seminar non invasive respiratory support
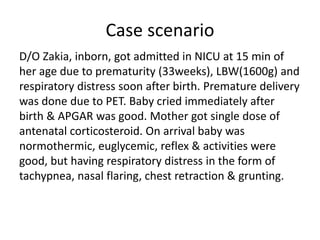
- 1. Case scenario D/O Zakia, inborn, got admitted in NICU at 15 min of her age due to prematurity (33weeks), LBW(1600g) and respiratory distress soon after birth. Premature delivery was done due to PET. Baby cried immediately after birth & APGAR was good. Mother got single dose of antenatal corticosteroid. On arrival baby was normothermic, euglycemic, reflex & activities were good, but having respiratory distress in the form of tachypnea, nasal flaring, chest retraction & grunting.
- 2. Question - 1 Which support will you provide first to the baby?
- 3. Question - 2 How will you select appropriate respiratory support for this baby?
- 4. Non Invasive Respiratory Support in newborn Dr. Lubana Akram Resident, Year – 1 Dr. Arif Hossain Resident, Year – 5
- 5. Content • Definition of respiratory distress • Respiratory distress scoring system • Delivery room management of respiratory distress • Different modalities of respiratory support • Supplemental O2 delivery apparatus • Different types of non invasive respiratory support • O2 toxicities • O2 monitoring device
- 6. Suzanne Reuter et al. Respiratory Distress in the Newborn. Pediatrics in Review. 2014;35(10):417 - 29 Respiratory distress in the newborn is defined as one or more signs of increased work of breathing, such as - tachypnea, - nasal flaring, - chest retractions or - grunting.
- 7. Assessment of respiratory distress • The WHO provides the most simplified scoring system.
- 9. Downes’ scoring system 0 1 2 Cyanosis none In room air In 40% Fio2 Retractions none Mild Severe Grunting none Audible with stethoscope Audible without stethoscope Air entry Clear Decreased or delayed Barely audible Respiratory rate <60 60-80 >80 or apnea
- 10. • Term newborn infant reach stable arterial oxygen saturation values around 85% to 90% by arterial oxygen saturation within 5 minutes. • Preterm infants, especially extremely preterm infants need almost 10 minutes to reach preductal Sp02 of around 85%. Delivery room management
- 11. Recommendation for pre term • In spontaneously breathing babies stabilise with CPAP of at least 6 cm H2O • Intubation should be reserved for babies not responding to positive pressure ventilation. • Surfactant who require intubation for stabilisation. Respiratory support in Delivery room
- 12. • T – piece resuscitator for resuscitation in delivery room. • Use an initial FiO2 of - 0.30 for < 28 weeks of gestation - 0.21–0.30 for 28–31 weeks - 0.21 for 32 weeks of gestation and above. (European Consensus Guidelines on the Management of Respiratory Distress Syndrome – 2019 ) Respiratory support in Delivery room
- 13. Rescue or therapeutic surfactant: Preterm who are - o Suspected of having surfactant deficiency o Required endotracheal intubation & MV o Required an FiO2 > 0.40 o Clinical and radiographic evidence of neonatal RDS AARC Clinical Practice Guideline. Surfactant Replacement Therapy: 2013
- 14. • Using CPAP immediately after birth with subsequent selective surfactant administration considered as an alternative to routine intubation with prophylactic or early surfactant administration in preterm infants. Respiratory support in Delivery room
- 15. CHIRUVOLU et al. Delivery room management of meconium- stained newborns and respiratory support. PEDIATRICS. 2018; 142(6): 1 – 7 • The recent NRP guideline change in the delivery room management of newborns who are nonvigorous and born through MSAF avoided a large number of intubations in the delivery room and was not associated with an increased incidence of MAS. • This change was associated with a higher incidence of NICU respiratory admissions and increased needs for mechanical ventilation, oxygen, and surfactant therapy.
- 16. Respiratory Therapeutic Modalities • Supplemental Oxygen • Noninvasive ventilation CPAP, HFNC NIPPV • Invasive modalities MV
- 17. Nasal prongs • Nasal prongs are a disposable plastic device that ends in two short tapered tubes (about 1 cm in length) designed to lie just within the nostrils. They are also called nasal cannula. • Standard flow rates through nasal prongs are 0.5–1 L/min for neonates
- 18. Nasal prongs Advantages • No risk of gastric distension • Humidification is not required with standard oxygen flow rates
- 19. Disadvantages • Airway will become obstructed by mucus • Unable to use with nasal obstruction • Can dislodge from nares easily • Causes skin irritation or breakdown over ears or at nares Nasal prongs
- 20. Nasal catheter • A nasal catheter is a thin, flexible tube that is passed into the nose and ends with its tip in the nasal cavity. • In neonates and infants, 8-French (F) size catheters should be used. • The maximum flow rate should be set at 0.5–1 L/min for neonates and 1–2 L/min for infant.
