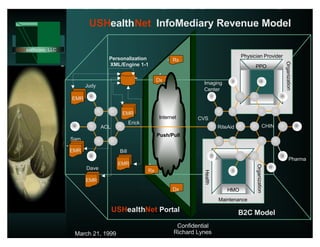
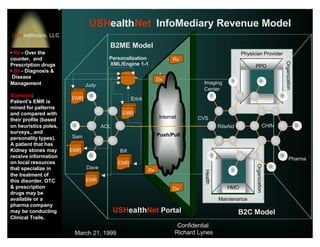
USHealthNet will provide an integrated internet application service platform for healthcare professionals and consumers. For professionals, it will integrate administrative, communication, and research functions into a single web-based solution. For consumers, it will offer a free health, wellness, and self-service portal. The company plans to partner with other healthcare companies and acquire physicians and their patients to build a large user base. Its goal is to lower costs for physicians while improving care quality and patient relationships.









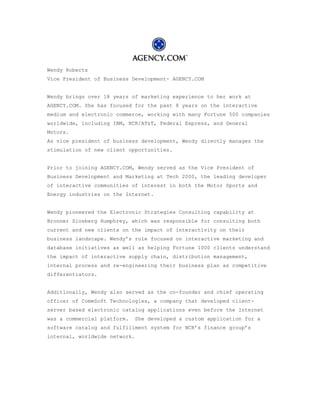
![Application Review
and each participant is dependent on the others for parts of that information. In sum, the finance and
delivery of healthcare requires that consistent, accurate information be shared confidentially across a
large and fragmented industry.
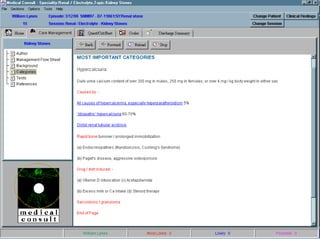
Underlying Technology
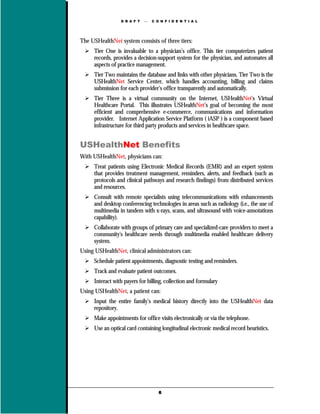
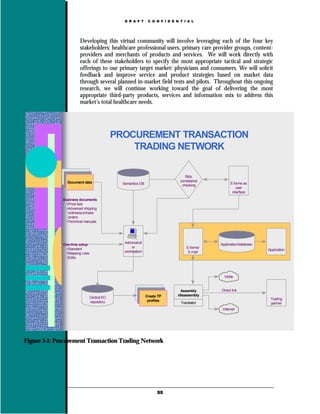
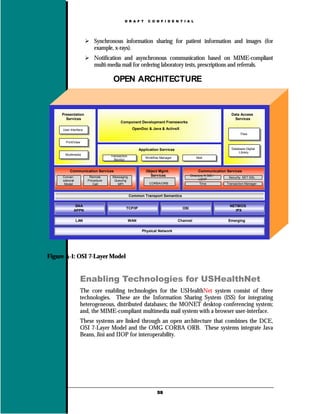
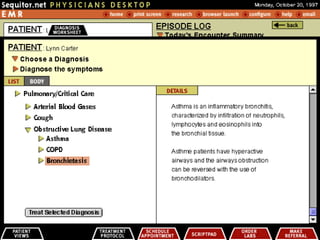
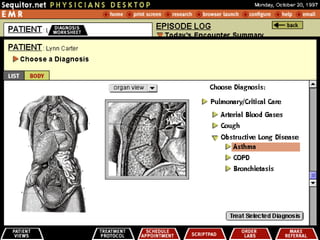
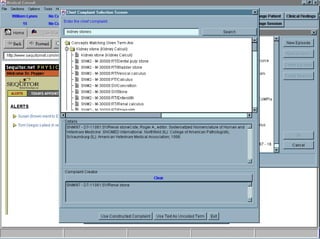
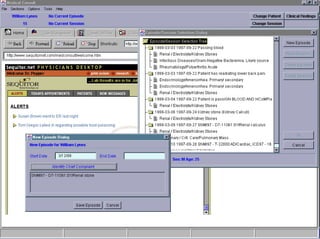
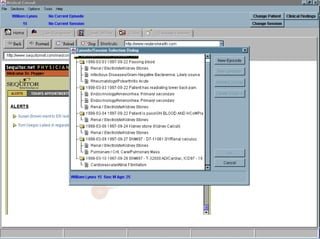
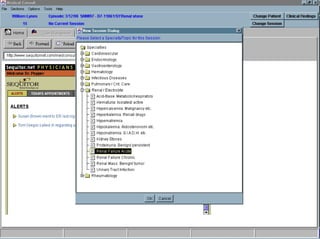
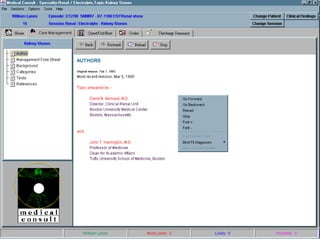
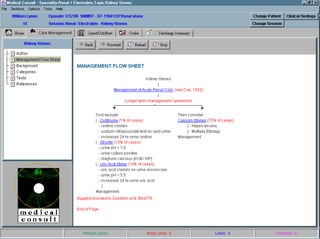
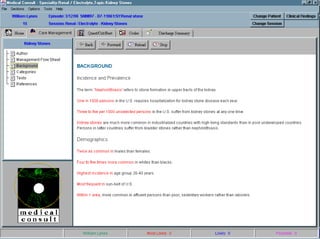
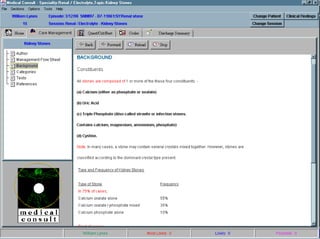
USHealthNet's iASP offering consists of an N-tiered application service strategy, which connects
physicians and patients to USHealthNet's portal through a single access point using a Web browser based
Thin-Client interface. These services integrate critical Point-of-Care Knowledge Tools allowing secure
global access over the Internet. These POC tools will be offered for free to consumers and through the
Company's premium subscription services for healthcare professionals. Further access is offered to
branded affiliate products and services, maximizing site stickiness while ensuring a consistent user
experience.
