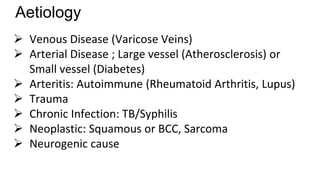
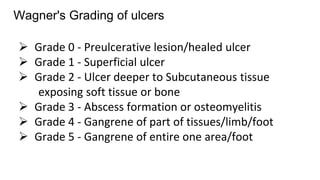
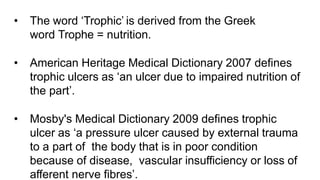
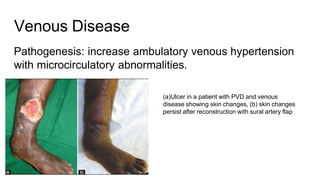
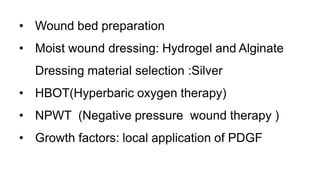
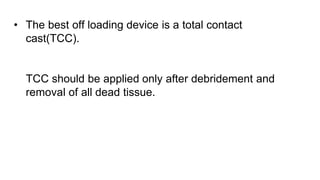
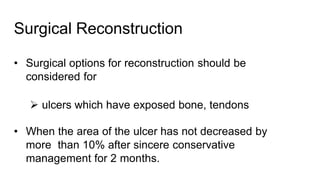
Trophic ulcers develop due to impaired wound healing caused by issues like poor circulation, neuropathy or prolonged pressure. They are classified based on their underlying cause such as diabetic ulcers, pressure sores or venous stasis ulcers. Treatment involves identifying the cause, wound debridement, dressing, offloading pressure, and correcting nutritional deficiencies or vascular issues. For non-healing ulcers, surgical reconstruction with flaps may be needed along with patient education on self-care. A multidisciplinary team approach is required for managing trophic ulcers.