- 21. • Catheter passed for a distance equal to the distance from the side of the nostril to the inner margin of the eyebrow usually reaches the posterior part of the nasal cavity. • The tip of the catheter should not be visible below the uvula.
- 22. Advantage: The oxygen does not have to be humidified because the tip of the catheter lies in the nasal cavity. Disadvantage: Catheters can become blocked with mucus, which can cause upper airway obstruction There is little risk of displacement into the oesophagus, with a consequent risk of gastric distension Nasal catheter
- 23. Nasopharyngeal catheters • Nasopharyngeal catheters are inserted into the nose to a depth 1 cm less than the distance from the side of the nose to the front of the ear (tragus). • In neonates and infants, 8-F catheters should be used. • Maximum flow rate 0.5 L/min for neonates
- 25. Nasopharyngeal catheters Disadvantage • Higher flow rates without effective humidification may cause drying of the nasal mucosa, with associated bleeding and airway obstruction. • Can be displaced downwards into the oesophagus and cause gagging, vomiting and gastric distension. Advantages: • Oxygen delivery is most economical of all the methods described here. • Better oxygenation is achieved with a lower oxygen flow than with nasal prongs
- 26. • An oxygen hood (cube) is a plastic enclosure that surrounds the head of the neonate, to which a continuous flow of humidified oxygen is supplied • Gas flow rate 3 – 10 L/min. Head box
- 27. Head box Advantages No increased risk for airway obstruction or gastric distension Humidification is not necessary. Disadvantage Carbon dioxide toxicity can occur if the flow of oxygen is inadequate. A gas flow of 2–3 L/kg per min is necessary to avoid rebreathing of carbon dioxide in a head box . • Head boxes interfere with feeding.
- 28. Face mask • Simple mask is made of clear, flexible,plastic or rubber that can be molded to fit the face • Not use in neonates
- 29. Supplemental Oxygen via the Incubator Is the most common method of low-level supplemental O2 delivery in Europe These incubators have respiratory gas connection ports, a microprocessor, and an oxygen sensor that control O2 content
- 30. Advantages: • Servo controlled incubators provides steady oxygen • Avoid the skin breakdown • Noise is low Disadvantages: Infant must be maintained in an incubator Supplemental Oxygen via the Incubator
- 31. O2 Administration By Holding O2 Source Near The Infant’s Face This kind of oxygen administration is widely used for short periods- - after extubation - during breast feeding who is on headbox O2
- 32. Oxygen Delivery Devices and Flow Limit • Nasal prongs : 1-2L /min • Nasal cannula: 1-2 L/min • Nasal catheter : 1-2L /min • Nasopharyngeal catheter : 1-2L /min • Head Box : 3-10L /min • CPAP : 3-10 L /min • HFNC: 3 – 8 L/min • Ventilator : As much as
- 33. Non invasive respiratory support(NIRS) NIRS Typical Non Typical eg. HHHFNC CPAP NIMV/NIPPV NHFV NIV-NAVA
- 34. Choice of respiratory support • CPAP should be initiated at the earliest or subtle signs of respiratory distress in neonates at risk for RDS. • Some arbitrary criteria can be Silverman score of ≥ 4 or FiO2 requirement ≥ 0.3. • For preterm baby especially in extremely low birth weight baby as tachypnea is the earliest sign of respiratory distress. Tachypnea = CPAP
- 35. A. B. Hedstrom et al. Performance of the Silverman Andersen Respiratory Severity Score in predicting PCO2 and respiratory support in newborns. Journal of Perinatology. February 2018.