USHealthNet's Java Enterprise Beans and Corba application component framework supporting the iASP
subscription service offering will consist of nine integrated applications:
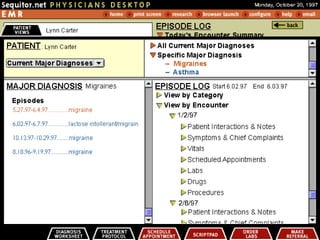
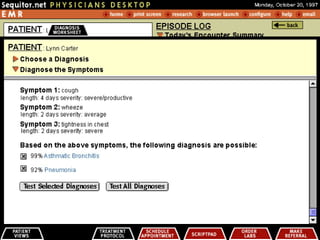
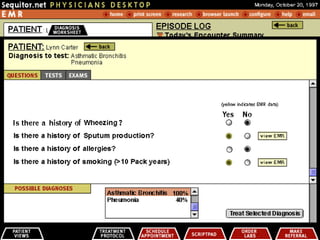
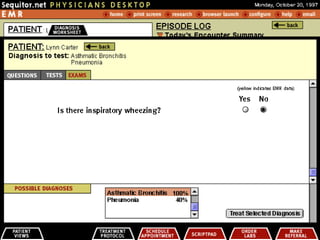
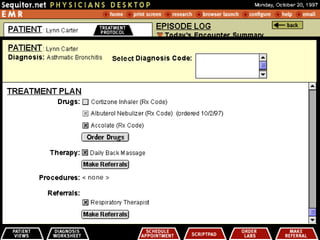
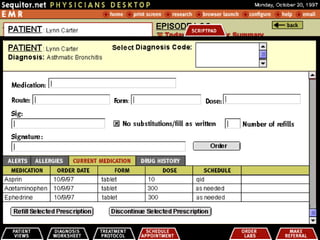
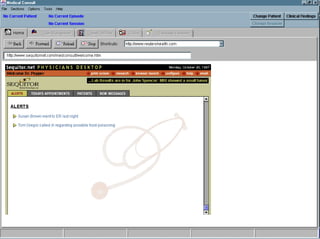
1. LifeTime (Longitudinal Electronic Medical Records)
2. DiagAssist (Diagnostic Decision Support System)
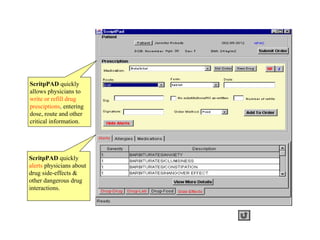
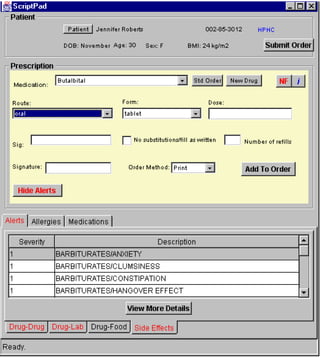
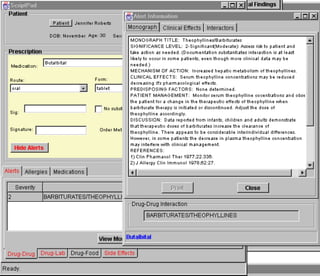
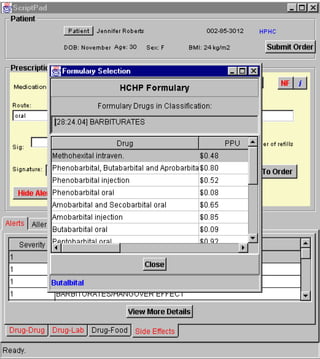
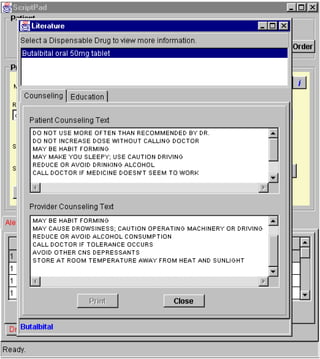
3. ScriptPad (Prescription and Drug Interaction Services)
4. LabDirect (Lab Order and Results)
5. Enterprise Workflow Engine and XFDL/XML based Forms Engine
6. Enterprise Resource Planning (ERP)
7. Enterprise Master Patient Index (EMPI)
8. Clinical Data Repository and OLAP
9. Java XML Search Engine, integrating (UMLS) Tools and semantic networks
Intellectual Properties
Do to the nature of providing our outsourcing iASP offerings, several key technology partners have been
identified and will require license agreements.
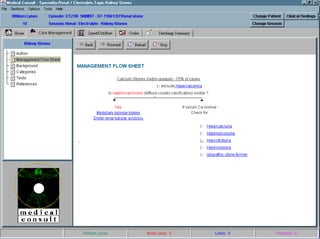
Manufacturing Process
We have an outsourcing agreement in place for all custom development and integration services through
our strategic partnership with a local Boston based developer.
Sales (return to top)
Unique selling proposition
The Value Proposition - Healthcare Professional
A Web-based Thin-Client front-end application provides a Single Point of Access for healthcare
professionals. This reduces the need for healthcare professionals to use multiple administrative,
communications and information services by integrating these applications and services via the Internet.
USHealthNet will enter into relationships to assist healthcare professionals in obtaining all hardware and
ancillary services necessary to use USHealthNet, including Internet access, computer hardware, training,
and support. USHealthNet's Premium subscription access to iASP and Knowledge Management Services
provides a suite of Point-of-Care (POC) tools, including backend EDI services for healthcare
http://www.garage.com/garage/preview.shtml (3 of 15) [6/16/1999 2:46:37 AM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-14-320.jpg)




![Application Review
In addition, USHealthNet does not have contractual rights to prevent its strategic partners from entering
into competing businesses or directly competing with the USHealthNet. While these statements can be
positioned as a negative resulting in a high-risk investment, they represent the reality of market
conditions for every company today and well into the future.
Competitive Advantage
USHealthNet's integrated Web service delivery model (iASP) positions the true competitive situation
with a more focused strategic value proposition.
Many of the more sessioned players in the healthcare market have been traditional product companies,
which would prevent them from competing in the Internet service space in the short-term. These
companies are not the usual first-movers and early adopters. They have funded business plans build
around a product model company and operational structures to support them. Product development life
cycles constrain traditional product companies from the point of view that measures success by
time-to-market, mass customization, personalization, and elasticity to rapidly changing market dynamics.
Many of these companies will seek security in partnership strategies that include them in the markets
natural trends toward consolidation and disintermediation.
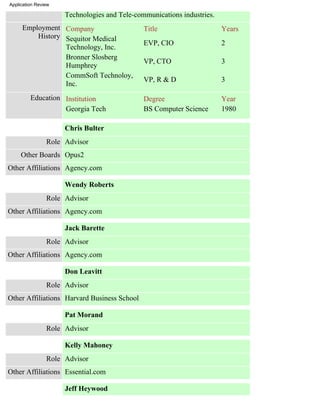
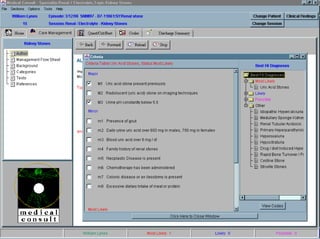
Management & Staffing (return to top)
Full-time permanent employees: 1
Part-time employees: 0
Contractors: 7
Critical positions not yet filled
CEO, COO, Chief Marketing Officer, SVP Business Development, VP Research & Development
Personnel
Richard Lynes
Role Founder
Title CTO
Functions Provide IT vision and strategy alignment
http://www.garage.com/garage/preview.shtml (9 of 15) [6/16/1999 2:46:37 AM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-20-320.jpg)


![USHealthNet
USHealthNet
Business Plan
for USHealthNet, a visionary
Health Care Information Delivery System.
June 11, 1999
Business Plan Copy Number [1 of 50 ]
This document contains confidential and proprietary information
belonging exclusively to Richard Lynes
Richard Lynes
Chief Technology Officer
3 Acorn Street
Scituate, MA 02066
(781) 545-3938
cto@mediaone.net
This is a business plan. It does not imply an offering of Securities.
