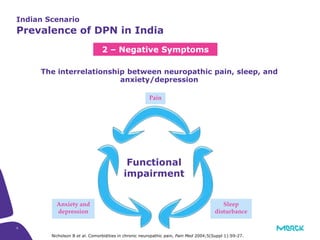
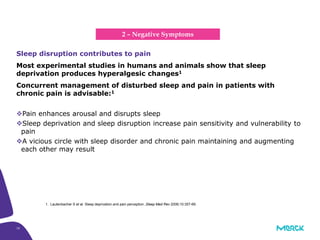
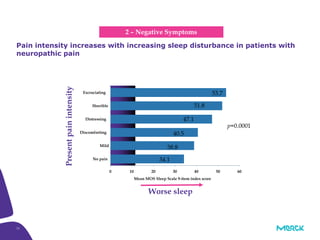
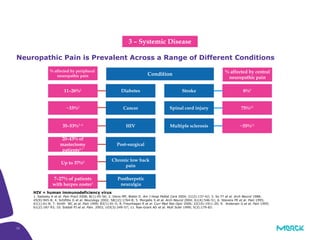
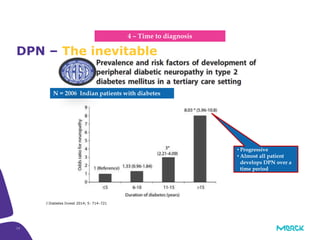
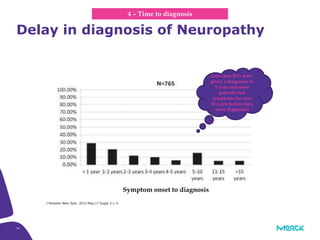
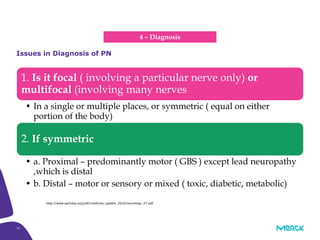
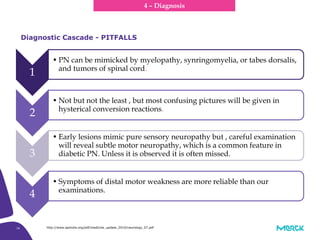
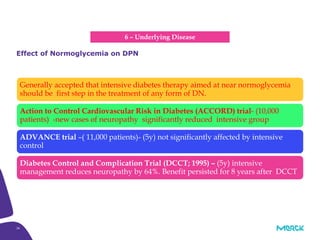
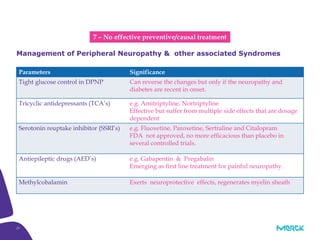
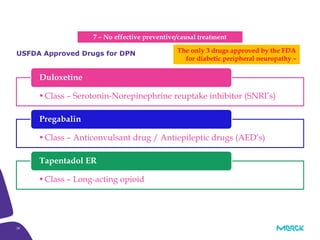
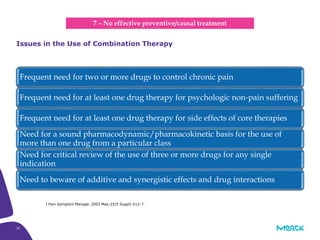
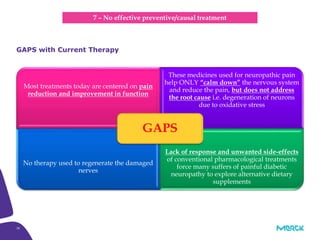
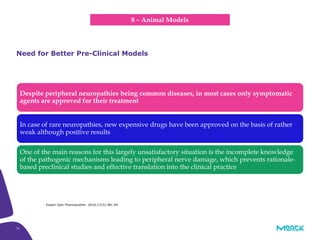
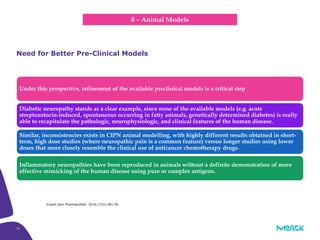
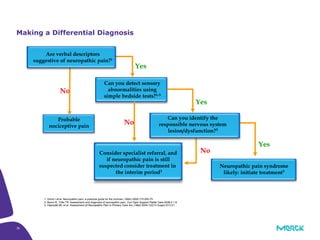
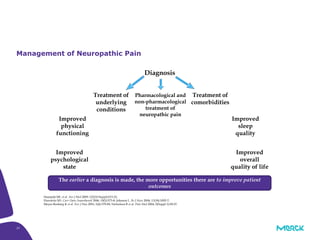
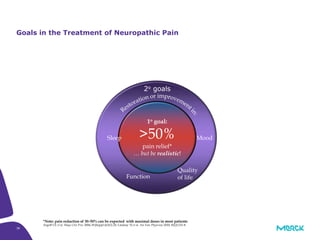
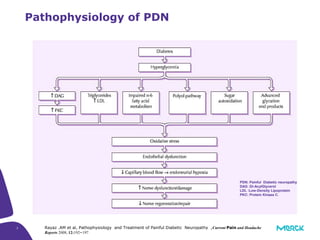
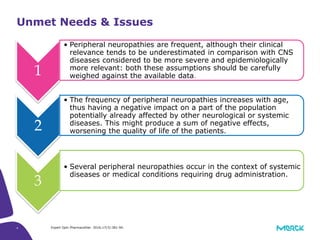
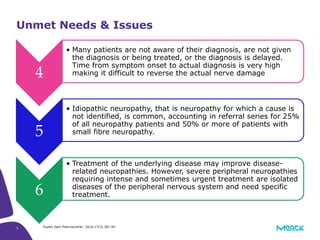
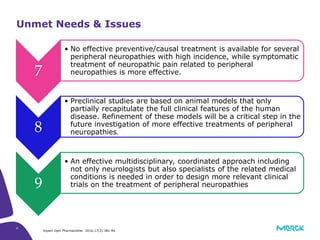
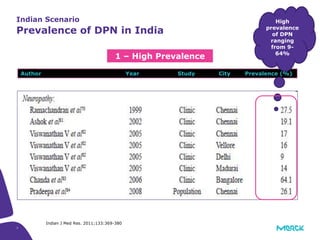
The document discusses the challenges of nerve care in India, particularly focusing on peripheral neuropathy and diabetic peripheral neuropathy (DPN), which have a high prevalence in the population. It highlights issues such as delayed diagnosis, lack of awareness among patients, and the inefficacy of current treatments, particularly regarding preventive measures. The need for a multidisciplinary approach in treatment and the improvement of preclinical models for better understanding and addressing these conditions is also emphasized.

![8
The cases had a mean age of 47.6 ± 10.2 years (59% males)
duration of symptoms of 5.9 ± 8.2 months prior to presentation.
Overall prevalence of DPN was 29.2% [95% CI 22.8-35.7].
PN among matched control was 10.7% (95% CI 3.5-17.8).
Prevalence of DPN showed an increasing trend with age.
J Postgrad Med. 2014 Jul-Sep;60(3):270-5.
1 – High Prevalence
Indian Scenario
Prevalence of DPN in India](https://image.slidesharecdn.com/unmetneedinpnsk-170716163441/85/Unmet-needs-in-Peripheral-Neuropathy-8-320.jpg)