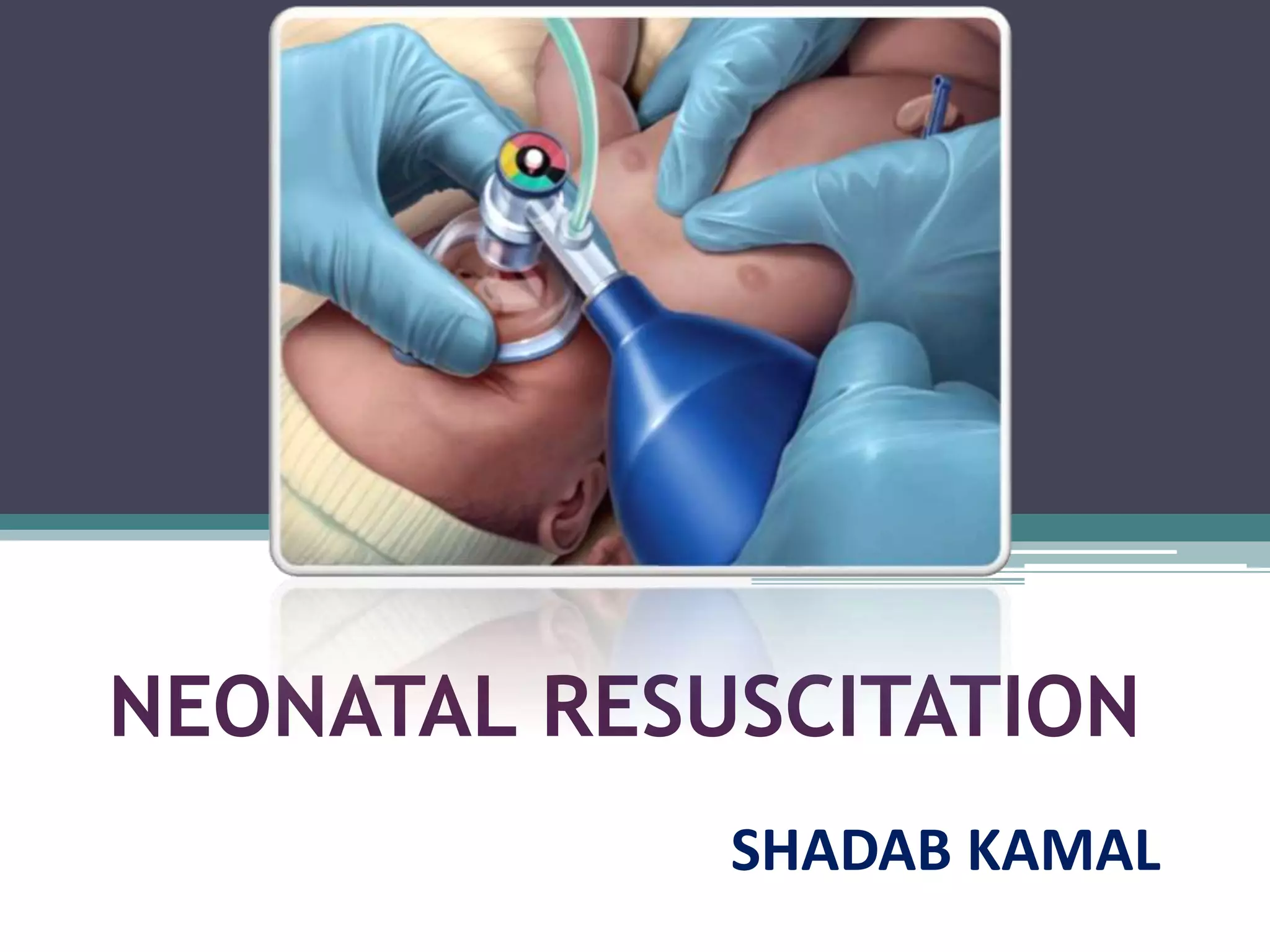
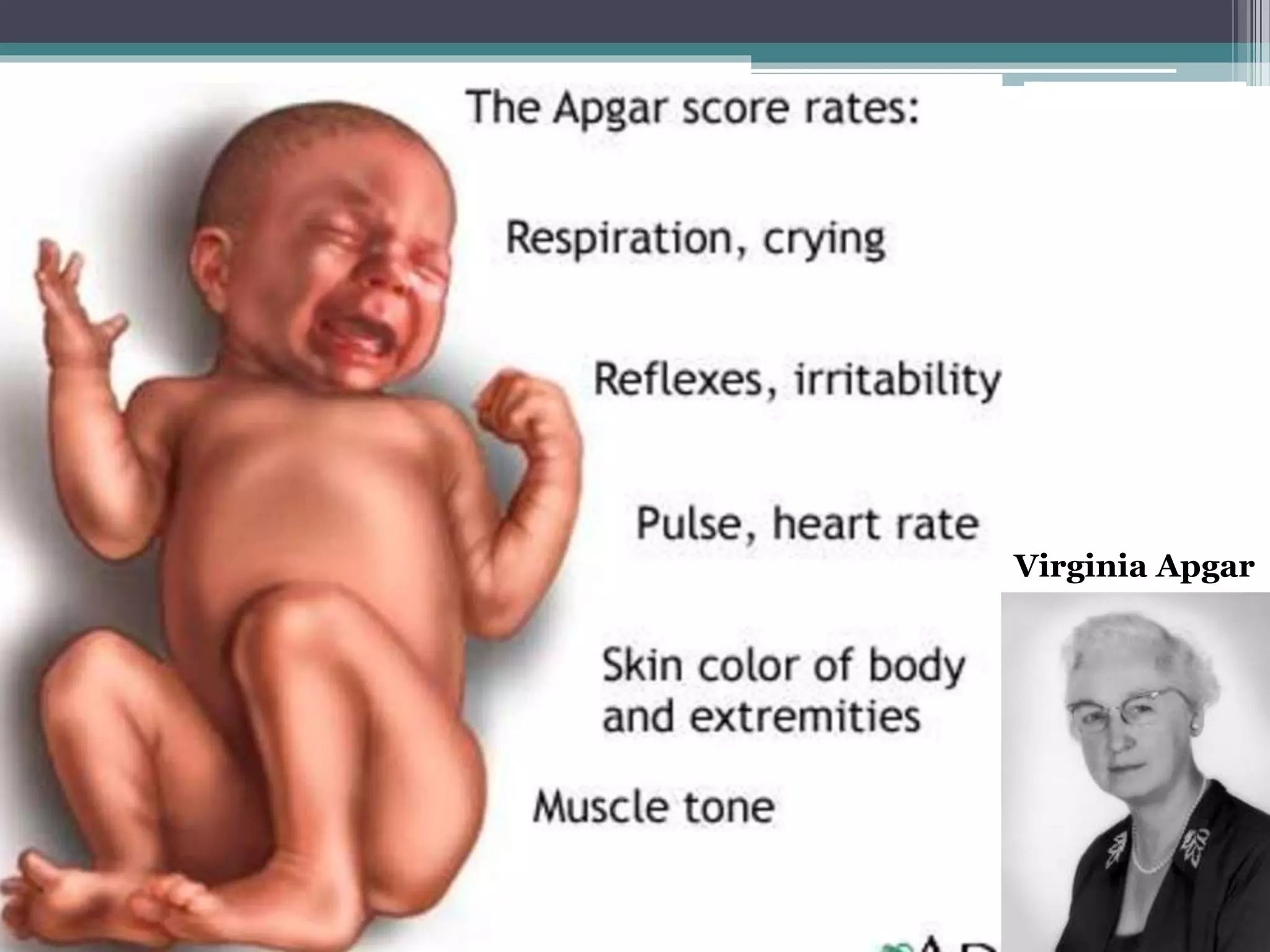
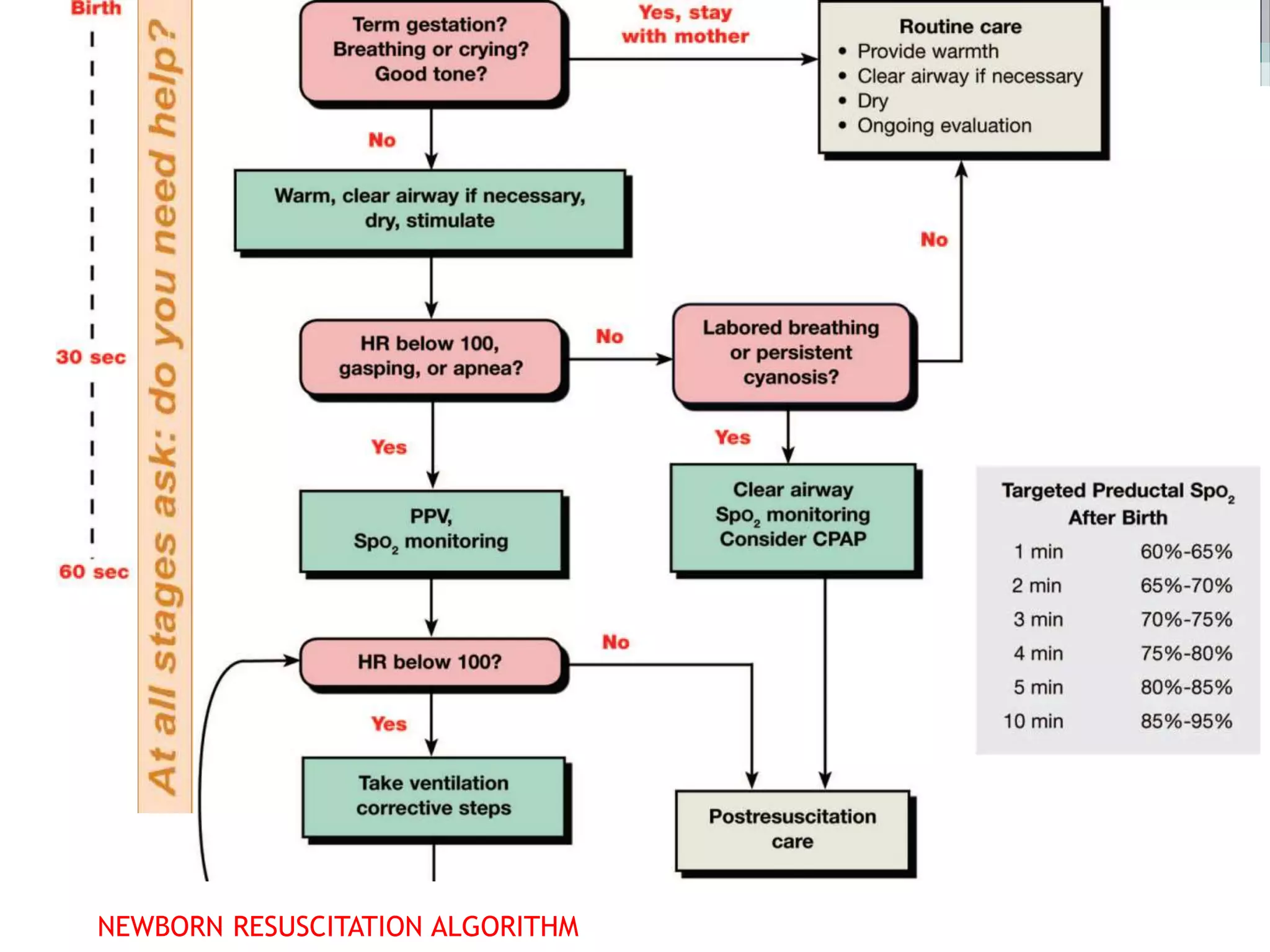
Neonatal resuscitation refers to the series of actions taken to assist newborns struggling to transition from intrauterine to extrauterine life, with around 10% needing some assistance and less than 1% requiring extensive procedures. Essential steps include assessment via the APGAR score, initial stabilization, and various forms of resuscitation, such as airway management and ventilation techniques. The document outlines the necessary equipment, procedures, and evaluation methods for effective resuscitation, emphasizing the importance of timely interventions and accurate assessment of the newborn's condition.