Confidential & Proprietary Property of Richard Lynes
Draft Only – June 11, 1999](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-27-320.jpg)





















![Worldmachine Technologies Corporation
http://www.worldmachine.com/ [6/11/1999 3:14:50 AM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-56-320.jpg)
![[Home] - Internet, intranet, extranet web development
Welcome!
Worldmachine Technologies is a leading consulting and
engineering firm specializing in the development of
highly-functional Internet, intranet, and extranet web sites.
We provide businesses with innovative and effective ways to
manage their information and improve their communications.
Our web site provides current information about our company
and the services and solutions that we offer, so please use
the links to the left to navigate throughout our site. We
suggest that you view the company overview as well as our
series of online solution demonstrations.
A full web site directory and search engine can also be found
on our site map (to the upper right).
Be sure to give us a call at (617) 357-4040, or email us at
sales@worldmachine.com if you would like to learn more
about what Worldmachine can do for you.
company | solutions | technology | resources | careers | contact | extranet
© 1999 · Worldmachine Technologies Corporation
44 Winter Street · Boston, MA 02108 · (617) 357-4040
http://www.worldmachine.com/index.html [6/11/1999 3:15:06 AM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-57-320.jpg)
![Fujitsu - Total Cost of Ownership Introduction
Total Cost of Ownership
Fujitsu Ergo$ave - The first quantitative analysis
Introduction
What are the real costs of owning your PC?
It is a lot more than just the initial purchase price.
According to the Gartner Group, the initial purchase price
of a PC accounts for only 14% of the Total Cost of
Ownership (TCO) over its average lifetime.
This is a very significant figure and Fujitsu aims to remove the jargon and
one which has resulted in TCO being a explain what TCO really means for you.
key agenda item for senior IT
managers. Many PC vendors have tried What is Total Cost of Ownership?
to market TCO as part of their product
offering in a vague manner - Fujitsu is What do the expert research
the first company to actually quantify consultants say?
TCO for large companies.
Fujitsu Ergo$ave, what is it ?
By developing Fujitsu Ergo$ave,
Fujitsu has taken TCO one stage Fujitsu Ergo$ave in practice
further by developing a tool that
clearly demonstrates the savings that Conclusion... I want an Ergo$ave demo
can be made specifically for your
organisation - a quantifiable audit of
your PC strategy.
http://www.fujitsu-computers.com/coo/main.html [6/14/1999 4:09:48 PM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-58-320.jpg)

![Worldmachine Technologies Corporation
http://www.worldmachine.com/ [6/9/1999 12:55:05 PM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-60-320.jpg)
![[Home] - Internet, intranet, extranet web development
Welcome!
Worldmachine Technologies is a leading consulting and
engineering firm specializing in the development of
highly-functional Internet, intranet, and extranet web sites.
We provide businesses with innovative and effective ways to
manage their information and improve their communications.
Our web site provides current information about our company
and the services and solutions that we offer, so please use
the links to the left to navigate throughout our site. We
suggest that you view the company overview as well as our
series of online solution demonstrations.
A full web site directory and search engine can also be found
on our site map (to the upper right).
Be sure to give us a call at (617) 357-4040, or email us at
sales@worldmachine.com if you would like to learn more
about what Worldmachine can do for you.
company | solutions | technology | resources | careers | contact | extranet
© 1999 · Worldmachine Technologies Corporation
44 Winter Street · Boston, MA 02108 · (617) 357-4040
http://www.worldmachine.com/index.html [6/9/1999 12:55:15 PM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-61-320.jpg)











































































































![UMLS Metathesaurus
Fact Sheet
UMLS ® Metathesaurus ®
The UMLS Metathesaurus is one of three knowledge sources developed and distributed by the National Library of Medicine
as part of the Unified Medical Language System® (UMLS®) project. The Metathesaurus contains information about
biomedical concepts and terms from many controlled vocabularies and classifications used in patient records, administrative
health data, bibliographic and full-text databases and expert systems. It preserves the names, meanings, hierarchical
contexts, attributes, and inter-term relationships present in its source vocabularies; adds certain basic information to each
concept; and establishes new relationships between terms from different source vocabularies.
The Metathesaurus supplies information that computer programs can use to interpret user inquiries, interact with users to
refine their questions, identify which databases contain information relevant to particular inquiries, and convert the users'
terms into the vocabulary used by relevant information sources. The scope of the Metathesaurus is determined by the
combined scope of its source vocabularies. The Metathesaurus is produced by automated processing of machine-readable
versions of its source vocabularies, followed by human review and editing by subject experts. The Metathesaurus is intended
primarily for use by system developers, but can also be a useful reference tool for database builders, librarians, and other
information professionals.
The Metathesaurus is organized by concept or meaning. Alternate names for the same concept (synonyms, lexical variants,
and translations) are linked together. Each Metathesaurus concept has attributes that help to define its meaning, e.g., the
semantic type(s) or categories to which it belongs, its position in the hierarchical contexts from various source vocabularies,
and, for many concepts, a definition. A number of relationships between different concepts are represented. Some of these
relationships are derived from the source vocabularies; others are created during the construction of the Metathesaurus. Most
inter-concept relationships in the Metathesaurus link concepts that are similar along some dimension. The Metathesaurus
also includes use information, including the names of selected databases in which the concept appears, and, for MeSH®
terms, information about the qualifiers that have been applied to the terms in MEDLINE®. Information on the
co-occurrence of concepts in MEDLINE and in some other information sources is also included.
Content of the Metathesaurus
The 1999 version of the Metathesaurus contains 626,893 biomedical concepts with 1,358,891 different concept names from
about 50 source vocabularies. Important additions for 1999 include the Beth Israel Clinical problem list vocabulary; the
Alcohol and Other Drug Thesaurus; clinical drug terminology derived from Micromedex; the Pharmacy Practice Activity
Classification; the Patient Care Data Set, which contains detailed nursing terminology; Alternative Billing Concepts, used to
bill for procedures by licensed practitioners of alternative therapies; a small initial set of valid values for segments of HL7
messages; and terminology used to characterize cancer research projects. Many existing source vocabularies have been
updated to more current versions, including SNOMED, the Read Codes, LOINC, and MeSH®. A complete list of the
UMLS Metathesaurus source vocabularies appears in the Appendix to the License Agreement for the Use of UMLS
Products. Statistics for the number of strings present from each source appear in the UMLS Documentation Appendix B.3.
Metathesaurus Applications
The Metathesaurus is used in a wide range of applications including: information retrieval from databases with human
assigned subject index terms and from free-text information sources; linking patient records to related information in
bibliographic, full-text, or factual databases; natural language processing and automated indexing research; and structured
data entry. In many cases, the utility of the Metathesaurus is enhanced when it is used in combination with the SPECIALIST
http://www.nlm.nih.gov/pubs/factsheets/umlsmeta.html (1 of 2) [5/28/1999 10:19:22 PM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-231-320.jpg)
![UMLS Metathesaurus
Lexicon, the lexical programs, and the UMLS Semantic Network. To obtain coherent, comparable results in data creation
applications, such as patient data entry, it is necessary to define which Metathesaurus concepts and terms can be included in
the records being created. This may be done by selecting one or more of the many Metathesaurus source vocabularies which
provide the most appropriate concepts and terms for the specific data being created. Other Metathesaurus concepts and terms
will then provide synonyms and related terms which can help to lead users to the vocabularies selected for a particular data
creation application.
