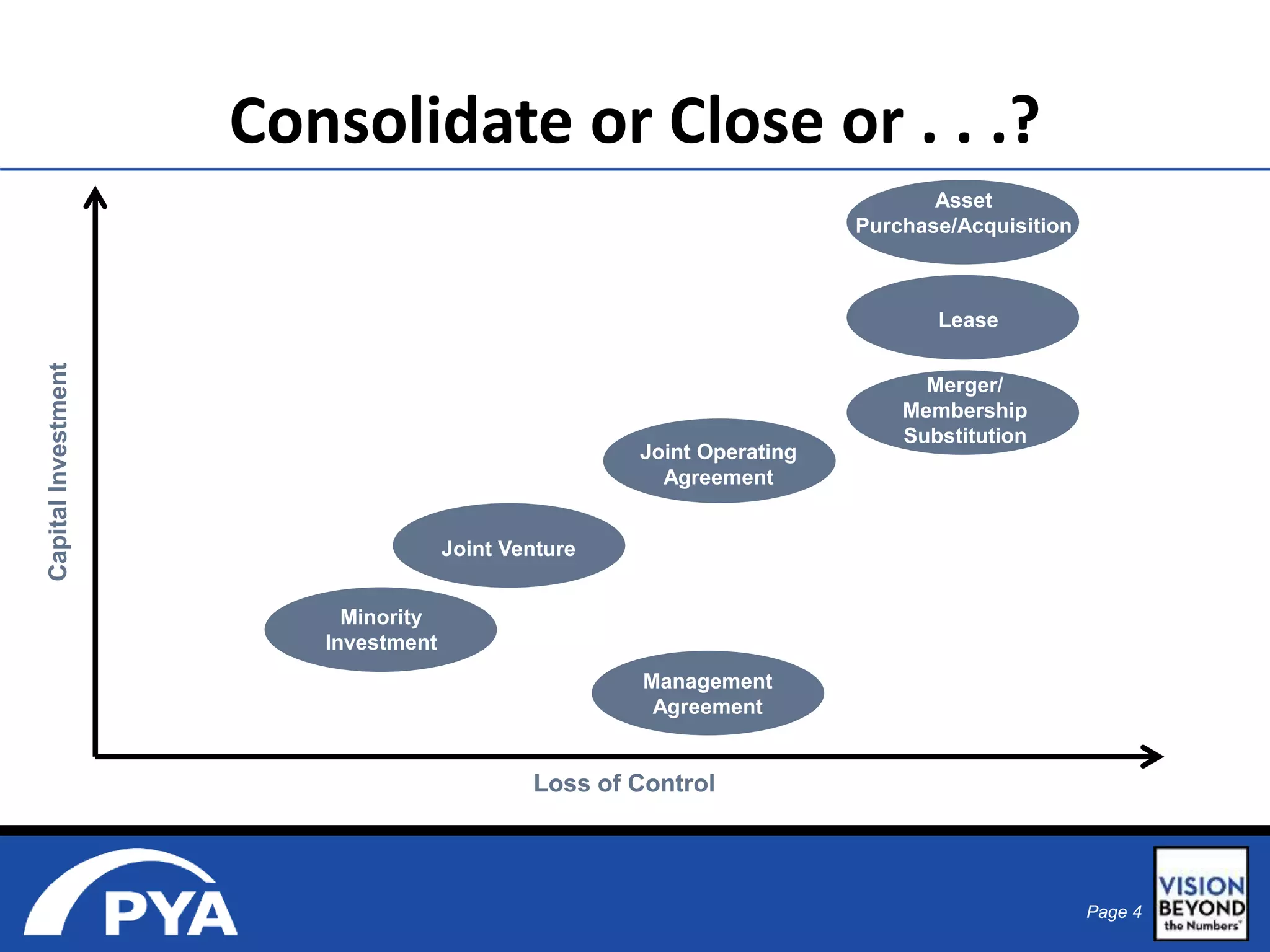
