraine syndromes Nearsightedness (myopia)  21
- 22. RISK FACTORS Eye trauma or eye surgery Prolonged use of topical or systemic corticosteroids Having high internal eye pressure (intraocular pressure) High blood pressure and sickle cell anemia Having corneas that are thin in the center Being extremely nearsighted or farsighted Having had an eye injury  22
- 23. CLASSIFICATION Primary and secondary glaucoma refer to whether the cause is the disease alone or another condition.  23
- 24. CLASSIFICATION Acute and chronic refer to the onset and duration of the disorder.  24
- 25. CLASSIFICATION Open (wide) and closed (narrow) describe the width of the angle between the cornea and the iris, anatomically narrow anterior-chamber angles predispose people to an acute onset of angle closure glaucoma.  25
- 26. A. PRIMARY OPEN ANGLE The most common form, is a multifactorial disorder that is often genetically determined, bilateral, insidious onset slow in progress. Referred to as see the "thief in the night" because no early clinical manifestations are present to alert the client that vision is being lost. Aqueous humor flow is slowed or stopped because of obstruction by the trabecular meshwork is slowed. Usually bilateral, but one eye may be more severely affected than the other. In all three types of open-angle glaucoma, the anterior chamber angle is open and appears normal.  26
- 28. A. PRIMARY OPEN ANGLE
- 29. B. ANGLE-CLOSURE An acute attack of angle-closure glaucoma can develop only in an eye in which the anterior chamber angle is anatomically narrow. The attack occurs because of a sudden blockage of the anterior angle by the base of the iris Obstruction in aqueous humor outflow due to the complete or partial closure of the angle from the forward shift of the peripheral iris to the trabecula. The obstruction results in an increased IOP.  29
- 31. B. ANGLE-CLOSURE 1. Acute angle-closure glaucoma (AACG): Rapidly progressive visual impairment, periocular pain, conjunctival hyperemia, and congestion. Pain may be associated with nausea, vomiting, bradycardia, and profuse sweating. Reduced central visual acuity, severely elevated IOP, corneal edema. Pupil is vertically oval, fixed in a semidilated position, and unreactive to light and accommodation. 
- 32. B. ANGLE-CLOSURE 1. Acute angle-closure glaucoma (AACG): Ocular emergency; administration of hyperosmotics, azetazolamide, and topical ocular hypotensive agents, such as pilocarpine and beta-blockers (betaxolol). Possible laser incision in the iris (iridotomy) to release blocked aqueous and reduce IOP. Other eye is also treated with pilocarpine eye drops and/or surgical management to avoid a similar spontaneous attack. 
- 33. B. ANGLE-CLOSURE 2.Subacute angle-closure glaucoma: Transient blurring of vision, halos around lights; temporal headaches and/ or ocular pain; pupil may be semi-dilated. Prophylactic peripheral laser iridotomy. Can lead to acute or chronic angle-closure glaucoma if untreated.  33
- 34. B. ANGLE-CLOSURE 3.Chronic angle-closure glaucoma : Progression of glaucomatous cupping and significant visual field loss; IOP may be normal or elevated; ocular pain and headache.Management includes laser iridotomy and medications.  34
- 35. C. NORMAL-TENSION Optic nerve becomes damaged even though eye pressure is within the normal range. No one knows the exact reason for this. Sensitive optic nerve, or may have less blood being supplied to optic nerve. Caused by atherosclerosis — the buildup of fatty deposits (plaque) in the arteries — or other conditions that impair circulation.  35
- 36. D. GLAUCOMA IN CHILDREN It's possible for infants and children to have glaucoma. May be present from birth or develop in the first few years of life. The optic nerve damage may be caused by drainage, blockages or an underlying medical condition.  36
- 38. E. PIGMENTARY GLAUCOMA In pigmentary glaucoma, pigment granules from iris build up in the drainage channels, slowing or blocking fluid exiting eye. Activities such as jogging sometimes stir up the pigment granules, depositing them on the trabecular meshwork and causing intermittent pressure elevations.  38
- 40. PATHOPHYSIOLOGY There are two accepted theories regarding how increased IOP damages the optic nerve in glaucoma. The direct mechanical theory suggests that high IOP damages the retinal layer as it passes through the optic nerve head.
