Cancer of the Vulva
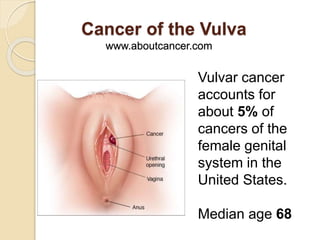
- 1. Cancer of the Vulva www.aboutcancer.com Vulvar cancer accounts for about 5% of cancers of the female genital system in the United States. Median age 68
- 2. Possible signs of vulvar cancer include bleeding or itching should lead to an examination by a physician
- 3. Possible signs of vulvar cancer include bleeding or itching. -A lump or growth on the vulva. -Changes in the vulvar skin, such as color changes or growths that look like a wart or ulcer. -Itching in the vulvar area, that does not go away. -Bleeding -Tenderness in the vulvar area.
- 4. Female Cancers in the US in 2014 Cancer Incidence Deaths Breast 235,030 40,420 Uterus 52,630 8,590 Ovary 21,980 14,270 Cervix 12,360 4,020 Vulva 4,850 1,030 Vagina 3,170 880
- 5. What causes Vulva Cancer? Two independent pathways of vulvar carcinogenesis are felt to currently exist, the first related to mucosal HPV (Human Papilloma Virus) infection second related to chronic inflammatory (vulvar dystrophy) or autoimmune processes
- 6. The risk of developing vulvar cancer is increased by the following: Older age Precancerous changes (dysplasia) in vulvar tissues Lichen sclerosus, which causes persistent itching and scarring of the vulva Human papillomavirus (HPV) infection Cancer of the vagina or cervix Heavy cigarette smoking Chronic granulomatous disease (a hereditary disease that impairs the immune system)
- 8. SEER rates for new vulvar cancer cases have been rising on average 0.5% each year over 2002-2011. Death rates have been rising on average 0.5% each year over 2001-2010.
- 9. Histology and Prognosis About 90% of vulvar carcinomas are squamous cell cancers. Survival is dependent on the pathologic status of the inguinal nodes and whether spread to adjacent structures has occurred.
- 10. Most Common Histologies Squamous: >90% Melanoma: 5-10% Basal Cell: 2% Sarcoma: 1-2% Paget: <1% Bartholin: rare
- 11. Other Histologies Non-neoplastic epithelial disorders of skin and mucosa Lichen sclerosus (lichen sclerosus et atrophicus). Squamous cell hyperplasia (formerly hyperplastic dystrophy). Other dermatoses. VIN vulvar intraepithelial neoplasias Usual type (high-grade 2 and 3). Differentiated type (high-grade 3). Paget disease of the vulva Characteristic large pale cells in the epithelium and skin adnexa. Other histologies Basal cell carcinoma. Histiocytosis X. Malignant melanoma. Sarcoma. Verrucous carcinoma.
- 12. Vulva Anatomy The vulva is the area immediately external to the vagina, including the mons pubis, labia, clitoris, Bartholin glands, and perineum.
- 14. Vulva Anatomy The labia majora are the most common site of vulvar carcinoma involvement and account for about 50% of cases. The labia minora account for 15% to 20% of vulvar carcinoma cases. The clitoris and Bartholin glands are less frequently involved. Lesions are multifocal in about 5% of cases.
- 17. Female Pelvic Lymph Nodes Para-aortic Lateral External Iliac Deep InguinalSuperficial Inguinal Obturator Medial External Iliac Internal Iliac Sacral Highest Deep Inguinal (Cloquet) Sacral Common Iliac
- 18. Pelvic Nodes
- 19. Pelvic Nodes
- 20. Odds of Lymph Node Spread If the groin nodes are enlarged the odds of finding cancer is 59% - 76% If the groin nodes are not enlarged the odds 25-35% (16-24%) If there is cancer in the groin nodes the odds of cancer in the pelvic nodes is 28 - 30%
- 21. Odds of Lymph Node Spread Depth of Tumor Positive Groin Nodes <1mm 0% 1-2mm 7% 2-3mm 8% 3-4mm 22% 4-5mm 25% Size of Tumor <2cm 19% > 2cm 42% < 3cm 18-19% > 3cm 29-72% Extended beyond the Vulva 54%
- 22. Stage I Tumor confined to the vulva. IA Lesions ≤2 cm in size, confined to the vulva or perineum and with stromal invasion ≤1.0 mm, no nodal metastasis. IB Lesions >2 cm in size or with stromal invasion >1.0 mm, confined to the vulva or perineum, with negative nodes. Stage II Tumor of any size with extension to adjacent perineal structures (1/3 lower urethra, 1/3 lower vagina, Vulva Stage System
- 23. Stage I and II Vulva Cancer
- 24. Stage III Tumor of any size with or without extension to adjacent perineal structures (1/3 lower urethra, 1/3 lower vagina, anus) with positive inguino- femoral lymph nodes. IIIA (i) With 1 lymph node metastasis (≥5 mm), or (ii) 1–2 lymph node metastasis(es) (<5 mm). IIIB (i) With 2 or more lymph node metastases (≥5 mm), or (ii) 3 or more lymph node metastases (<5 mm). IIIC With positive nodes with extracapsular spread.
- 25. Stage III Vulva Cancer
- 26. PET-CT Scan Stage III Vulva Cancer
- 27. Stage IV Tumor invades other regional (2/3 upper urethra, 2/3 upper vagina), or distant structures. IVA Tumor invades any of the following: (i) upper urethral and/or vaginal mucosa, bladder mucosa, rectal mucosa, or fixed to pelvic bone, or (ii) fixed or ulcerated inguino-femoral lymph nodes. IVB Any distant metastasis including pelvic lymph nodes.