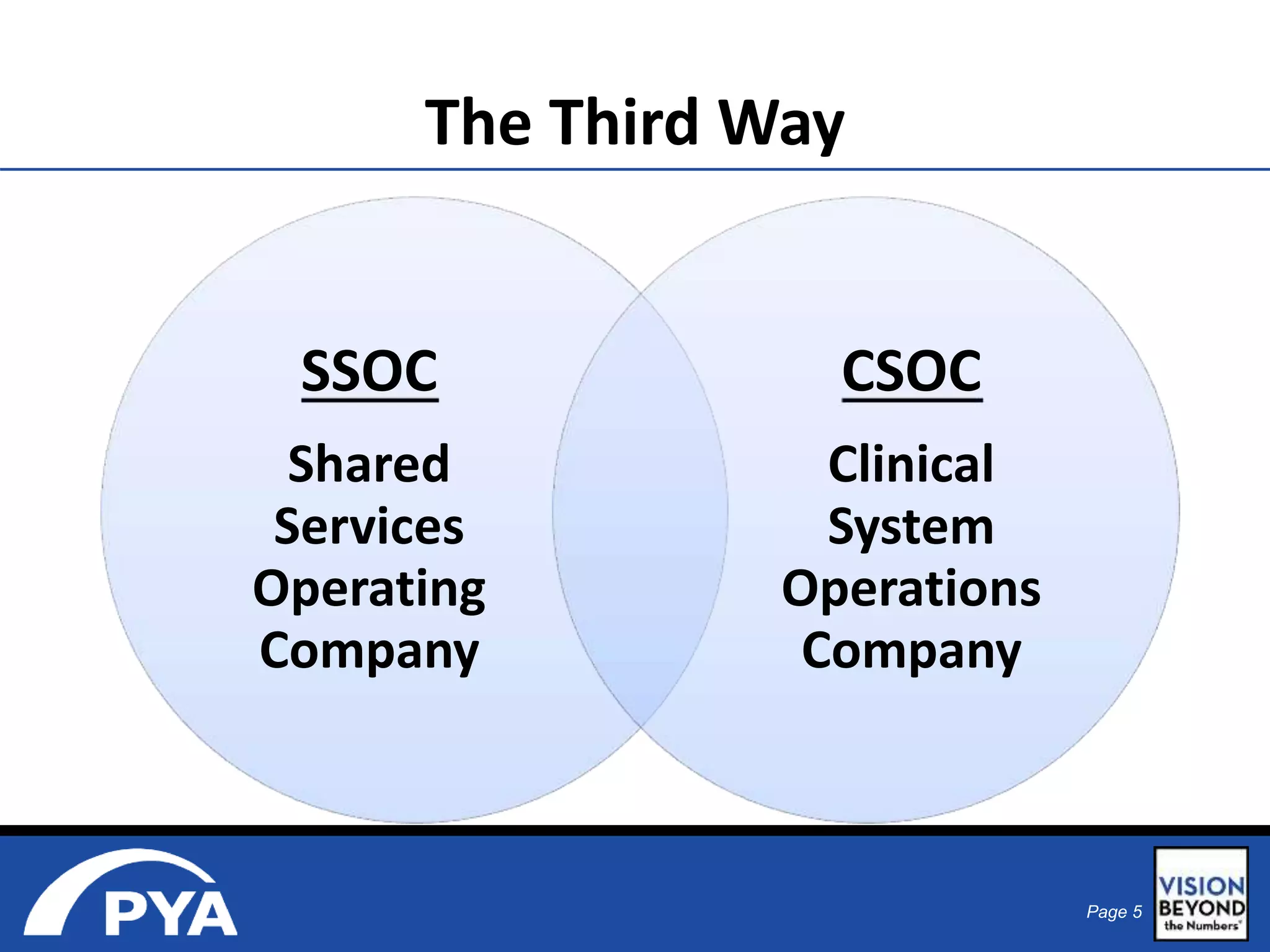