- 41. PATHOPHYSIOLOGY The indirect ischemic theory suggests that high IOP compresses the microcirculation in the optic nerve head, resulting in cell injury and death. Some glaucomas appear as exclusively mechanical, and some are exclusively ischemic types. Typically, most cases are a combination of both.  41
- 42. PATHOPHYSIOLOGY Regardless of the cause of damage, glaucomatous changes typically evolve through clearly discernible stages: Initiating events: precipitating factors include illness, emotional stress, congenital narrow angles, long-term use of corticosteroids, and mydriatics (ie, medications causing pupillary dilation). These events lead to the second stage.  42
- 43. PATHOPHYSIOLOGY Structural alterations in the aqueous out fl ow system: tissue and cellular changes caused by factors that a ff ect aqueous humor dynamics lead to structural alterations and to the third stage. Functional alterations: conditions such as increased IOP or impaired blood fl ow create functional changes that lead to the fourth stage.  43
- 44. PATHOPHYSIOLOGY Optic nerve damage: atrophy of the optic nerve is characterized by loss of nerve fi bers and blood supply, and this fourth stage inevitably progresses to the fi fth stage. Visual loss: progressive loss of vision is characterized by visual fi eld defects.  44
- 45. Eye pain Vision loss Nausea and vomiting Blurred vision Halos around lights Rainbow blurred halos around lights Eye redness CLINICAL MANIFESTATIONS  45
- 46. Open-angle glaucoma: Patchy blind spots in side (peripheral) or central vision Frequently in both eyes Tunnel vision in the advanced stages CLINICAL MANIFESTATIONS  46
- 47. Severe headache A loss of central or peripheral vision Blindness or changes in vision Chronic eye pain COMPLICATIONS  47
- 48. DIAGNOSTIC TESTS Medical history comprehensive Eye examination. Measuring intraocular pressure (tonometry) Optic nerve damage with a dilated eye examination Imaging tests Vision loss (visual field test) Corneal thickness (pachymetry)  48
- 49. DIAGNOSTIC TESTS Inspecting the drainage angle (gonioscopy) An ophthalmoscopic examination shows atrophy (pale color) and cupping (indentation) of the optic nerve head. The visual field examination is used to determine the extent of peripheral vision loss. chronic open-angle glaucoma, a small crescent-shaped scotoma (blind spot) appears early in the disease.  49
- 50. DIAGNOSTIC TESTS In acute angle closure glaucoma, the fields demonstrate larger areas of significant loss of vision. In clients with angle-closure glaucoma, a slit-lamp examination may demonstrate an erythematous conjunctiva and corneal cloudiness. The aqueous humor in the anterior chamber may also appear turbid (hazy), and the pupil may be nonreactive.  50
- 51. DIAGNOSTIC TESTS Increased IOP (>23 mmn Hg) indicates the need for further evaluation. Gonioscopy is performed to determine the depth of the anterior chamber angle and to examine the entire circumference of the angle for any abnormal changes in the filtering meshwork.  51
- 52. PREVENTION OF GLAUCOMA •≈ Get regular dilated eye examinations. American Academy of Ophthalmology recommends having a comprehensive eye exam every five to 10 years if you're under 40 years old; every two to four years if you're 40 to 54 years old; every one to three years if you're 55 to 64 years old; and every one to two years, the if you're older than 65.  52
- 53. PREVENTION OF GLAUCOMA •≈ Know your family's eye health history. Glaucoma tends to run in families. If you're at increased risk, you may need more frequent screening. Exercise safely. Regular, moderate exercise may help prevent glaucoma by reducing eye pressure. Talk with your doctor about an appropriate exercise program.  53
- 54. PREVENTION OF GLAUCOMA •≈ Take prescribed eyedrops regularly. Glaucoma eyedrops can significantly reduce the risk that high eye pressure will progress to glaucoma. To be effective, eyedrops prescribed by your doctor need to be used regularly even if you have no symptoms. Wear eye protection. Serious eye injuries can lead to glaucoma. Wear eye protection when using power tools or playing high-speed racket sports in enclosed courts.  54
- 55. MEDICAL MANAGEMENT •≈ Ocular pressure can be reduced by increasing fl ow of aqueous fl uids. In narrow angle glaucoma pupil is constricted using topical miotics or epinephrine, which opens the canal of Schlemm and promotes drainage of aqueous humor.  55
- 56. MEDICAL MANAGEMENT •≈ Prostaglandins. These increase the out fl ow of the fl uid in your eye (aqueous humor), thereby reducing your eye pressure. Medicines in this category include latanoprost (Xalatan), travoprost (Travatan Z), ta fl uprost (Zioptan), bimatoprost (Lumigan) and latanoprostene bunod (Vyzulta). Possible side e ff ects include mild reddening and stinging of the eyes, darkening of the iris, darkening of the pigment of the eyelashes or eyelid skin, and blurred vision. This class of drug is prescribed for once-a-day use.  56
- 57. MEDICAL MANAGEMENT •≈ Beta blockers. These reduce the production of fl uid in your eye, thereby lowering the pressure in your eye (intraocular pressure). Examples include timolol (Betimol, Istalol, Timoptic) and betaxolol (Betoptic). Possible side e ff ects include di ffi culty breathing, slowed heart rate, lower blood pressure, impotence and fatigue. This class of drug can be prescribed for once- or twice-daily use depending on your condition.  57
- 58. MEDICAL MANAGEMENT •≈ Alpha-adrenergic agonists. These reduce the production of aqueous humor and increase out fl ow of the fl uid in your eye. Examples include apraclonidine (Iopidine) and brimonidine (Alphagan P, Qoliana). Possible side e ff ects include an irregular heart rate, high blood pressure, fatigue, red, itchy or swollen eyes, and dry mouth. This class of drug is usually prescribed for twice-daily use but sometimes can be prescribed for use three times a day.  58
- 59. MEDICAL MANAGEMENT •≈ Carbonic anhydrase inhibitors. These medicines reduce the production of fl uid in your eye. Examples include dorzolamide (Trusopt) and brinzolamide (Azopt). Possible side e ff ects include a metallic taste, frequent urination, and tingling in the fi ngers and toes. This class of drug is usually prescribed for twice-daily use but sometimes can be prescribed for use three times a day.  59
- 60. MEDICAL MANAGEMENT •≈ Rho kinase inhibitor. This medicine lowers eye pressure by suppressing the rho kinase enzymes responsible for fl uid increase. It is available as netarsudil (Rhopressa) and is prescribed for once-a-day use. Possible side e ff ects include eye redness, eye discomfort and deposits forming on the cornea.  60