The 1999 edition of the UMLS Knowledge Sources includes Metamorphosys, software useful in producing customized
versions of the Metathesaurus.
Obtaining the UMLS Metathesaurus
NLM does not charge for the Metathesaurus (or other UMLS products) and it is available to both U.S. and international
users. Those who wish to obtain the UMLS Metathesaurus and the other UMLS Knowledge Sources must sign a License
Agreement for the Use of UMLS Products and send it to the address at the end of the agreement. Licensees are responsible
for complying with the restrictions on use of the contents of the UMLS Metathesaurus that are detailed in the agreement.
Some uses of some Metathesaurus source vocabularies require separate agreements, which may involve fees, with the
individual vocabulary producers.
The UMLS Metathesaurus is available to licensees via ftp, Web interface, and applications program interface (API) from the
UMLS Knowledge Source Server. It is also available on CD-ROM by explicit request. A complete description of the
Knowledge Sources and their distribution formats can be found in the UMLS Documentation.
Other Fact Sheets in the UMLS series: Unified Medical Language System, UMLS Semantic Network, SPECIALIST
Lexicon, and UMLS Knowledge Source Server.
For additional information contact: E-mail: custserv@nlm.nih.gov or 1-888-FINDNLM
U.S. National Library of Medicine (NLM)
http://www.nlm.nih.gov/
Last updated: 1 March 1999
http://www.nlm.nih.gov/pubs/factsheets/umlsmeta.html (2 of 2) [5/28/1999 10:19:22 PM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-232-320.jpg)
![Unified Medical Language System
Fact Sheet
Unified Medical Language System
Background:
In 1986, the National Library of Medicine, (NLM) began a long-term research and development project to build a Unified
Medical Language System® (UMLS®). The purpose of the UMLS is to aid the development of systems that help health
professionals and researchers retrieve and integrate electronic biomedical information from a variety of sources and to make
it easy for users to link disparate information systems, including computer-based patient records, bibliographic databases,
factual databases, and expert systems. The UMLS project develops machine-readable "Knowledge Sources" that can be used
by a wide variety of applications programs to overcome retrieval problems caused by differences in terminology and the
scattering of relevant information across many databases.
UMLS Development Strategy:
The project is directed by a multi-disciplinary team of NLM staff. NLM encourages broad use of the UMLS products by
distributing annual editions free-of-charge under a license agreement. The Knowledge Sources are iteratively refined and
expanded based on feedback from those applying each successive version.
UMLS Knowledge Sources:
There are three UMLS knowledge sources:
q UMLS Metathesaurus
q SPECIALIST Lexicon
q UMLS Semantic Network
The Metathesaurus provides a uniform, integrated distribution format from about 50 biomedical vocabularies and
classifications and links many different names for the same concepts. The Lexicon contains syntactic information for many
Metathesaurus terms, component words, and English words, including verbs, that do not appear in the Metathesaurus. The
Semantic Network contains information about the types or categories (e.g., "Disease or Syndrome," "Virus") to which all
Metathesaurus concepts have been assigned and the permissible relationships among these types (e.g., "Virus" causes
"Disease or Syndrome"). NLM also distributes associated lexical programs and software helpful in producing customized
versions of the UMLS Metathesaurus.
NLM has discontinued release of the UMLS Information Sources Map.
UMLS Applications:
NLM and many other institutions are applying the UMLS Knowledge Sources in a wide variety of Applications including
patient data creation, curriculum analysis, natural language processing, and information retrieval. NLM's own applications
include Internet Grateful Med® , and PubMed.
An issue of NLM's Current Bibliographies in Medicine series, Unified Medical Language System® (UMLS®), covers the
structure and semantics of the UMLS Knowledge Sources, their development and maintenance, and assessments of their
coverage and utility for particular purposes, and the full range of UMLS applications. It contains 280 citations covering the
period from January 1986 through December 1996. More recent references can be found by searching for Unified Medical
http://www.nlm.nih.gov/pubs/factsheets/umls.html (1 of 2) [5/28/1999 10:19:31 PM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-233-320.jpg)
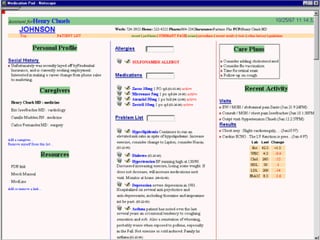
![Other Web-based EMR Projects
Web based EMR or Clinical Information Systems
Project/Product Organization Contact
Guardian Angel MIT Peter Szolovitz PhD
W3 EMRS Harvard University/Children's Hospital I. Kohane MD, PhD
Web/Java based ICU monitoring Spacelabs Medical Corporation/Boston University K. Wang PhD
ARTEMIS West Virginia University's Juggy PhD
Web based CIS Columbia University J.J. Cimino MD
Virtual EMR Hewlett-Packard/Virginia Neurological Institutes James Kazmer
Web access project. Massachusetts General Hospital
Web access project University of Missouri in Columbia
Primary Rheumatology Web Munich University Project W. Swobada
The GEODE-CM Harvard Medical School Paul Eric Stoufflet MD
SPIDER Medical College of Wisconsin C. Kahn MD
Java Interface to THE ELECTRONIC
Duke University Medical Center D. Pollard MBA
MEDICAL RECORD
Affinity Marina L. Douglas RN
CompuCare
MS
ChartMax MedPlus
Web based system Telemachus Inc/TMAC
Benefit Management Healtheon Corporation David Shnell MD
MediVault Service Emergency Medical Systems Inc.
Oacis Healthcare Systems Inc.
Araxys Solution Araxys Inc.
Webpatient System Syracuse University
Intranet product Lawson Software
Webrad Analogic Inc. P. Keezer
ALI Webserver ALI
Freeview (gateway for viewing
Passport Technologies division of Elscint Inc.
DICOM-3 images)
Webrad Radiology department at Georgetown University
Hospital
Healthcare Online Daou Systems
Dept. of Family Medicine and Pediatrics,
Java based CPR A.E Zuckerman MD
Georgetown University School of Medicine
Virtual Medical Manager Secureware Inc./Emory University Charles Watt PhD
Regenstrief Institute for Health Care, Indiana
Web interface to CIS J.M. Overhage MD PhD
University
Web access to ultrasound Indiana University School of Medicine A.M. Golichowski MD
http://www.telemedical.com/webemr.htm (1 of 3) [5/28/1999 10:44:49 PM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-234-320.jpg)
![Other Web-based EMR Projects
Web interface to childhood
LCS at MIT E.M. Jordan SM
immunizations
Section on Medial Informatics and Dept of
Webreport H.J. Lowe MD
Pathology at University of Pittsburg
TeleMed Los Alamos National Laboratory D.W. Forslund PhD
Web version of the PIS and RxPad PDX Inc.
RxMed
QSINET Quality Systems Inc.
Avicenna Systems Synetic Corporation
EnVenture Health Systems Integration Inc.
Care-Web Institute for Interventional Informatics Dave Warner MD
IDXtendR Outreach IDX Cedric Priebe MD
CareNet Praxis Corporation/Datahouse Inc.