- 28. Stage and Survival in the US (2004-2010) SEER Stage Incidence 5 Year Relative Survival Local 59% 86% Regional 32% 54% Distant 5% 16%
- 29. Survival with Vulva Cancer Reported 5 year Survival Node Negative: 70 – 93% Node Positive: 25 - 41%
- 30. Stage Distribution NCDB 2000-2011 Stage Percent Stage 0 29% Stage I 29% Stage II 14% Stage III 12% Stage IV 6%
- 31. Observed Survival NCDB 2003-2006 Stage Percent Stage 0 92% Stage I 81% Stage II 59% Stage III 43% Stage IV 21%
- 32. Five-Year Survival by Stage and Node Status Clinical FIGO Stage I 98% II 85% III 74% IV 31% Node Status Groin Negative 91% Groin Positive 52% Pelvic Positive 11%
- 33. 5 Year Survival Stage Survival I 79% II 59% III 43% IV 13%
- 34. Surgery Area removed Area removed Partial Vulvectomy Radical Vulvectomy
- 35. Surgery Until the 1980’s, the standard therapeutic approach was radical surgery, including complete en bloc resection of the vulva and regional lymph nodes.
- 36. In tumors clinically confined to the vulva or perineum, radical local excision with a margin of at least 1 cm has generally replaced radical vulvectomy; separate incision has replaced en bloc inguinal node dissection; ipsilateral inguinal node dissection has replaced bilateral dissection for laterally localized tumors; and femoral lymph node dissection has been omitted in many cases.
- 37. Modern Treatment Early Stage: Radical Local Excision More Advanced: Modified Radical Excision with Sentinel Node Biopsy Advanced Stage: Radiation plus Chemotherapy (chemoradiation) possibly followed by limited surgery
- 39. Sentinel Node Biopsy Node metastases were identified in 26% of sentinel node procedures, and these patients went on to full inguinofemoral lymphadenectomy. The patients with negative sentinel nodes were followed with no further therapy. Side Effects Node Dissection Sentinel Nodes wound breakdown 34% 11.7% cellulitis 21% 4.5% lymphedema 25% 2%
- 40. Frequency of Bilateral Nodes Midline: 70% Laterally ambiguous: 58% Lateral position: 22%
- 42. Radiation Instead of Surgery for Lymph Nodes About 20-35% of patients will be found to have spread to the groin lymph nodes Small study compared surgery with radiation to the groin and there were more relapse in the radiation group (18% versus 0%) so the study was discontinued The radiation dose was very low in the study so the results may not be valid
- 43. Radiation Instead of Surgery for Lymph Nodes Women with positive groin nodes were randomized between pelvic node surgery or radiation. Radiation was superior with better survival (51%/6y versus 41%) Lower vulva cancer mortality (29% versus 51%) and less chronic lymphedema (16% s 22%)
- 44. PostOp Radiation Lympho-vascular invasion depth of invasion > 5mm margins < 8mm positive surgical margins more than one + node node with extracapsular invasion
- 45. Indications for Chemoradiation -Anorectal, urethral, or bladder involvement (in an effort to avoid colostomy and urostomy) -Disease that is fixed to the bone -Gross inguinal or femoral node involvement (regardless of whether a debulking lymphadenectomy was performed)
- 46. Chemoradiation for Squamous Cancer of the Vulva Chemotherapy: 5FU plus cisplatin or mitomycin Radiation: 40 – 65Gy range Cure Rate: 25-75% range
- 47. Locally-Advanced Squamous Cell Carcinoma of the Vulva Treated With Definitive Radiation Therapy Records of all patients treated for squamous cell carcinoma of the vulva between 1980 and 2011 were reviewed International Journal of Radiation Oncology • Biology • Physics Volume 87, Issue 2, Supplement, Pages S129–S130, October 1, 2013
- 48. Eighty-eight patients were identified whose only vulvar treatment was radiation therapy (RT) +/- chemotherapy (CT) due primarily to unresectable disease or co-morbidities Median prescribed dose of RT to the vulva was 64 Gy The median age 67 years Clinical FIGO stages were T1 (10%), T2 (65%), or T3 (25%); 70% had clinically positive inguinal nodes. The Median tumor size was 5 cm.
- 49. Overall Survival rate for all patients was 50% at 5 yrs. Local Recurrence rate in the vulva for all patients was 25% at 5 yrs. Incidence of late grade 3 and 4 toxicities was 4% for gastrointestinal and 10% for genitourinary.
- 50. CT scan is obtained at the time of simulation CT images are then imported into the treatment planning computer
- 51. In the simulation process the CT and PET scan images are used to create a computer plan
- 52. Cross section anatomy of the female pelvis
- 53. CT Scans are used to identify the target structures for radiation bowel sacrum Iliac bone Pelvic nodes Pre-sacral nodes
- 54. CT Scans are used to identify the target structures for radiation bowel nodes vagina bladder rectum hips
- 56. IMRT (the colored areas are the radiation zones) Pelvic nodes Pelvic nodes Rectum Groin nodes Vulva/Vagina Vulva
- 57. Computer reconstruction of radiation fields to cover groin and pelvic lymph nodes but avoid the bladder and rectum in vulva cancer patient
- 58. Tomotherapy fields used to hit the groin and pelvic nodes but avoid the bladder and rectum
- 59. Side Effects of Pelvic Radiation
- 60. Side Effects of Vaginal/Vulvar Radiation •Vaginal and vulva skin burning irritation or discharge •Urethra irritation or frequency •Anus burning
- 61. Cancer of the Vulva www.aboutcancer.com