- 61. MEDICAL MANAGEMENT •≈ Miotic or cholinergic agents. These increase the out fl ow of fl uid from your eye. An example is pilocarpine (Isopto Carpine). Side e ff ects include headache, eye ache, smaller pupils, possible blurred or dim vision, and nearsightedness. This class of medicine is usually prescribed to be used up to four times a day. Because of potential side e ff ects and the need for frequent daily use, these medications are not prescribed very often anymore.  61
- 62. MEDICAL MANAGEMENT •≈ Because some of the eyedrop medicine is absorbed into your bloodstream, you may experience some side e ff ects unrelated to your eyes. To minimize this absorption, close your eyes for one to two minutes after putting the drops in. You may also press lightly at the corner of your eyes near your nose to close the tear duct for one or two minutes. Wipe o ff any unused drops from your eyelid.  62
- 63. MEDICAL MANAGEMENT •≈ If you have been prescribed multiple eyedrops or you need to use arti fi cial tears, space them out so that you are waiting at least fi ve minutes in between types of drops. Oral medications If eyedrops alone don't bring your eye pressure down to the desired level, your doctor may also prescribe an oral medication, usually a carbonic anhydrase inhibitor. Possible side e ff ects include frequent urination, tingling in the fi ngers and toes, depression, stomach upset, and kidney stones.  63
- 65. 1. LASER THERAPY. •≈ For open-angle glaucoma. laser burns are applied to the inner surface of the trabecular meshwork to open the intratrabecular spaces and widen the canal of Schlemm, thereby promoting out fl ow of aqueous humor and decreasing IOP. The procedure is indicated when IOP is inadequately controlled by medications it is contraindicated when the trabecular meshwork cannot be fully visualized because of narrow angles. A serious complication of this procedure is a transient rise in IOP (usually 2 hours after surgery) that may become persistent.  65
- 66. 2. LASER IRIDOTOMY •≈ for pupillary block glaucoma, an opening is made in the iris to eliminate the pupillary block. Laser iridotomy is contraindicated in patients with corneal edema, which interferes with laser targeting and strength. Potential complications are burns to the cornea, lens, or retina; transient elevated IOP; closure of the iridotomy; uveitis; and blurring. Pilocarpine is usually prescribed to prevent closure of the iridotomy.  66
- 67. 3. FILTERING •≈ Filtering procedures for chronic glaucoma are used to create an opening or fi stula in the trabecular meshwork to drain aqueous humor from the anterior chamber to the subconjunctival space into a bleb, thereby bypassing the usual drainage structures. This allows the aqueous humor to fl ow and exit by di ff erent routes (ie, absorption by the conjunctival vessels or mixing with tears).  67
- 68. 3. TRABECULECTOMY •≈ With a surgical procedure called a trabeculectomy, surgeon creates an opening in the white of the eye (sclera) and removes part of the trabecular meshwork. Complications include hemorrhage, an extremely low (hypotony) or elevated IOP, uveitis, cataracts, bleb failure, bleb leak, and endophthalmitis. Scarring is inhibited by using anti fi brosis agents such as the antimetabolites fl uorouracil (Efudex) and mitomycin (Mutamycin). Like all antineoplastic agents, they require special handling procedures before, during, and after the procedure. Fluorouracil can be administered intraoperatively and by subconjunctival injection during followup; mitomycin is much more potent and is administered only intraoperatively.  68
- 69. DRAINAGE TUBES •≈ Inserts a small tube shunt in your eye to drain away excess fl uid to lower the eye pressure. Drainage implants or shunts are open tubes implanted in the anterior chamber to shunt aqueous humor to an attached plate in the conjunctival space. A fi brous capsule develops around the episcleral plate and fi lters the aqueous humor, thereby regulating the out fl ow and controlling IOP.  69
- 70. MINIMALLY INVASIVE •≈ MIGS procedure to lower your eye pressure. These procedures generally require less immediate postoperative care and have less risk than trabeculectomy or installing a drainage device. They are often combined with cataract surgery. There are a number of MIGS techniques available, and your doctor will discuss which procedure may be right for you.  70
- 71. IRIDECTOMY HISTORY •≈ : Surgical removal of a portion of the iris facilitates drainage of aqueous humor through a newly created opening in the iris connecting to normal out fl ow channels. Note: Bilateral iridectomy is performed because glaucoma usually develops in the other eye.  71
- 72. NURSING MANAGEMENT •≈ Older clients with arthritic or shaking hands have difficulty instilling their own eyedrops. Instruct the client to lie down on a bed or sofa. Tilting the head back can to loss of balance. The eye drop regimen for glaucoma requires accurate timing. Older clients may need reminders, such as a check- off list and may a to use a timer or an alarm clock to help them remember.  72
- 73. •≈ Following surgery, the eye is covered with a patch and a metal or plastic shield for protection to protect from light and trauma. Instruct the client not to lie on the operative side to avoid pressure on the surgical site. When the effects of perioperative sedation have diminished, the client may ambulate and eat as desired. Frequent monitoring of 1OP is necessary because the surgical site is microscopic. Assess the client for continued or increasing pain, nausea, and decreased vision. Follow- up care is needed to monitor for delayed healing. The anterior chamber may fail to heal, or the wound may seal too tightly. Both situations warrant further surgery.  73 NURSING MANAGEMENT
- 74. NURSING MANAGEMENT •≈ Teach the client and family and provide written information on the following: Manifestations of infection (redness, swelling, drainage, blurred vision, pain) Manifestations of increased IOP (increasing pain, nausea, decrease in vision) The rationale for eye protection (shield or eyeglasses at all times) to protect from light and trauma Medications and eye drop instillation technique Scheduled return visit date and time Treatment of the surgical site: a. Carefully clean the area around the eye with warm tap water and a clean washcloth. Do not rub or apply pressure over the closed eye, which may damage healing tissue.  74