- 36. Continuous Positive Airway Pressure (CPAP) Types: 1) Continuous Flow CPAP - Ventilator derived CPAP - Bubble CPAP 2) Variable Flow CPAP - Infant Flow Driver - Sigh Intermittent Positive Airway Pressure (SiPAP)
- 38. Most widely used CPAP is Bubble CPAP Indications: Presence of good respiratory drive is pre requisite of CPAP support. - Respiratory disorder (RDS, MAS, Pneumonia, PPHN) - Apnea of prematurity - Disorder causing excessive lung fluid (TTN, PDA, CCF, Hydrops fetalis ect.) - Laryngo/tracheo/broncho malacia - After extubation
- 39. Contraindications of CPAP • Poor respiratory drive that is not improved by CPAP • Cleft palate • Choanal atresia • Tracheoesophageal fistula • Unrepaired CDH • Severe cardiovascular instability (Hypotension) • Severe apneic episode • Severe ventilatory impairment (PH < 7.25, PCO2>60)
- 40. How CPAP work? • Increase FRC • Improve lung compliance • Aid in the stabilization of highly complaint infant chest wall • Decrease thoracoabdominal asynchrony • Decrease intrapulmonary shunting • Reduce tachypnea • Decrease labored breathing
- 41. Time of application of CPAP • Prophylactic CPAP in delivery room • Early : within 2 hours of distress • Late : after FiO2 requirement > 0.40 CPAP does not work as expected if it is started after atelectasis have been already occurred. Early CPAP is beneficial. It enhance - surfactant conservation - lower PEEP - reduce the need for MV
- 42. Devices used for interface • Nasal prong • Nasopharyngeal prong • Nasal mask • Face mask Widely used nasal prong. No published data concerning the safety and efficacy of nasal mask.
- 43. Bipin.Is nasal mask better than nasal prongs for delivering nasal continuous positive airway pressure in preterm infants with respiratory distress syndrome? 2018 CONCLUSION Nasal Continuous positive airway pressure (NCPAP) with mask interface is equally effective as nasal continuous positive airway pressure (NCPAP) with prongs interface. Incidence of stage II nasal trauma was significantly lower in mask group than in the prongs group.
- 44. Setting of PEEP, FiO2 & Flow • Set up is disease specific. • Pressure ranges 4 – 7 cmH2O • FiO2 0.21 – 0.60 • Flow rate 2 – 8 L/min General rules of initial setup is rules of “5”. - Pressure: 5 cmH2O - FiO2: 0.50 - Flow: 5 L/min Always insert orogastric tube while baby on CPAP and keep open & above the level of stomach
- 45. How to assess optimum CPAP • Baby is comfortable in CPAP • Minimal or no retraction • No grunt • Normal CRT & BP • Maintain SpO2 within 90 – 95% • CXR: Presence of 8 posterior ICS above diaphragm. • Achieve expected blood gas level in high set up (PH > 7.25, PCO2 < 60 & PO2 > 50)
- 46. Adjustment of PEEP, FiO2 & Flow • ↑ PEEP by 1 cmH20 in every 15 to 20 min to maintain SpO2 between 90 – 95% • Adjust PEEP by seeing the chest retraction. Increase PEEP upto 8 cmH2O • Do not raise FiO2 before pressure. • ↑ FiO2 upto 0.60 to maintain SpO2 • No bubbling inadequate flow to generate pressure or may be leak in circuit. • Excess bubbling wastage of gases or turbulence in flow.
- 47. CPAP & FiO2 proportionality CPAP 4 FiO2 25 – 40% CPAP 5 FiO2 50% CPAP 6 FiO2 60% CPAP 7 FiO2 70% If there is any discrepancy between CPAP and pressure & FiO2 think about - PPHN - CHD - Metabolic acidosis - Over distended lungs
- 48. Weaning of CPAP • The process of weaning should be slow and steady. • Every 1 cmH2O decrease in CPAP aims to decrease FiO2 10%. • When baby comes down to PEEP 5 & FiO2 50% then first decrease FiO2 upto 30% and then decrease pressure from 5 to 4 cmH2O. • When pressure 4 and FiO2 < 30% with normal SpO2 and minimal retraction, CPAP may be weaned to air or head hood.
- 49. CPAP Failure • Presence of retraction/grunt despite giving optimum CPAP • Recurrent or severe apnea (significant apnea means 3 apnea/ hour or that requiring bag & mask ventilation) • Significant bradycardia • PO2 < 50 in FiO2 >0.60 • PCO2 > 60 or PH < 7.25 Most common cause for CPAP failure is delayed in initiation after birth.
- 50. Complications of CPAP • Pulmonary air leak syndrome • Decreased cardiac out put due to reduction in venous return • Impedance of pulmonary blood flow with increased pulmonary vascular resistance • Gastric distension & CPAP belly syndrome • Nasal irritation, damage to the septal mucosa, skin damage and necrosis from fixing devices.
