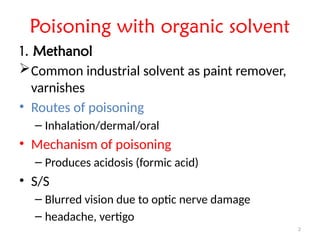
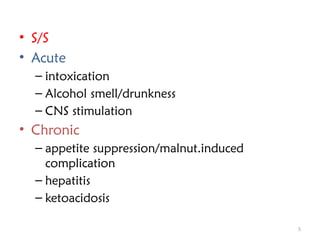
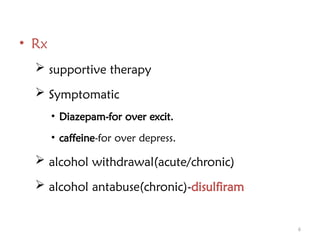
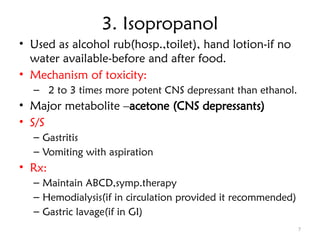
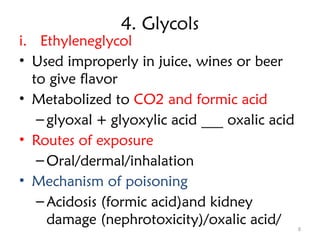
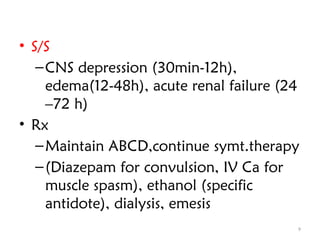
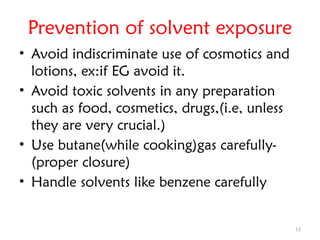
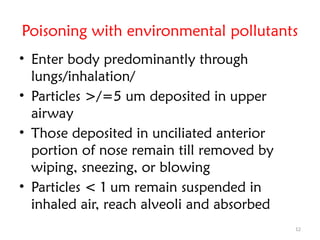
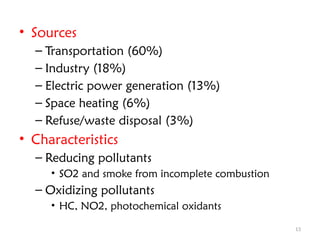
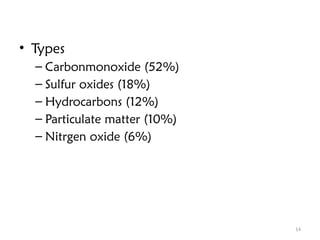
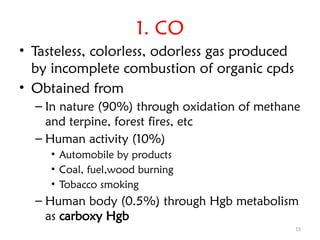
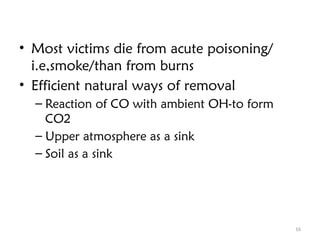
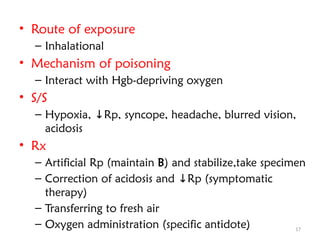
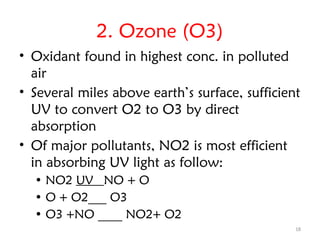
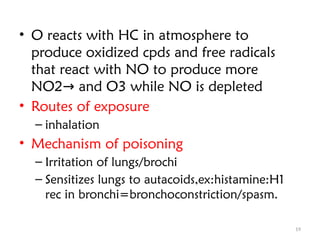
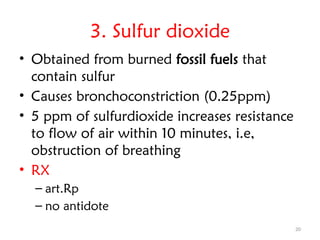
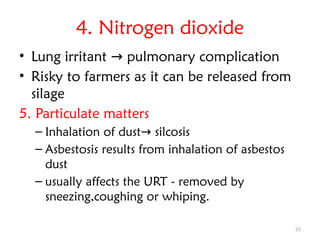
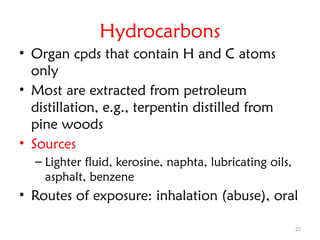
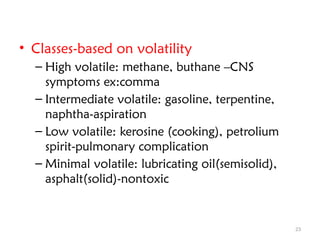
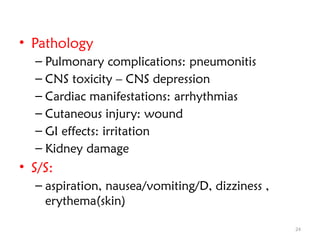