- 75. NURSING ASSESSMENT •≈ Demographic data of age and race because open-angle glaucoma occurs most often in clients more than 40 years of age and in blacks. Determine whether there is a family history f glaucoma or other eye problems and whether the client has had ocular surgery, infections, or trauma. imperative. An accurate list of current medications is because over-the- counter medications (such as antihistamines) may dilate the pupil, increasing the risk for angle-closure glaucoma. Always note a history of allergic reactions, particularly to medications or dyes. Ask the client to describe any changes in vision.  75
- 76. NURSING ASSESSMENT •≈ Although the manifestations of primary open-angle glau- coma are insidious, the client may describe blind spots in the periphery or an overall decreased visual acuity with loss of contrast sensitivity. Decreased, uncorrectable visual acuity usually Occurs when there has been irreversible damage to the optic nerve. If it has been previously established that the client has visual loss from glaucoma, assess how the client is coping with this loss. Although people adapt to the loss of vision in different ways, they usually manifest grief and loss at any stage of the disease process. Clients may be under standby anxious during examinations because they may fear discovery that further vision loss has occurred Assess the client's perception of glaucoma and the effect it has on quality of life. Help the client identify effective coping skills that may have been used in the past.  76
- 77. NURSING DIAGNOSIS AND INTERVENTIONS
- 78. 1. Disturbed Sensory Perception related to altered sensory reception: altered status of sense organ as evidenced by Progressive loss of visual fi eld. •≈ Nursing Interventions Determine type and degree of visual loss. Allow expression of feelings about loss and possibility of loss of vision. Implement measures to assist patient to manage visual limitations such as reducing clutter, arranging furniture out of travel path; turning head to view subjects; correcting for dim light and problems of night vision. Demonstrate administration of eye drops (counting drops, adhering to the schedule, not missing doses). Assist with administration of medications as indicated: Stress the importance of meticulous compliance with prescribed drug therapy: Provide sedation, analgesics as necessary.  78
- 79. 2. Anxiety related toPhysiological factors, change in health status; presence of pain; possibility/reality of loss of vision as evidenced by Apprehension, uncertainty. •≈ Nursing Interventions Evaluate anxiety level, degree of pain experienced or suddenness of onset of symptoms, and current knowledge of the condition. Give accurate, honest information. Discuss the probability that careful monitoring and treatment can prevent additional visual loss. Allow the patient to acknowledge concerns and express feelings. Identify helpful resources and people.  79
- 80. 3. De fi cient Knowledge related to Lack of recall, information misinterpretation evidenced by Questions; •≈ Nursing Interventions Stress the importance of glaucoma screening. Review pathology and prognosis of the condition and lifelong need for treatment. Discuss the necessity of wearing identification (MedicAlert bracelet). Demonstrate proper technique for administration of eye drops, gels, or discs. Have the patient perform a return demonstration. Review the importance of maintaining drug schedule like eye drops. Discuss medications that should be avoided such as mydriatic drops (atropine, propantheline bromide), overuse of topical steroids, and additive effects of [beta]-blocking when systemic [beta]-blocking agents are used. Identify potential side effects and adverse reactions of treatment such as decreased appetite, nausea, and vomiting, diarrhea, fatigue, “drugged” feeling, decreased libido, impotence, cardiac irregularities, syncope, heart failure (HF).  80
- 81. 3. De fi cient Knowledge related to Lack of recall, information misinterpretation evidenced by Questions; •≈ Encourage patient to make necessary changes in lifestyle. Reinforce avoidance of activities such as heavy lifting and pushing, snow shoveling, wearing tight or constricting clothing. Discuss dietary considerations (adequate fluid, bulk or fiber intake). Stress importance of routine checkups. Advise patient to immediately report severe eye pain, inflammation, increased photophobia, increased lacrimation, changes in the visual field, veil-like curtain, blurred vision, flashes of light and particles floating in the visual field. Recommend family members be examined regularly for signs of glaucoma Identify strategies and resources for socialization like support groups, Visually Impaired Society, local library, and transportation services.  81
- 82. 4. Risk for fall related to loss of vision •≈ Nursing Interventions Assess mood, coping abilities and personality styles Monitor vital signs and also the health condition of the patient Assist the client and provide information regarding present eye condition and risk that accompany it  82
- 83. 5.Pain related to spasm, intra-ocular pressure, glaucoma acute. As evidenced by protect the side of the pain patients, •≈ Intervention : Monitor blood pressure, pulse, and respiration every 4 hours. Monitor the degree of eye pain every 30 minutes during the acute phase. Monitor input and output every 8 hours while receiving intravenous osmotic agent. Monitor visual acuity at any time before hatching ophthalmic agents. Give appropriate instructions optalmic agent for glaucoma. Inform your doctor if : hypotension, urinary output of less than 40 ml / hour, No loss of pain in the eye within 30 minutes of drug therapy, Decrease in constant visual acuity. Prepare patients for surgery Maintain bed rest in semi-Fowler position. Prevent increase in IOP :Instruct to avoid coughing, sneezing, straining, or placing the head below the pelvic Provide quiet environment and avoid light. Give anlgetic prescription and evaluation of its e ff ectiveness.  83
