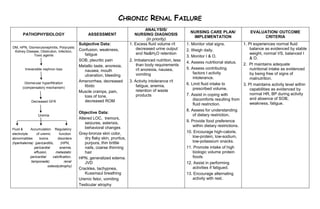
Nursing care plan chronic renal failure
- 1. CHRONIC RENAL FAILURE ANALYSIS/ NURSING CARE PLAN/ EVALUATION/ OUTCOME PATHOPHYSIOLOGY ASSESSMENT NURSING DIAGNOSIS IMPLEMENTATION CRITERIA (in priority) Subjective Data: 1. Excess fluid volume r/t 1. Monitor vital signs. 1. Pt experiences normal fluid DM, HPN, Glomerulonephritis, Polycystic decreased urine output balance as evidenced by stable Kidney Disease, Obstrution, Infection, Confusion, weakness, 2. Weigh daily. Toxic agents fatigue and Na&H2O retention weight, normal VS, balanced I 3. Monitor I & O. & O. SOB, pleuritic pain 2. Imbalanced nutrition, less 4. Assess nutritional status. 2. Pt maintains adequate Metallic taste, anorexia, than body requirements Irreversible nephron loss r/t anorexia, nausea, 5. Assess contributing nutritional intake as evidenced nausea, mouth vomiting factors t activity by being free of signs of ulceration, bleeding intolerance. malnutrition. Glomerular hyperfiltration Amenorrhea, decreased 3. Activity intolerance r/t libido fatigue, anemia, 6. Limit fluid intake to 3. Pt maintains activity level within (compensatory mechanism) prescribed volume. retention of waste capabilities as evidenced by Muscle cramps, pain, products 7. Assist in coping with normal HR, BP during activity loss of tone, discomforts resulting from and absence of SOB, Decreased GFR decreased ROM fluid restriction. weakness, fatigue. 8. Assess for understanding Objective Data: Uremia of dietary restriction. Altered LOC, tremors, seizures, asterixis, 9. Provide food preference behavioral changes within dietary restrictions. Fluid & Accumulation Regulatory electrolyte of uremic function Gray-bronze skin color, 10. Encourage high-calorie, abnormalities toxins disorders dry flaky skin, pruritus, low-protein, low-sodium, (hperkalemia) (pericarditis, (HPN, purpura, thin brittle low-potassium snacks. pericardial anemia, nails, coarse thinning 11. Promote intake of high effusion, metastatic hair biologic volume protein pericardial calcification, HPN, generalized edema. foods tamponade) renal JVD 12. Assist in performing osteodystrophy) Crackles, tachypnea, activities if fatigued. Kussmaul breathing 13. Encourage alternating Uremic fetor, vomiting activity with rest. Testicular atrophy
