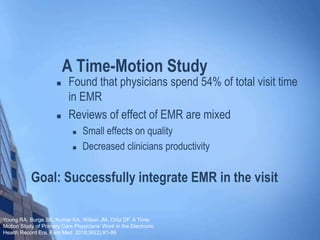
The document discusses the impact of electronic medical records (EMR) on patient-provider interactions, highlighting frustrations when physicians focus more on screens than on patients. It notes that physicians spend 54% of their time in EMR during visits, leading to decreased productivity and mixed effects on care quality. The conclusion emphasizes the need for better EMR integration to enhance patient involvement and make the system more efficient for clinicians.