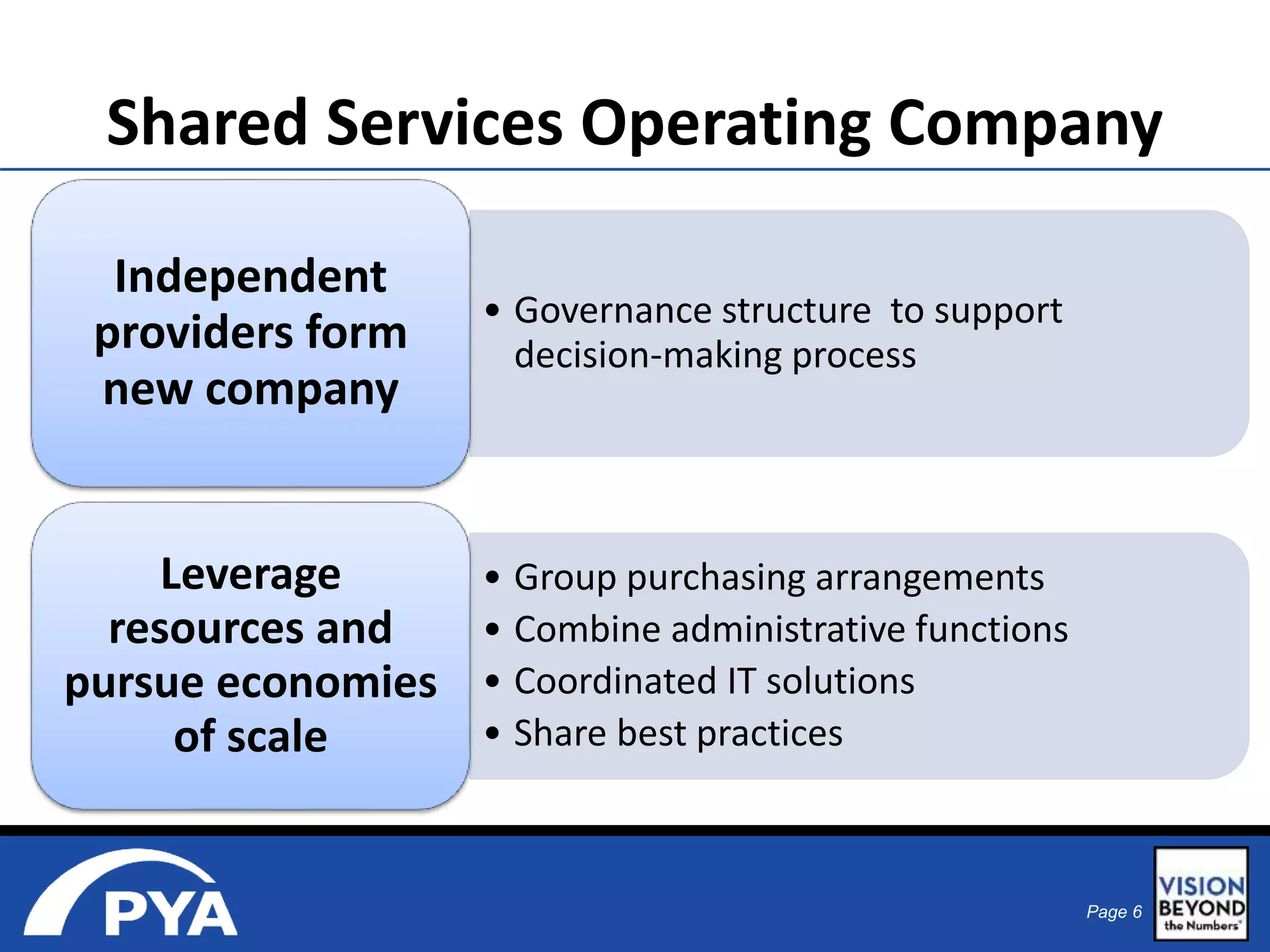