- 51. Other CPAP devices Infant Flow Driver: This device generate CPAP at the airway proximal to infants nose. Principles: - Bernoullis effect (maintain constant pressure) - Venturi effect (flow variation acc. to baby needs) - Coanda effect (causes fluidic flip & hence ↓ WOB)
- 52. Sigh Intermittent Positive Airway Pressure (SiPAP) • It is newer mode of NIV which provides bilevel CPAP • SiPAP is not a nasal IMV • Small (2-3 cmH2O), slow, intermittent increase in CPAP pressure for duration up to 3 sec →sigh breath. • SiPAP setting: - Baseline CPAP level - Frequency (usually 6) - Pressure rise (2-3 cm H2O) - Duration of pressure rise (1-2 sec)
- 53. Advantages of different types of NCPAP • Bubble CPAP → continuous bubbling & pressure oscillates in the circuit → facilitates gas exchange by facilitated diffusion. • Sea-PAP → more oscillation by bending at an angle of 135 degree in expiratory tube. • IFD → more uniform pressure. • SiPAP → more alveoli recruitment, stimulate resp center. There are no definite data to support or refute using one NCPAP system to another.
- 54. Trouble Shoot in CPAP SpO2 Retraction Air entry Bubbling Diagnosis Low +++ Poor Yes Lung disease Low +/nil Good Yes PPHN/CHD Normal +++ Good Yes Metabolic acidosis Low +++ Poor Yes Obstruction Low +++ Poor Nil Leaks
- 55. Colin et al. Nasal CPAP or Intubation at Birth for Very Preterm Infants. n engl j med.2008; 358(7). COIN trial Conclusion: Infants who were born at 25-28 weeks’ gestation and were breathing spontaneously were treated with CPAP shortly after birth. Half were subsequently intubated. Infants in the CPAP group had a better outcome at 28 days. Two groups had a similar outcome at 36 weeks’ gestational age, but there was an increased incidence of pneumothorax in the CPAP group.
- 56. Early CPAP versus Surfactant in Extremely Preterm Infants. n engl j med. 2010; 362(21). SUPPORT trial Conclusion: No significant difference in the primary outcome of death or bronchopulmonary dysplasia between two groups. CPAP results lower rate of intubation, reduced rate of postnatal corticosteroid use, shorter duration of ventilation without an increased risk of any adverse neonatal outcome. Data supports CPAP as an alternative to routine intubation and surfactant administration in preterm infants.
- 57. SANDRI et a. Prophylactic or Early Selective Surfactant Combined With nCPAP in Very Preterm Infants. PEDIATRICS.2010;125(6). CURPAP trial. CONCLUSIONS: • Prophylactic surfactant was not superior to nCPAP. • Early selective surfactant decreases the need for MV in the first 5 days of life and the incidence of main morbidities of prematurity in spontaneously breathing very preterm infants on nCPAP.
- 58. DUNN et a. Randomized Trial Comparing 3 Approaches to the Initial Respiratory Management of Preterm Neonates. PEDIATRICS. 2011;128(5). VON DRM trail CONCLUSIONS: Preterm neonates were initially managed with either nCPAP or PS with rapid extubation to nCPAP had similar clinical outcomes to those treated with PS followed by a period of mechanical ventilation. An approach that uses early nCPAP leads to a reduction in the number of infants who are intubated and given surfactant.
- 60. Humidified High Flow Nasal Cannula(HHFNC) • Same as CPAP but without having in- build PEEP. • Here PEEP is created by high flow (3-8 L/mi) which is dynamic pressure.
- 61. HHFNC cont… Mechanism by which it works: Flushing the upper airway dead space of CO2, allowing for better alveolar gas exchange. Providing a flow adequate to support inspiration, thereby reducing inspiratory WOB. Improving lung & airway mechanics by eliminating the effect of drying/cooling. Reducing or eliminating the metabolic cost of gas conditioning. Provide end distending pressure.
- 62. Indications of HHFNC • In post extubation setting • Weaning from nCPAP • As primary mode of support in respiratory distress though enough evidence for safety and efficacy lacking.
- 63. Protocol for initiating set up of HHFNC • First appropriate size nasal cannula is attached to circuit tube. • Set FiO2 at same or 5-10% higher from previous mode of support in post extubation cases. Start with FiO2 0.40 in case of primary support. • A rule of thumb for initial flow rate setting, use 1-2-3, 2-3-4, 3-4-5 formula 1 to 2 kg = 3 L/min 2 to 3 kg = 4 L/min > 3 kg = 5 L/min
- 64. Maintain & weaning of HHFNC • ↑flow rate 1 L/min if FiO2 increases > 10% and PCO2 increases > 10 mmHg above baseline. • Titrate flow & FiO2 to keep SpO2 between 90-95%. • First decrease FiO2 during weaning upto 40% then decrease flow rate slowly by 1 L/min upto 3L/min. • Then further decrease FiO2. • Then wean to air or headhood.