ClinicalWare CompuRad division of LumisysInc.
Wang Inc.
Integrated Healthcare Solutions
Eclipsys Inc.
Internet Prescription Ordering Physician's Online Inc.
Clinical Information System Kaiser Foundation John Maddison MD
Axolotl Inc.
HBOC Inc.
Medicalogic Inc.
Medica Computer Systems/MYSYS LTD
Oceania
Protocol Systems
Health Systems Technologies Inc.
HealthMagic Inc.
Advanced Medical Systems Inc.
UCSD/SAIC Project
Medvision
Healthdesk Inc.
VitalWorks Inc.
Healtheon Inc.
Masterchart
Lucent's HRM system
SMS
Cerner
Object Products Inc.
http://www.telemedical.com/webemr.htm (2 of 3) [5/28/1999 10:44:49 PM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-235-320.jpg)
![Other Web-based EMR Projects
Websight Dynamic Healthcare Technologies Inc.
This list is being researched and created by Foster P. Carr MD. and is the 1996-1997 copyright of Digital Med Inc., All
rights are reserved
http://www.telemedical.com/webemr.htm (3 of 3) [5/28/1999 10:44:49 PM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-236-320.jpg)
![Duke Medical Informatics Research
Duke Medical Informatics Research
Research activities in the Division of Medical Informatics at Duke include:
q computer-based patient record systems
q decision support systems
q hospital information systems
q computer-assisted management protocol systems
q standards development
q security, confidentiality, and privacy
q medical data mining
Much of the current research in the division is centered around The Medical Record
(TMR), a comprehensive longitudinal computer-based patient record system
(CPRS) developed at Duke University over the last 25 years. TMR provides total
administrative, financial, and medical management capabilities for the patient
encounter.
The TMR record focuses on the patient as an individual. Rather than storing
information as a series of unrelated accounting transactions, TMR creates an
integrated medical and accounting database which allows detailed reviews of both
health and financial history.
TMR - The Medical Record
q Introduction
q Appointment Section
q The Patient Encounter: Check-in
q The Patient Encounter: Medical
q The Patient Encounter: Check-out
http://dmi-www.mc.duke.edu/dukemi/research/research.html (1 of 2) [5/28/1999 10:45:33 PM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-237-320.jpg)
![TITLE
Calendar of Download Become a OMG
Press Room OMG Store Contact Us
Events Specifications Member Publications
The OMG
OMG Home
About the OMG CORBA Med Specification
Member Companies
Liaison Relationships by Chapter
OMG News & Info
How We're Organized
Staff Contacts & Partners
For your convenience we have provided you with the discrete chapter
CORBA
CORBA for Beginners breakdown of formal/99-03-01: CORBA Med Specification to make it
Success Stories easy for you to copy/print the sections you are interested in. The full
CORBAnet
Products and Services Guide
CORBA Meds document is also available as a single downloadable file
CORBA Academy Training here, for those who wish to copy/print the book in its entirety.
Free Stuff
Copies of the CORBAMed book in the printed binder form will be
The OMA available for purchase on our website after April 1st, 1999. After this
IDL Text Files
CORBA/IIOP date you will be able to order through our Ordering Department using our
Domain Interfaces on-line Order From on the Web at /store/publications.html.
Common Facilities
CORBA Services
CORBA Telecoms
CORBA Finance
Index
CORBA Med
MOF Documents
UML Cover Page
Table of Contents Page
Technology Process
Form for Reporting Issues Chapter 1 - Overview
OMG Revision Issues
Chapter 2 - Person ID specification
Technical Commitee Groups
Technology Process FAQ Chapter 3 - Lexicon Query
RFI FAQ
Index
TC Home Pages
TC Work in Progress
TC Deadlines
TC Vote Status
Technical Library Cover
Library Index
Document Search
99-03-02.pdf
About OMG Documentation 99-03-02.ps
Presentation Library
Listen to the Experts Return to Index
Whitepapers
Meeting Information
Table of Contents
99-03-03.pdf
http://www.omg.org/corba/cmchptr.html (1 of 2) [5/28/1999 10:57:31 PM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-238-320.jpg)




























![The ASP Market
The ASP Market
ASP.
Unheard of even a year ago, the term 'ASP' is now used all over the industry. But what is an ASP?
ASP is an acronym for Application Service Provider. As outsourcers of enterprise applications, at the bare
minimum ASPs take on the hosting and application service needs of companies whose core competencies
are not in information technology (IT). A large draw for middle market customers is that ASPs can
essentially work with their IT departments to host complex applications for e-commerce, human resources,
and financial management solutions. ASPs offer them access to Fortune 500 applications to which they
were previously denied.
USi: A Superior ASP
But not every company using the term ASP can deliver the same service. Some outsourcers only offer
co-location or hosting, yet claim the ASP title. Any company considering an ASP to outsource their
enterprise solutions would do well to ask the ASP the following key questions.
How many software partners do they have? What are the capabilities of their network? How quickly can
they get your solution up and running? What kind of capital outlay will you have to provide up-front?
How large is their technical staff? How much expertise do they possess to implement and manage your
application, and respond to any emergency? Is their network secure? Is it redundant, failsafe, and
geographically mirrored? How fast is their connectivity?
Are regular software and network upgrades included in the service? Do they offer contracts with service
level agreements and project timeframes that include financial penalties when these promises are not met?
A top of the line ASP can offer all of this so its clients don't have to — and USi aspires to over-reach these
benchmarks. USi has partnerships with a number of best-of-breed software vendors, Cisco-Powered
Global Network, and a partnership with telco U S WEST. This ensures that our clients have multiple
outsourcing options, can leverage a world-class network, and have high-speed Internet access and
performance.
Info | News | Products | Technology | Sales | Careers | Events | Support | Contact
Site Search - Enter Keywords Below
search
http://www.usinternetworking.com/news/features/99-05-24-asp.html [6/2/1999 2:34:01 PM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-267-320.jpg)
![Phrma: Publications: Industry Profile 1998, Chapter 4
Value Brochure
Biomedicine
Leading the way
Return to Table of Contents
Annual Report
Health Guides
Ind. Profile '99
q Pharmaceutical Expenditures in Perspective
q Cost-effectiveness of Pharmaceuticals
q From the Manufacturer to the Patient
q Compliance with Medication Regimens
Prescription drugs not only prolong life and improve the quality of life, they also
frequently reduce or replace more expensive forms of medical treatment such as
hospitalization, nursing care, and surgery. With the great potential for continued
pharmaceutical breakthroughs, prescription drugs will continue to play an important
role in containing costs, even as overall health-care expenditures increase.
PHARMACEUTICAL EXPENDITURES
IN PERSPECTIVE
Rising health-care costs can be attributed to several factors, notably demographic
shifts in the population and the explosion of life-prolonging innovation. In 1997, total
national health expenditures (NHE) in the United States amounted to 1.1 trillion
dollars—13.5 percent of gross domestic product (GDP)—according to the Health
Care Financing Administration. The share of GDP allocated to health has nearly
doubled since 1970, when it was just 7.4 percent.