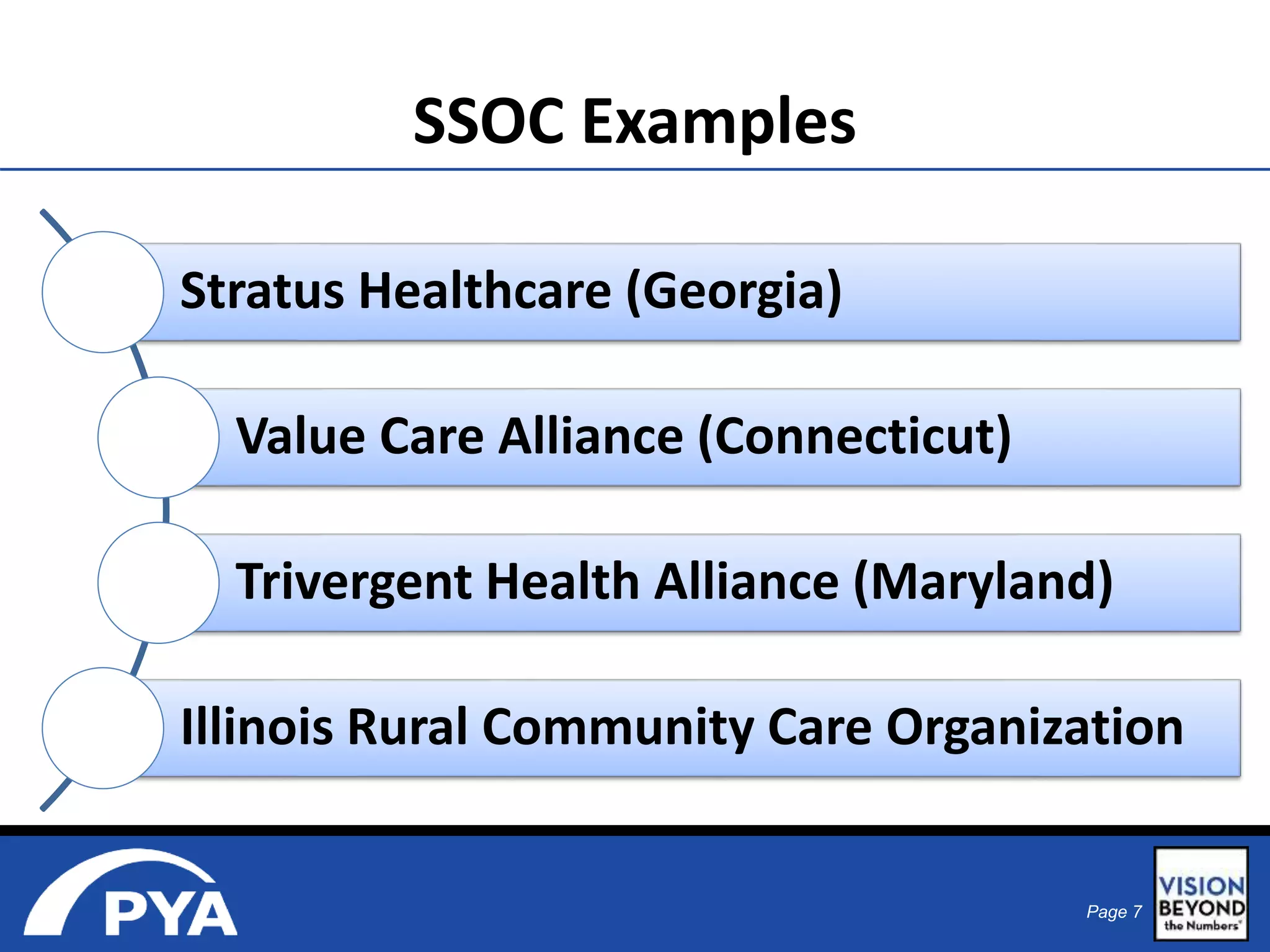