- 84. 6. Grieving related to loss of vision as evidenced by signi fi cant loss of vision represents the need for compromise and adaptation for both the client and the client's family. •≈ Interventions. Assess the causative and contributing fac- tors that may delay the work of grieving and promote family cohesiveness. The social stigma of blindness underlies the anxiety that clients experience with actual or potential loss of vision. Total loss of vision isolates a person within a di ff erent reality. Although most clients are successfully rehabilitated, some losses are permanent. Also, some people, for a variety of reasons, remain socially isolated. The image of a blind person who is pit- ied and must accept the charity of others is disturbing. Use therapeutic communication to express empathy as the client relates expected and actual losses that are due to loss of vision. People with actual or potential loss of vision may be faced with barriers in their vocations that force an unwanted change. Not all jobs and work environments are adaptable for a person who is visually impaired. Age may be a major factor in the person's ability to meet this challenge. Self-esteem is closely related to the roles of people in their particular lifestyle. Loss of control in personal.  84
- 85. 7. Risk for Ine ff ective Therapeutic Regimen Management •≈ Interventions. The client may need to instill as many day. Constricting eyedrops are usually prescribed our times a day, and beta-blockers are usually prescribed every 12 hours; however, the eyedrops may be needed every 4 to 6 hours. The schedule is designed to provide the best possible control of IOP around the clock. Medications are an integral part of the treatment and care of a client with glaucoma, and nursing interventions must thus be directed at the client's ability to understand and comply with prescribed therapy. First, determine the client's current level of knowledge. Provide necessary information about glaucoma and its treatment in understandable terms. Diagrams may be helpful to the client and the client's signi fi cant others. Because treatment for glaucoma is often complex, involving both oral and topical ophthalmic medications, review a written plan of care in large print with the client and family. To maximize compliance, ensure that the plan of care fi ts into the client's lifestyle. The administration of eyedrops is a critical component of self-care for the client with glaucoma. After instructing the client and family on the technique of instillation, validate the client's or the family's ability to instill eyedrops properly by asking for a return demonstration. Be sure to include discussion of medications and their side e ff ects.  85
- 86. HEALTH EDUCATION •≈ Know your intraocular pressure (IOP) measurement and the desired range. Be informed about the extent of your vision loss and optic nerve damage. Keep a record of your eye pressure measurements and visual fi eld test results to monitor your own progress.  86
- 87. HEALTH EDUCATION •≈ Review all your medications (including over-the-counter and herbal medications) with your ophthalmologist, and mention any side e ff ects each time you visit. Ask about potential side e ff ects and drug interactions of your eye medications. Ask whether generic or less costly forms of your eye medications are available.  87
- 88. CATARACT
- 89. DEFINITION In cortical cataracts, spoke-like opacifications are found in the periphery of the lens. They progress slowly, infrequently involve the visual axis, and often do not cause severe loss of vision. Nuclear sclerotic cataracts are a result of a progressive yellowing and hardening of the central lens (nucleus). Most people older than 70 have some degree of nuclear sclerosis. directly on the visual axis.  89
- 90. RISK FACTORS INSPECTION. Ageing Loss of lens transparency Clumping or aggregation of lens protein (which leads to light scattering) Accumulation of a yellow brown pigment due to the break down of lens protein Decreased oxygen uptake Increase in sodium and calcium Decrease in levels of vitamin C, protein, and glutathione  90
- 91. The cumulative exposure to ultraviolet light over a person's life span is the single most important risk factor in cataract development. People who live at high altitudes or who work in bright sunlight, such as commercial fi shermen, appear to experience cataract formation earlier in life.  91 ETIOLOGY
- 92. Glassblowers and welders who do not wear eye protection are also at higher risk. Cataracts may develop as a result of many other systemic, ocular, and congenital disorders.  92 ETIOLOGY
- 93. Systemic disorders include diabetes, tetany, myotonic dystrophy, neurodermatitis, galactosemia, Lowe syndrome, Werner’s syndrome, and Down syndrome. Intraocular disorders include iridocyclitis, retinitis, retinal detachment, onchocerciasis, Infections (German measles, mumps, hepatitis, poliomyelitis, chickenpox, infectious mononucleosis) during the fi rst trimester of pregnancy may cause congenital cataracts.  93 ETIOLOGY
- 94. Blunt trauma, lacerations, foreign bodies, radiation, exposure to infrared light, and chronic use of corticosteroids may also result in cataracts.  94 ETIOLOGY
- 95. TYPES OF CATARACT 1.Cataracts a ff ecting the center of the lens (nuclear cataracts). A nuclear cataract may at fi rst cause more nearsightedness or even a temporary improvement in your reading vision. But with time, the lens gradually turns more densely yellow and further clouds your vision. As the cataract slowly progresses, the lens may even turn brown. Advanced yellowing or browning of the lens can lead to di ffi culty distinguishing between shades of color.  95
- 96. TYPES OF CATARACT 2.Cataracts that a ff ect the edges of the lens (cortical cataracts). A cortical cataract begins as whitish, wedge- shaped opacities or streaks on the outer edge of the lens cortex. As it slowly progresses, the streaks extend to the center and interfere with light passing through the center of the lens.  96
- 97. TYPES OF CATARACT 3.Cataracts that a ff ect the back of the lens (posterior sub capsular cataracts). A posterior sub capsular cataract starts as a small, opaque area that usually forms near the back of the lens, right in the path of light. A posterior sub capsular cataract often interferes with your reading vision, reduces your vision in bright light, and causes glare or halos around lights at night. These types of cataracts tend to progress faster than other types do.  97
- 98. TYPES OF CATARACT 4.Cataracts you're born with (congenital cataracts). Some people are born with cataracts or develop them during childhood. These cataracts may be genetic, or associated with an intrauterine infection or trauma. These cataracts may also be due to certain conditions, such as myotonic dystrophy, galactosemia, neuro fi bromatosis type 2 or rubella. Congenital cataracts don't always a ff ect vision, but if they do, they're usually removed soon after detection.  98