Beyond 2010, the aging of the population will have a significant impact on
health-care spending. Those 65 and older are about 13 percent of the population
today and account for roughly 34 percent of health expenditures. As baby boomers
enter their 70s and 80s, the share of the population 65 and over will exceed 20
percent. Because the frequency and intensity of health-care utilization increase
sharply with age, this demographic shift will raise health expenditures.
The U.S. currently devotes a higher percentage of GDP to health expenditures than
http://www.phrma.org/publications/industry/profile99/chap4.html (1 of 9) [6/16/1999 1:15:41 PM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-268-320.jpg)
![Phrma: Publications: Industry Profile 1998, Chapter 4
any other major industrialized country [Figure 4-1]. Since 1980, the gap has widened
between the U.S. and other industrialized countries in the share of GDP allocated to
health. In contrast, the share of GDP devoted to pharmaceuticals in the U.S. is about
average for an industrialized country [Figure 4-2]. Since 1980, the share of GDP
allocated to pharmaceuticals also has increased in the U.S., although this has been at
a much slower rate than with other health-care components and is in line with
increases elsewhere. These data suggest that pharmaceutical expenditures do not
contribute to higher than average health expenditures in the U.S.
Overall, the proportion of health expenditures allocated to outpatient prescription
drugs in this country has declined from past levels, but has risen somewhat in recent
years [Figure 4-3]. In 1965, 9.0 percent of health expenditures was allocated to
prescription drugs. In 1997, the percentage was 7.2.
In relation to consumer spending on other items, expenditures on prescription drugs
are relatively small. According to the Department of Commerce, per capita personal
consumption expenditures on pharmaceuticals averaged 64 cents a day in 1997. This
compares to consumer expenditures of $8.45 a day on housing, $7.94 on food, $2.84
on clothing, and $1.07 on telephone services [Figure 4-4].
COST-EFFECTIVENESS OF
PHARMACEUTICALS
Prescription-drug therapy is highly cost-effective. Other interventions—such as
surgery, hospitalization, physician visits, and nursing care—are typically
time-consuming and expensive. Prescription-drug therapy often eliminates the need
for these costly interventions. Until cures are discovered, incremental advances in
drug therapies often reduce treatment costs by controlling symptoms and alleviating
pain.
Ulcer therapy illustrates the progression of drug innovation and its ability to lower
medical costs. Prior to the advent of H2 antagonist drug therapy in 1977, 97,000
operations were performed for ulcers each year.1 By 1987, the number of surgeries
had dropped to 18,926. In the early 1990s, the annual cost of drug therapy per person
amounted to about $900, compared to $28,000 for surgery.2 The discovery that the H.
pylori bacterium is the principal cause of ulcers has led to the use of antibiotics in
combination with H2 antagonists to treat duodenal ulcers. At a cost of about $140 per
patient, combination therapies now eradicate the bacterial cause of most ulcers. More
recent examples of the cost-effectiveness of prescription drugs include:
q For asthma patients, increased drug spending keeps patients out of the hospital.
Results from the Virginia Health Outcomes Partnership program for Medicaid
asthma patients demonstrated an average 42 percent decline in the rate of
emergency room and hospital urgent care visits. In a little more than one year
after the program was implemented, it saved Medicaid about $285,000. Had
the program been in effect throughout the state—rather than in just seven
http://www.phrma.org/publications/industry/profile99/chap4.html (2 of 9) [6/16/1999 1:15:41 PM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-269-320.jpg)
![Phrma: Publications: Industry Profile 1998, Chapter 4
counties—it is estimated that the savings could have topped $2 million.
q In a year-long disease-management program for about 1100 patients with
congestive heart failure run by Humana Hospitals, pharmacy costs increased by
60 percent, while hospital costs declined 78 percent. The net savings were $9.3
million.3
q Researchers at the National Bureau of Economic Research recently examined
the overall costs of treating heart attacks and depression, two conditions for
which drugs play an important role. They found that the total cost of restoring
health for heart attack patients has fallen by about 1 percent annually from
1984 through 1991.4 Similarly, researchers found that the aggregate price of
treating acute major depression fell by 25 percent during 1991–1995.5 These
trends highlight the cost-effectiveness of prescription drugs and the need for
health-care plans to examine prescription drug costs comprehensively in the
context of the overall costs of treating patients.
q A recent study sponsored by NIH found that treating stroke patients promptly
with a clot-busting drug not only reduces disability—it also saves health-care
costs. The study showed that while it initially costs more to treat patients with
the drug, the expense is more than offset by reduced rehabilitation and nursing
home costs.6 Treatment with the clot-buster costs an additional $1.7 million per
1,000 patients. But reduced rehabilitation and nursing-home costs result in net
savings of more than $4 million for every 1,000 patients [Figure 4-5].
According to NIH, use of the clot-busting drug in the tens of thousands of
eligible stroke patients could amount to savings to the health-care system in
excess of $100 million per year.7
q A study published in the American Journal of Managed Care shows that a new
drug for migraine headaches is lowering the total cost of caring for patients
with this disease. Although drug expenditures for patients in the study
increased, the total costs of treating these patients for migraine headaches
declined 41 percent as a result of treatment with the new drug.8 Another study
showed that the drug lowered lost-labor costs and reduced employees’ lost
productivity due to migraines. The benefit to employers of this reduction in
lost productivity was valued at $435 per month per employee [Figure 4-6]. In
contrast, the cost of the drug was $43.78 per month. The benefit-to-cost ratio
was 10 to 1.9
q A study released by the Agency for Health Care Policy and Research in
September 1995 concluded that increased use of a blood-thinning drug would
prevent 40,000 strokes a year, saving $600 million. In economic terms, the
lifetime cost of a stroke exceeds $100,000, while the average annual cost of
drug therapy and monitoring is $1,025.10
q In a 1993 study, cancer patients whose immune systems were weakened by
high-dose chemotherapy were helped by a new pharmaceutical known as a
colony-stimulating factor. The treatment saves $30,000 per patient in
http://www.phrma.org/publications/industry/profile99/chap4.html (3 of 9) [6/16/1999 1:15:41 PM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-270-320.jpg)
![Phrma: Publications: Industry Profile 1998, Chapter 4
hospitalization costs for bone-marrow transplants [Figure 4-7].
q A study published in the New England Journal of Medicine showed that
patients on ACE inhibitors for congestive heart failure avoided nearly $9,000
each in hospitalization costs over a three-year period—and that the drug
reduced deaths by 16 percent. The potential savings for Americans with heart
failure amounts to $2 billion a year.11
q A drug for schizophrenia has enabled many patients to be treated outside the
hospital, in less costly settings, according to a 1990 study. The annual cost of
the drug therapy was $4,500, compared to more than $73,000 a year for
treatment in a state mental institution. Between 133,000 and 189,000
schizophrenia patients could potentially be helped by schizophrenia therapy.12
q Patients with kidney disease who suffer anemia may be treated with drug
therapy at an annual cost of $3,600 to $4,000 a patient. Drug therapy saves
$6,540 a patient in the cost of medical care plus costs associated with reduced
productivity, such as lost wages.13
q Immunosuppressive drugs have dramatically improved the success rate of
organ-transplant surgery by preventing patients’ immune systems from
destroying the new tissue. One of these drugs was found to shorten average
hospital stays by as much as 10 days and reduce rehospitalization after kidney
transplants. The cost of postoperative hospitalization may be nearly $10,000
less for patients treated with the drug.14
q Combination drug therapy of three medicines—including a protease
inhibitor— can reduce the AIDS virus in many patients to undetectable levels,
enabling them to return to work and reducing the need for hospitalization. The
annual cost of the three-medicine therapy ranges from $10,000 to $16,000. In
contrast, the cost of treating advanced AIDS in a hospital is estimated at
$100,000 a year [Figure 4-8; also see box on HIV/AIDS in Chapter 1].