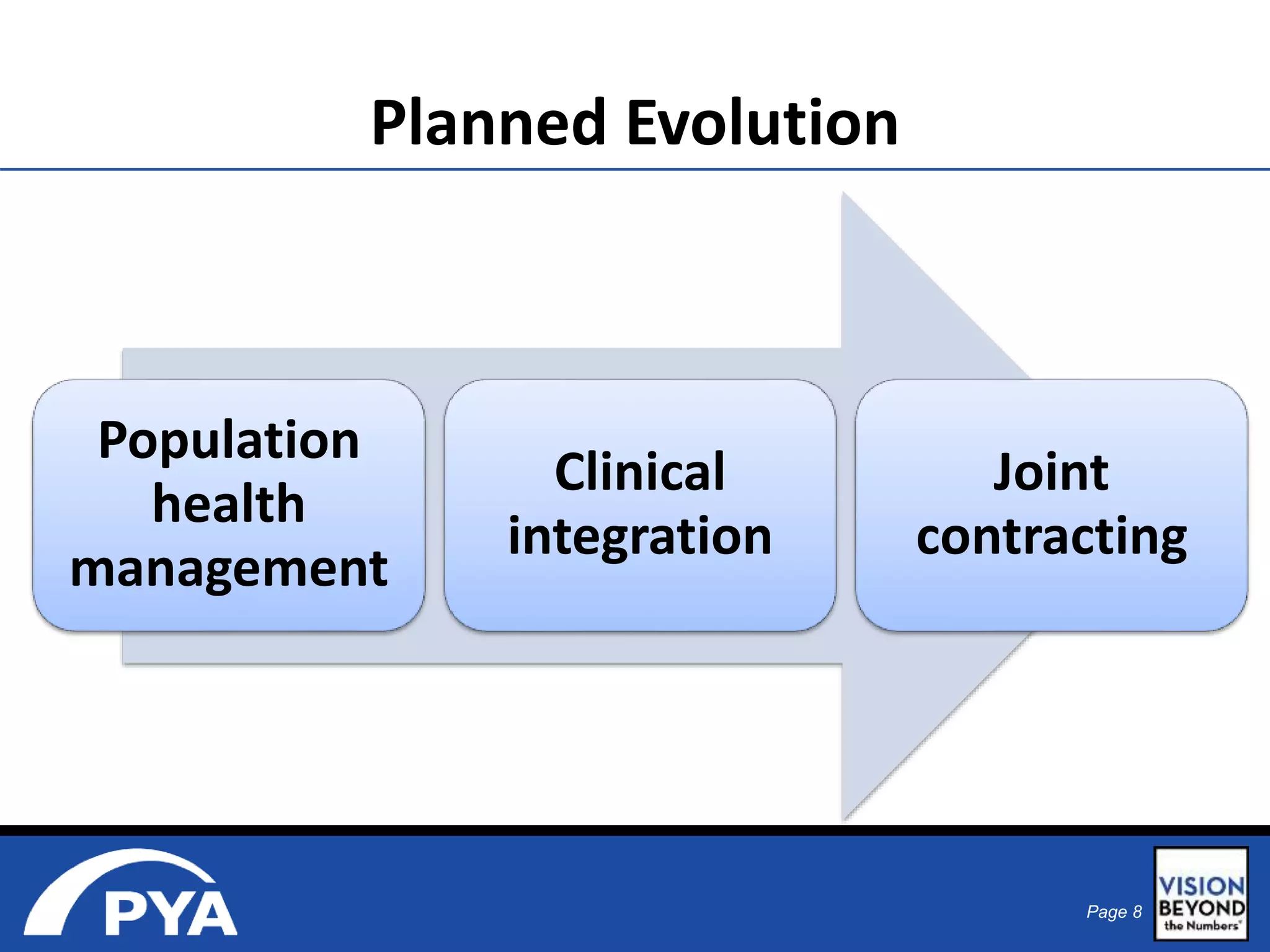