- 99. PATHOPHYSIOLOGY Cataract formation is characterised chemically by reduction in oxygen uptake and an initial increase water content followed by dehydration of the lens Sodium and calcium contents are increased; potassium, ascorbic acid, and protein contents are decreased. The protein in the lens undergoes numerous age related changes, including yellowing from formation of fl uorescent compounds and molecular changes.  99
- 100. PATHOPHYSIOLOGY These changes, along with the photo absorption of ultraviolet radiation throughout life, suggest that cataracts may be caused by a photochemical process. Cataracts progress in a predictable pattern. They begin as immature cataracts that are not completely opaque, and some light is transmitted through them, allowing useful vision.  100
- 101. PATHOPHYSIOLOGY The pieces of protein are engulfed by macrophages, which may obstruct the trabecular meshwork, causing phacolytic glaucoma.  101
- 102. PATHOPHYSIOLOGY Mature cataracts are completely opaque (the former term for this stage was ripe). Vision is signi fi cantly reduced. Hyper mature cataracts are those in which the lens proteins break down into short-chain polypeptides that leak out through the lens capsule. The pieces of protein are engulfed by macrophages, which may obstruct the trabecular meshwork, causing phacolytic glaucoma.  102
- 103. CLINICAL MANIFESTATIONS Clouded, blurred or dim vision Increasing di ffi culty with vision at night Sensitivity to light and glare Need for brighter light for reading and other activities Seeing "halos" around lights Frequent changes in eyeglass or contact lens prescription Fading or yellowing of colors Double vision in a single eye  103
- 104. DIAGNOSTIC TEST The Snellen visual acuity test, ophthalmoscopy, and slit lamp bio microscopic examination are used to establish the degree of cataract formation. The degree of lens opacity does not always correlate with the patient’s functional status. Some patients can perform normal activities despite clinically signi fi cant cataracts.  104
- 105. DIAGNOSTIC TEST Visual acuity test. A visual acuity test uses an eye chart to measure how well you can read a series of letters. Your eyes are tested one at a time, while the other eye is covered. Using a chart or a viewing device with progressively smaller letters, your eye doctor determines if you have 20/20 vision or if your vision shows signs of impairment.  105
- 106. DIAGNOSTIC TEST Slit-lamp examination. A slit lamp allows your eye doctor to see the structures at the front of your eye under magni fi cation. The microscope is called a slit lamp because it uses an intense line of light, a slit, to illuminate your cornea, iris, lens, and the space between your iris and cornea. The slit allows your doctor to view these structures in small sections, which makes it easier to detect any tiny abnormalities.  106
- 107. DIAGNOSTIC TEST Retinal exam. To prepare for a retinal exam, your eye doctor puts drops in your eyes to open your pupils wide (dilate). This makes it easier to examine the back of your eyes (retina). Using a slit lamp or a special device called an ophthalmoscope, your eye doctor can examine your lens for signs of a cataract.  107
- 108. DIAGNOSTIC TEST Applanation tonometry. This test measures fl uid pressure in your eye. There are multiple di ff erent devices available to do this.  108
- 109. PREVENTION Have regular eye examinations. Eye examinations can help detect cataracts and other eye problems at their earliest stages. Ask your doctor how often you should have an eye examination. Quit smoking. Ask your doctor for suggestions about how to stop smoking. Medications, counseling and other strategies are available to help you.  109
- 110. PREVENTION Manage other health problems. Follow your treatment plan if you have diabetes or other medical conditions that can increase your risk of cataracts. Choose a healthy diet that includes plenty of fruits and vegetables. Adding a variety of colourful fruits and vegetables to your diet ensures that you're getting many vitamins and nutrients. Fruits and vegetables have many antioxidants, which help maintain the health of your eyes.  110
- 111. PREVENTION Wear sunglasses. Ultraviolet light from the sun may contribute to the development of cataracts. Wear sunglasses that block ultraviolet B (UVB) rays when you're outdoors. Reduce alcohol use. Excessive alcohol use can increase the risk of cataracts.  111
- 112. No nonsurgical treatment cures cataracts. Ongoing studies are investigating ways to slow cataract progression, such as intake of antioxidants (eg, vitamin C, beta-carotene, vitamin E). In the early stages of cataract development, glasses, contact lenses, strong bifocals, or magnifying lenses may improve vision. Reducing glare with proper light and appropriate lighting can facilitate reading.  112 MEDICAL MANAGEMENT
- 113. Mydriatics can be used as short-term treatment to dilate the pupil and allow more light to reach the retina, although this increases glare. Adequate control of diabetes mellitus, Removal of cataractogenic drugs such as corticosteroids, phenothiazenes and strong miotics  113 MEDICAL MANAGEMENT
- 114. Removal of irradiation (infrared or X-rays) Early and adequate treatment of ocular diseases like uveitisCommercially available preparations containing iodide salts of calcium and potassium are being prescribed in abundance in early stages of cataract Vit E and aspirin also delays the process of cataractogenesis.  114 MEDICAL MANAGEMENT
- 115. Removal of irradiation (infrared or X-rays) Early and adequate treatment of ocular diseases like uveitisCommercially available preparations containing iodide salts of calcium and potassium are being prescribed in abundance in early stages of cataract Vit E and aspirin also delays the process of cataractogenesis.  115 MEDICAL MANAGEMENT
- 116. Commercially available preparations containing iodide salts of calcium and potassium are being prescribed abundance in early stages of cataract . Refraction should be corrected at frequent intervals  116 MEDICAL MANAGEMENT
- 117. Arrangement of illumination-patients with peripheral opacities brilliant illumination Use of dark goggles in patients with central opacities Mydriatics- 5%phenyephrine or 1% tropicamide b.i.d in a ff ected eye.  117 MEDICAL MANAGEMENT