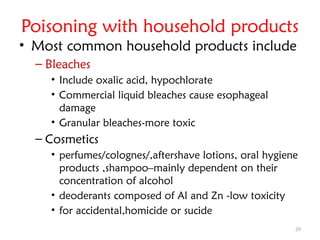
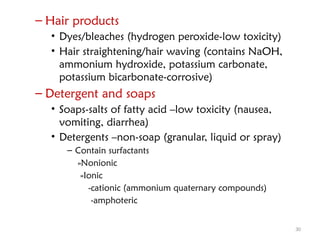
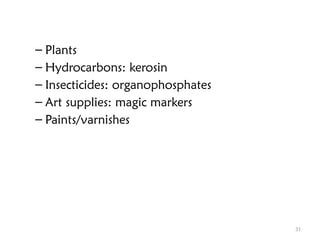
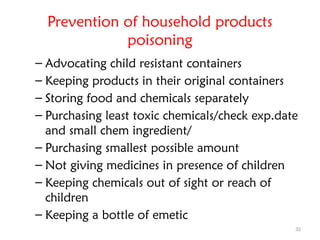
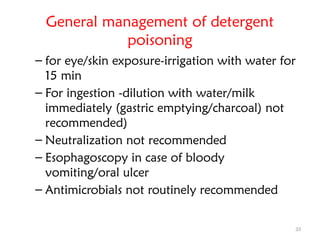
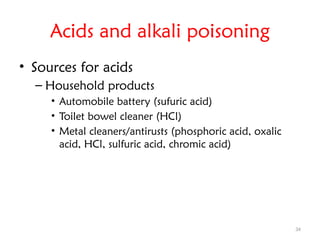
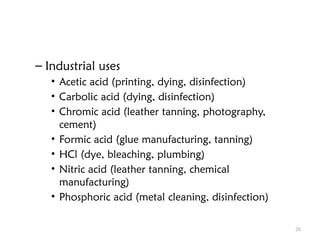
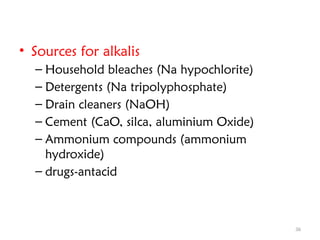
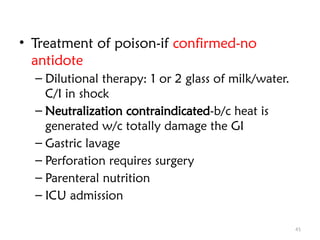
The document discusses various non-metallic environmental toxicants, their sources, routes of exposure, mechanisms of poisoning, clinical effects, and recommended treatments. It covers toxicants such as organic solvents like methanol, ethanol, and isopropanol, as well as glycols, environmental pollutants, food contaminants, and household products. The document emphasizes prevention methods and the general management of poisoning cases.