- 65. Non Invasive Ventilation (NIV) NIV or NIPPV is used for patient failing NCPAP or following extubation from MV. Synchronized & nonsynchronized NIMV with a conventional ventilation is the most common form. NIV avoid complications of prolonged invasive ventilator (volutrauma, infection & subglottic stenosis.) One study showed that NPSIMV may be less injurious to lungs & provide better ventilation with less need for support than invasive SIMV.
- 66. NIPPV cont… • Short binasal prongs are the most commonly used interface for NIPPV. • Nasal mask & nasopharyngeal prongs can be used. • Set up: Short inflation times (0.3–0.5 s), Variable inflation rates of 10–60/min and Peak pressures and positive end expiratory pressure similar to those used with endotracheal ventilation.
- 67. Neurally Adjusted Ventilatory Assist (NAVA) • NAVA is new & unique form of assisted ventilation. • It can be used in both intubated & non intubated patients. • It controls the ventilator by using the electrical activity of the diaphragm (EAdi). • EAdi signal is obtained by nine miniaturized electrodes embedded on a conventional naso/oro gastric tube, positioned in the lower esophagus.
- 69. NAVA cont… • EAdi signal will not be present during apnea, oversedation or severe brain injury. • NIV-NAVA is possible only when the infant has a reasonably stable respiratory drive. • A RCT of 15 infants of <32 weeks compared NIV- NAVA with NIV-Pressure Support and found better patient ventilator synchrony with NAVA.
- 70. Nasal High Frequency Ventilation (NHFV) • NHFV breath can be delivered by nasopharyngeal or nasal prongs. • NHFV with Drager VN500 ventilator showed nearly threefold more efficient CO2 clearance than NIMV. • Potential advantage of NHFV over NIMV is that synchronization is not necessary, because of relatively high frequencies.
- 71. HFNC CPAP NIPPV Answer is Which non invasive modality is the best? ?
- 73. The aim : was to assess the clinical effectiveness and safety of HFNC compared to CPAP as a noninvasive respiratory support for the initial respiratory management of respiratory distress in preterm infants. Conclusion : There is no evidence to support the non inferiority of HFNC compared to CPAP as an initial management of respiratory distress in premature infants at between 30 and 35 weeks gestational age. The difference in failure rate is not significant without an increase in the incidence of complications. HFNC Vs CPAP cont…
- 74. Sarah et al.Safety and Efficacy of High-Flow Nasal Cannula Therapy in Preterm Infants: A Meta-analysis.PEDIATRICS Volume 136, number 3, September 2015 RESULTS: High-flow therapy was similar in efficacy to other modes of NIV in preterm infants when used as primary support (odds ratio of failure of therapy, 1.02) as well as after extubation (1.09). There were no significant differences in odds of death (0.48) between the groups. Preterm infants supported on high flow had significantly lower odds of nasal trauma (0.13)
- 79. HFNC CPAP More trials is required to find out optimum non invasive ventilation NIPPV Answer is Which non invasive modality is the best?
- 80. Oxygen is Life Saving, but…. • Oxygen is the energy source of cellular life. • It is the biomedical double –edged sword. • It is mandatory to avoid hypoxia, but prolonged hyperoxia leads to oxidative stress and cellular injury.
- 81. Complications of Oxygen Therapy • Skin irritation • Drying of nasal and pharyngeal mucosa • Induced hypoventilation • Absorption atelectasis • Adverse effect on retina • Adverse effect on lung eg CLD
- 82. Noninvasive monitoring of Gas Exchange? Pulse oximetry: by which SpO2 is measured. Transcutaneous oxygen monitoring (TcPO2) Capnography & End – Tidal CO2 monitoring - Mainstream capnography - Sidestream devices Transcutaneous CO2 monitoring Tissue oxygen saturation monitoring using Near Infrared Spectroscopy (NIRS)
- 83. Target Range of Saturation spo2 • Preterm : 88-92% • The optimal SpO 2 target of ELBW infants is not known • Term : 93-97%
- 84. Take home message • Stabilization in the delivery room should be done with 30% O2 in gestation ≤ 32 weeks. • CPAP immediately after birth with subsequent selective surfactant administration is an alternative to routine intubation with prophylactic or early surfactant administration in preterm. • Noninvasive ventilator (NIV) support is preferred in comparison to invasive supports.
- 85. References • Rennie & Roberton’s textbook of neonatolog. 5th edition • Neonatolog. management, procedure, no-call problems, and drugs. 7th editiom • Manual of neonatal care. 8th edition • Avery’s diseases of the newborn. 7th edition • Nelson textbook of pediatrics. 20th edition • Assisted ventilation of the neonate. 5th edition • CPAP bedside application in the newborn. 2nd edition • Workshop on CPAP. Science, evidence & practice. 4th edition • Online journal