- 118. Surgery is performed on an outpatient basis and usually takes less than 1 hour, with the patient being discharged in 30 minutes or less afterward. Although complications from cataract surgery are uncommon, they can have signi fi cant e ff ects on vision. Restoration of visual function through a safe and minimally invasive procedure is the surgical goal, which is achieved with advances in topical anesthesia, smaller wound incision (ie, clear cornea incision), and lens design (ie, foldable and more accurate intraocular lens measurements).  118 SURGICAL MANAGEMENT
- 119. Topical anesthesia, such as lidocaine gel applied to the surface of the eye, eliminates the hazards of regional anesthesia, such as ocular perforation, retrobulbar hemorrhage, optic injuries, diplopia, and ptosis, and is ideal for patients receiving anticoagulants. Moreover, patients can communicate and cooperate during surgery.  119 SURGICAL MANAGEMENT
- 120. Intracapsular Cataract Extraction. The entire lens (ie, nucleus, cortex, and capsule) is removed, and fi ne sutures close the incision. ICCE is infrequently performed today; however, it is indicated when there is a need to remove the entire lens, such as with a subluxated cataract (ie, partially or completely dislocated lens).  120 SURGICAL MANAGEMENT
- 121. Extracapsular Surgery. Extracapsularcataractextraction(ECCE) achieves the intactness of smaller incisional wounds (less trauma to the eye) and maintenance of the posterior capsule of the lens, reducing postoperative complications, particularly aphasic retinal detachment and cystoid macular edema. In ECCE, a portion of the anterior capsule is removed, allowing extraction of the lens nucleus and cortex. The posterior capsule and zonular support are left intact.  121 SURGICAL MANAGEMENT
- 122. Phacoemulsi fi cation. This method of extracapsular surgery uses an ultrasonic device that lique fi es the nucleus and cortex, which are then suctioned out through a tube. The posterior capsule is left intact. Because the incision is even smaller than the standard ECCE, the wound heals more rapidly, and there is early stabilization of refractive error and less astigmatism.  122 SURGICAL MANAGEMENT
- 123. Lens Replacement. After removal of the crystalline lens, the pa- tient is referred to as aphakic (ie, without lens). The lens, which focuses light on the retina, must be replaced for the patient to see clearly. There are three lens replacement options: aphakic eye- glasses, contact lenses, and IOL implants.  123 SURGICAL MANAGEMENT
- 124. Aphakic glasses are e ff ective but heavy. Objects are magni fi ed by 25%, making them appear closer than they actually are. Ob- jects are magni fi ed unequally, creating distortion. Peripheral vi- sion is also limited, and binocular vision (ie, ability of both eyes to focus on one object and fuse the two images into one) is im- possible if the other eye is phakic (normal).  124 SURGICAL MANAGEMENT
- 125. Contact lenses provide patients with almost normal vision, but because contact lenses need to be removed occasionally, the patient also needs a pair of aphakic glasses. Contact lenses are not advised for patients who have di ffi culty inserting, removing, and cleaning them. Frequent handling and improper disinfection increase the risk for infection  125 SURGICAL MANAGEMENT
- 126. Discomfort, bruising and swelling of the eyelid, increased intraocular pressure, and allergic reaction to the steroid or antibiotic drop. Progression to pain, decrease in vision, or any discharge from the eye, patients are advised to seek medical attention. Posterior Capsule Rupture/Vitreous loss  126 COMPLICATIONS
- 127. Due to the nature of cataract surgery, posterior capsule tears may occur at any point during the operation. The capsulotomy step of the surgery is the most crucial, not only to create an opening to access the nucleus of the lens, but also due to the associated high risks if improperly performed.  127 COMPLICATIONS
- 128. Loss of the vitreous due to capsular rupture can lead to severe visual disability and other complications previously mentioned such as retinal detachment. Cystoid Macular Edema CME is the most frequent complication after an uncomplicated  128 COMPLICATIONS
- 129. Optical coherence tomography (OCT) is the standard method for diagnosis and monitoring of CME, though fl uorescein angiography is considered the gold standard. With modern phacoemulsi fi cation techniques, CME occurs in about 1 to 2% of cataract surgery.  129 COMPLICATIONS
- 130. Fluid collection places mechanical stress on the Muller cells, which manifest as decreased central vision and scotoma in the patient.  130 COMPLICATIONS
- 131. Endophthalmitis Endophthalmitis is a serious complication of cataract surgery involving microorganisms that gain entry into the eye. Risk factors for the development of endophthalmitis include rupture of the posterior capsule or the need for anterior vitrectomy during the procedure, age greater than 85 years, and male sex.  131 COMPLICATIONS
- 132. Higher rates of endophthalmitis were found in patients undergoing intracapsular cataract extraction compared to extracapsular cataract extraction. Staphylococcus epidermidis is the most common infectious organism since it is native to the eyelid, skin, and conjunctiva and can seed the eye during the procedure. Vitreous/Suprachoroidal Hemorrhage  132 COMPLICATIONS
- 133. Hemorrhage is a sight-threatening complication that is often associated with incisional intraocular surgery. Risk factors determined for hemorrhage include myopia, glaucoma, diabetes, atherosclerotic vascular disease, and hypertension. Retinal Tears/Detachment Retinal detachment is considered a delayed complication of cataract surgery. Lens Dislocation  133 COMPLICATIONS
- 134. During the history and physical examination ask the client about any predisposing factors (trauma, Systemic diseases, medications such as corticosteroids and other ocular problems). Visual acuity (both distant and near) in each eye is documented. Ask the client to describe visual disturbances. The client's visual acuity may be relatively close to normal ranges, and yet the Client may experience di ffi culty in performing ADL. The client's individual perception of the quality of Vision 15 an important factor in determining the need for surgery.  134 NURSING ASSESSMENT
- 135. Nursing Interventions 1. Assess the degree and duration of visual impairment. Encourage conversation to fi nd out the patient's concerns, feelings, and the level of understanding. 2. Orient the patient to the new environment. 3. Explain the preoperative routines. 4. Describes intervention much detail as possible. 5. Push to perform daily living habits when able. 6. Encourage participation of family or the people who matter in patient care. 7. Encourage participation in social activities and diversion whenever possible (visitors, radio, audio recording, TV, crafts, games).  135 1.Anxiety related to lack of knowledge