q A 1994 study published in the Journal of the American Medical Association
estimated that a routine chicken pox vaccination program in the U.S. would
save $391 million annually in work-loss costs [Figure 4-9]. Work-loss costs
include the value of work missed by adults with chicken pox and the value of
work parents miss when their children are sick.
q Use of a cholesterol-lowering drug in patients with angina or who have had a
heart attack increases life expectancy in men and women of various ages and
varying cholesterol levels, according to a Scandinavian study. The
Scandinavian researchers analyzed the direct costs saved by this therapy for
people of different ages and cholesterol levels and found that savings ranged
from $3,800 per year of life for 70-year-old men with cholesterol levels over
300, to $27,400 per year of life for 35-year-old women with cholesterol levels
in the lower 200s.15
http://www.phrma.org/publications/industry/profile99/chap4.html (4 of 9) [6/16/1999 1:15:41 PM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-271-320.jpg)
![Phrma: Publications: Industry Profile 1998, Chapter 4
q The 6,595-patient "West of Scotland Coronary Prevention Study" found that a
cholesterol-lowering drug reduced the risk of heart attack by 31 percent and the
risk of death from all cardiovascular causes by 32 percent in individuals who
have elevated cholesterol levels, but have never had a heart attack. These
findings showed for the first time that cholesterol-lowering drugs could prevent
heart disease and reduce the risk of death.16
q The Centers for Disease Control estimates that every $1 spent on the vaccine
for measles-mumps-rubella (MMR) saves the health system $21, every $1
spent on the oral polio vaccine saves $6, and every $1 spent on the
diphtheria-tetanus-pertussis vaccine saves $30.17 The introduction of the oral
polio vaccine eliminated the need to build the national iron-lung centers
envisioned by the government in the 1950s, saving billions of dollars.18
q Cases of bacterial meningitis among young children dropped nearly 80 percent
over 11 years after the introduction of a vaccine, saving $135 million a year in
avoided hospital costs.19
q Bronchial-mucolytic therapy for cystic fibrosis, when used in conjunction with
standard therapies, was proven in clinical trials to reduce the risk of
respiratory-tract infections requiring IV antibiotic therapy by 27 percent,
reducing costly hospitalizations and other related medical costs.20
q Estrogen-replacement therapy can help aging women avoid osteoporosis and
crippling hip fractures, a major cause of nursing-home admissions.
Estrogen-replacement therapy costs approximately $3,000 for 15 years of
treatment, while a hip fracture costs an estimated $41,000.21
FROM THE MANUFACTURER
TO THE PATIENT
The cost-effectiveness of prescription drugs—combined with a steady stream of
new-product introductions—has contributed to healthy industry growth since 1970,
when sales amounted to $6.6 billion [Figure 4-10]. Sales by research-based
pharmaceutical companies are projected to reach $134.1 billion in 1999, a 7.6 percent
increase from $124.6 billion in 1998. Sales within the United States by both
U.S.-owned and foreign-owned research-based companies account for $91.8 billion
of the 1998 total. Sales abroad by U.S.-owned companies account for the remaining
$42.3 billion.
According to data published by the health- care information company IMS Health,
the main drivers of growth in the late 1990s have been non-price factors, including
increased volume of prescriptions, record sales of new products and new product
formulations, and the changing mix of available products being used.22 In 1998, 80
percent of industry growth was due to non-price factors [Figure 4-11]. IMS data
differ from the sales figures quoted above because they include all products on the
http://www.phrma.org/publications/industry/profile99/chap4.html (5 of 9) [6/16/1999 1:15:41 PM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-272-320.jpg)
![Phrma: Publications: Industry Profile 1998, Chapter 4
market as well as added costs from drug wholesalers.
In 1997, manufacturers’ net U.S. sales of human-use prescription pharmaceuticals
amounted to $71.8 billion and was dominated by five major product classes. In 1997,
the largest class was pharmaceuticals acting on the central nervous system, with
$14.4 billion or 21.9 percent of manufacturers’ U.S. sales [Figure 4-12]. Over the
same period, products acting on the digestive or genito-urinary system generated $9.0
billion or 13.6 percent of sales. Cardiovasculars accounted for $11.5 billion or 17.5
percent. Anti-infectives sales totaled $9.6 billion or 14.6 percent. Sales of
pharmaceuticals affecting neoplasms (cancers), the endocrine system, and metabolic
diseases amounted to $12.1 billion or 18.4 percent of U.S. sales. Smaller classes
included respiratory products with 10.9 percent of the market, dermatological
products with 2.1 percent, and vitamins and nutrients with less than 1 percent.
Pharmaceutical manufacturers’ sales are mainly to large drug wholesalers.
Wholesalers, in turn, distribute the products to retail pharmacies, hospitals, HMOs,
clinics, mail-order companies, and other organizations that fill prescriptions. In 1998,
78.4 percent of sales of human-use ethical pharmaceuticals flowed through
wholesalers, up from 71.8 percent in 1990, and 57.3 percent in 1980 [Figure 4-13].
In 1998, the retail sector—including independent, chain, food store, and mass-
merchandise pharmacies—dispensed more than 2.1 billion prescriptions, according to
IMS Health. In terms of dollar sales, retail channels account for over 64 percent of
dispensed prescription sales in the U.S. [Figure 4-14]. Sales by hospital pharmacies
account for 12.8 percent of the market, mail-order pharmacies comprise 10.8 percent,
clinics 6.1 percent, long-term care pharmacies 3.1 percent, and staff-model HMOs
1.5 percent. More than 90 percent of HMOs contract with retail pharmacies to fill
prescriptions.23
COMPLIANCE WITH
MEDICATION REGIMENS
Unless patients take their medicines according to physicians’ instructions and
systems are in place to guard against adverse drug interactions, prescription drugs
may not be used cost-effectively. It is estimated that only about half of prescribed
medicines are taken correctly.
Noncompliance is a costly problem—for employers, insurers, the health-care system
and, of course, patients. The National Pharmaceutical Council (NPC), an industry
research organization, estimates that noncompliance costs more than $100 billion a
year, due to increased hospital admissions, nursing-home admissions, lost
productivity, and premature deaths.24 Noncompliance results in more hospital
admissions, emergency-room care, physician visits, and, occasionally, surgeries.
There are also serious personal consequences. For example, failure to take
contraceptives can lead to unwanted pregnancies, failure to take
estrogen-replacement medication can cause osteoporosis, and failure to take
http://www.phrma.org/publications/industry/profile99/chap4.html (6 of 9) [6/16/1999 1:15:41 PM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-273-320.jpg)
![Phrma: Publications: Industry Profile 1998, Chapter 4
hypertension medicine can result in heart attack or stroke.
Compliance rates vary with the disease and setting of the patient group. According to
data reported in the Journal of Clinical Pharmacy and Therapeutics, patients in homes
for the aged had relatively high rates of compliance, as did patients in the first year of
antihypertensive treatment. In contrast, patients taking penicillin for rheumatic fever
had relatively low rates of compliance.