- 136. Nursing Intervention 1. Help the patient when able to do until postoperative ambulation and achieve stable vision and adequate coping skills, using techniques of vision guidance. 2. Help the patient set the environment. 3. Orient the patient in the room. 4. Discuss the need for the use of metal shields or goggles when instructed 5. Do not put pressure on the a ff ected eye trauma. 6. Use proper procedures when providing eye drugs.  136 2.Risk for injury related to blurred vision
- 137. Nursing Interventions 1. Give medications to control pain and the IOP as prescribed. 2. Give cold compress on demand for blunt trauma. 3. Encourage use of sunglasses in strong light.  137 3.Acute pain related to trauma to the incision and increased IOP
- 138. Nursing Interventions 1. Maintain strict aseptic technique, do wash your hands frequently. 2. Supervise and report immediately any signs and symptoms of complications, such as: bleeding, increased IOP or infection. 3. Explain the recommended position. 4. Instruct the patient to know bedrest activity restrictions, with fl exibility to the bathroom, according to a gradual increase in activity tolerance. 5. Describe the actions that should be avoided, as prescribed by coughing, sneezing, vomiting (ask for medication for it). 6. Give medications as prescribed, according to prescribed techniques.  138 4.Risk for infection related to trauma to the incision
- 139. Nursing Interventions Assess the patient’s ability to see and perform activities. Provides a baseline for determination of changes a ff ecting the patient’s visual acuity.Encourage patient to see an ophthalmologist at least yearly. Can monitor progressive visual loss or complications. Decreases in visual acuity can increase confusion in the elderly patient. Provide su ffi cient lighting for the patient to carry out activities. Elderly patients need twice as much light as younger people.  139 5. Disturbed Sensory Perception related to CataractsPoor visual acuity Changes in the eyes due to evidenced by
- 140. After cataract surgery, clients are expected to return for a follow-up visit the next morning and again at 1 week and at one month. Care includes observation of the ocular dressing, if present, and assessment of the client's ability to perform ADL at the preoperative level.  140 HEALTH EDUCATION
- 141. Eye pain, if present, should be reported immediately. The eye patch is usually removed the next morning but may be removed after a few hours if the client has limited vision in the other eye.  141 HEALTH EDUCATION
- 142. Instruct the client to wear a plastic shield to protect the eye from accidental injury and not to rub the eye. Glasses may be worn during the day. Should avoid heavy lifting (>15 pounds) or straining in the early postoperative period.  142 HEALTH EDUCATION
- 143. Eye care for the client after cataract surgery is the same as that for glaucoma clients. Postoperative eye medications may include antibiotics, corticosteroids, or both.  143 HEALTH EDUCATION
- 144. Assess the client's or the family's ability to instill eyedrops appropriately. Review the rationale and schedule for the medications with the client and family. Postoperative discomfort should be minimal to moderate and is usually relieved by acetaminophen.  144 HEALTH EDUCATION
- 145. ASSESSMENT OF ORAL Clients commonly experience an itching sensation after cataract surgery. Instruct the client to report any pain that is unrelieved.  145 HEALTH EDUCATION
- 146. ASSESSMENT OF ORAL Review the clinical manifestations of infection and increased IOP with the client and family. Depending on the client's age, ability, and availability of assistance, make a referral for home health care as indicated.  146 HEALTH EDUCATION
- 148. Life Experiences of Patients With Glaucoma: A Phenomenological Study Abstract Background: Studies that describe the experiences of patients with glaucoma from di ff erent cultures may help health professionals gain a broader perspective on this issue. Currently, few qualitative studies describe how patients with glaucoma in Turkey cope with daily life. Purpose: The aim of this study was to explore the experiences of patients with glaucoma. Method: This descriptive phenomenological study used purposive sampling to enroll 20 patients with glaucoma. A qualitative, in-depth, face-to- face interview technique was used to collect data during January and February 2014. The data were analyzed using to the Van Kaam method. Results: Seven themes were identi fi ed, including con fi rming the diagnosis by acute symptoms or unrelated symptoms, grateful to God for having a non-life-threatening disease, feeling happy after receiving more accurate information, coping with the disease by using eye drops and attending follow-up examinations regularly, managing daily life to avoid further damage to eyesight, emotional reactions related to going blind, and urging family members or friends to attend regular glaucoma checkups. Conclusions: Patients with glaucoma experience physiological and psychological problems throughout the course of their disease. Being informed and cultural practices such as “praising God” and “resignation” helped patients cope with the disease. Furthermore, because of the cultural characteristic of social collectivism, participants acted to protect the health of others by informing them about glaucoma. Implications for Practice: Understanding the experiences of patients with glaucoma is important for nursing practice. Nurses should be encouraged to take a greater role in the care of patients with glaucoma by becoming the primary source of glaucoma disease, treatment, and care-related informatio  RESEARCH
- 149. BIBLIOGRAPHY Brunner & suddarth’s, Medical-Surgical nursing,(2015) 10th edition, Page 1748-61 Joyce.M.Black, Medical-Surgical nursing,(2020) 6th edition, page 1709-16 Williams.S. Linda,Understanding Medical Surgical Nursing, 3rd edition(2007) Taylor Carol, Fundamentals of nursing(2010), 5th edition Chintamani, Lewis Medical-surgical nursing,( 2011), 2nd edition,CBS Publications Priscilla Lemonne, Medical Surgical Nursing, 2nd edition https://nurseslabs.com/2-cataracts-nursing-care-plans/2/ https://www.scribd.com/doc/298494653/Nursing-Care-Plan-for-Glaucoma https://eyewiki.aao.org/Cataract_Surgery_Complications