The National Council on Patient Information & Education (NCPIE) divides
noncompliance into two categories: acts of omission and acts of commission. Acts of
omission include never filling a prescription; taking less than a prescribed dosage;
taking a medicine less frequently than prescribed; taking medicine "holidays"; and
stopping a regime too soon. Acts of commission include overuse; sharing medicines:
and consuming food, drink, or other medicines that can interact with a prescribed
drug.
One way to improve compliance is to provide patients with easy-to-understand
information about their medicines. As a result of voluntary, private-sector programs,
more than 60 percent of patients now receive written information about their
medicines with their prescriptions. This percentage increases every year.
ENDNOTES
1. Boston Consulting Group, The Contribution of Pharmaceutical Companies:
What’s at Stake for America, September 1993.
2. PhRMA, based on data supplied by the Health Care Financing Administration,
1993.
3. "Provide Education about Congestive Heart Failure and Pump Up Your
Savings," Managed Healthcare, April 1998, Vol. 8, No. 4, pp. 42–44.
4. Cutler, D., et al., "The Costs and Benefits of Intensive Treatment for
Cardiovascular Disease," American Enterprise Institute/Brookings Institution,
December 1997.
5. Frank, R.G., et al., "Price Indexes for the Treatment of Depression," American
Enterprise Institute/Brookings Institution, December 1997.
6. Fagan, S.C., et al., "Cost-effectiveness of Tissue Plasminogen Activator for
Acute Ischemic Stroke," Neurology, Vol. 50, pp. 883–889, 1998.
7. National Institutes of Health, National Institute of Neurological Disorders and
Stroke, "New Stroke Treatment Likely to Decrease Health Care Costs and
Increase Quality of Life," news release, April 22, 1998.
8. Legg, R.F., et al., "Cost-effectiveness of Sumatriptan in a Managed Care
Population," The Journal of Managed Care, Vol. 3, No. 1, January 1997.
9. Legg, R.F., et al., "Cost Benefit of Sumatriptan to an Employer," Journal of
http://www.phrma.org/publications/industry/profile99/chap4.html (7 of 9) [6/16/1999 1:15:41 PM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-274-320.jpg)
![Phrma: Publications: Industry Profile 1998, Chapter 4
Occupational and Environmental Medicine, Vol. 39, No. 7, July 1997.
10. Secondary and Tertiary Prevention of Stroke Patient Outcome Research Team:
9th Progress Report, March 1996.
11. "The SOLVD Investigators," New England Journal of Medicine, Vol. 325, No.
5, pp. 293-302, 1991; Walsh America/PDS.
12. Hospital and Community Psychiatry, Vol. 41, No. 8, 1990.
13. Levy, R.A., "What to Tell Patients About the Cost-Benefit of Medications,"
Wellcome Trends in Pharmacy, January 1993.
14. Showstack, J., et al., "The Effect of Cyclosporine on the Use of Hospital
Resources for Kidney Transplantation," The New England Journal of
Medicine, Vol. 321, No.16, 1989.
15. Johannesson, M., Jonnson, B., et al., "Cost Effectiveness of Simvastation
Treatment to Lower Cholesterol Levels in Patients with Coronary Heart
Disease," New England Journal of Medicine, Vol. 336, pp. 332–336, 1997.
16. Shepherd, J., et al., "Prevention of Coronary Heart Disease with Pravastatin in
Men with Hypercholesterolemia," The New England Journal of Medicine,
November 16, 1995.
17. Medicine and Health, "Vaccines for Children Program: Bad Policy or Start-up
Glitches?" August 15, 1994.
18. Boston Consulting Group, The Contribution of Pharmaceutical Companies:
What’s at Stake for America, September 1993.
19. Adams, W.G., et al., "Decline of Childhood Haemophilus Influenzae Type b
(Hib) Disease in the Hib Vaccine Era," Journal of the American Medical
Association, January 13, 1993, pp. 221–226.
20. Cystic Fibrosis Foundation, "Rationale for the Use of Human
Deoxyribonuclease 1 (rhDNase-Pulmozyme) in Patients with Cystic Fibrosis,"
Consensus Conferences, Volume IV, Section 1, September 22, 1993.
21. Clark, A.J., and Schuttinga, J.A., "Targeted Estrogen/Progestogen
Replacement Therapy for Osteoporosis: Calculation of Health Care Cost
Savings," Osteoporosis International, Vol. 1922, pp. 195–200.
22. IMS, IMS Retail and Provider Perspective, 1998.
23. Hoechst Marion Roussel Managed Care Digest Series: HMO-PPO/Medicaid
Digest, 1998.
24. National Pharmaceutical Council, Noncompliance with Medication Regimens:
An Economic Tragedy, June 1992.
http://www.phrma.org/publications/industry/profile99/chap4.html (8 of 9) [6/16/1999 1:15:41 PM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-275-320.jpg)
![Phrma: Publications: Industry Profile 1998, Chapter 4
Chapter Five: The Changing Pharmaceutical Marketplace
http://www.phrma.org/publications/industry/profile99/chap4.html (9 of 9) [6/16/1999 1:15:41 PM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-276-320.jpg)
![NaviSite, Inc.
NaviSite Breaks Ground for
Advanced Technology Data Center
Facility to Open January 2000 and
Launch Company Into the New
Millennium
NaviSite Announces Strategic
Alliances with Microsoft and Dell
for High Availability Application
Hosting and Management
Microsoft and Dell Raise Internet
Applications Stakes with Equity
Interest in NaviSite
Sign Up! Clear
Copyright © 1998 NaviSite, Inc.
http://www.navisite.com/ [6/21/1999 1:27:58 AM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-277-320.jpg)
![Welcome to USi - The First and Leading Application Service Provider
Go!
Join!
© 1998,1999 USinternetworking, Inc.
|
http://www.usinternetworking.com/ (1 of 2) [6/21/1999 1:28:07 AM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-278-320.jpg)
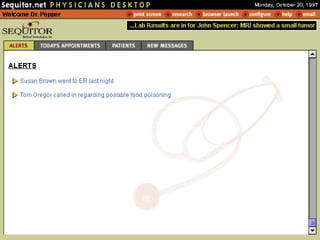
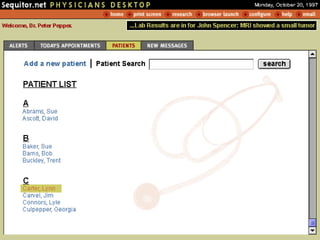
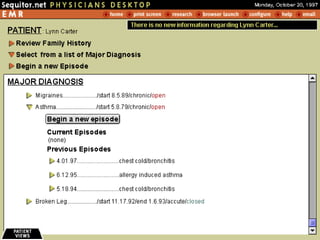
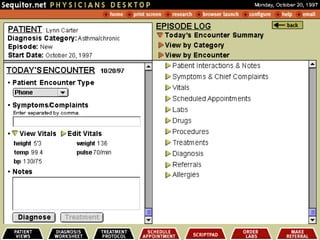
![Start the Presentation
(To view this you will need Netscape 4.0 or greater due to the use of layers)
http://www3.worldmachine.com/dev/sequitor/first.html [6/22/1999 1:05:59 AM]](https://image.slidesharecdn.com/ushealthnetllc-1304091838434-phpapp01/85/Us-Health-Net-Llc-279-320.jpg)