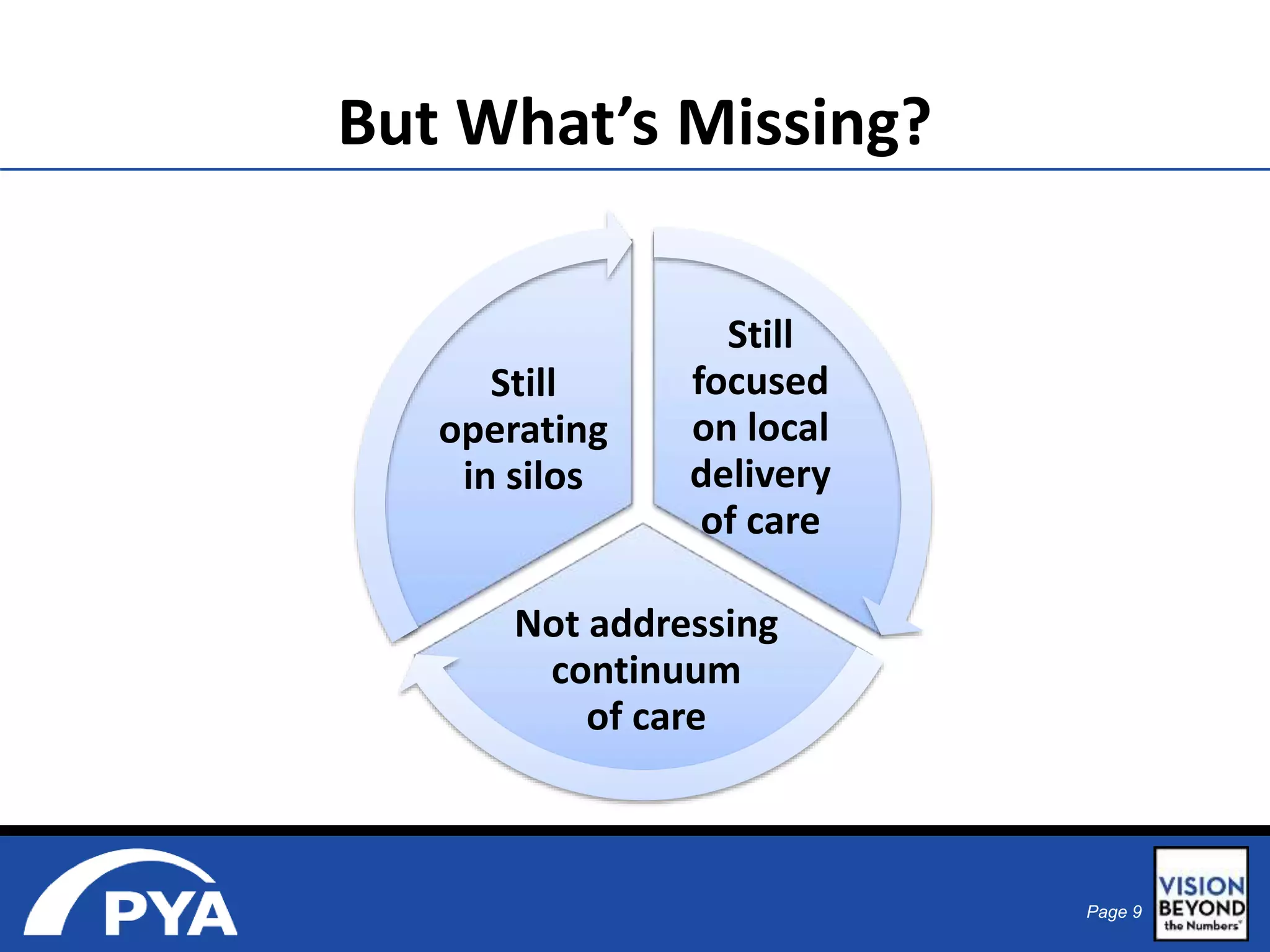
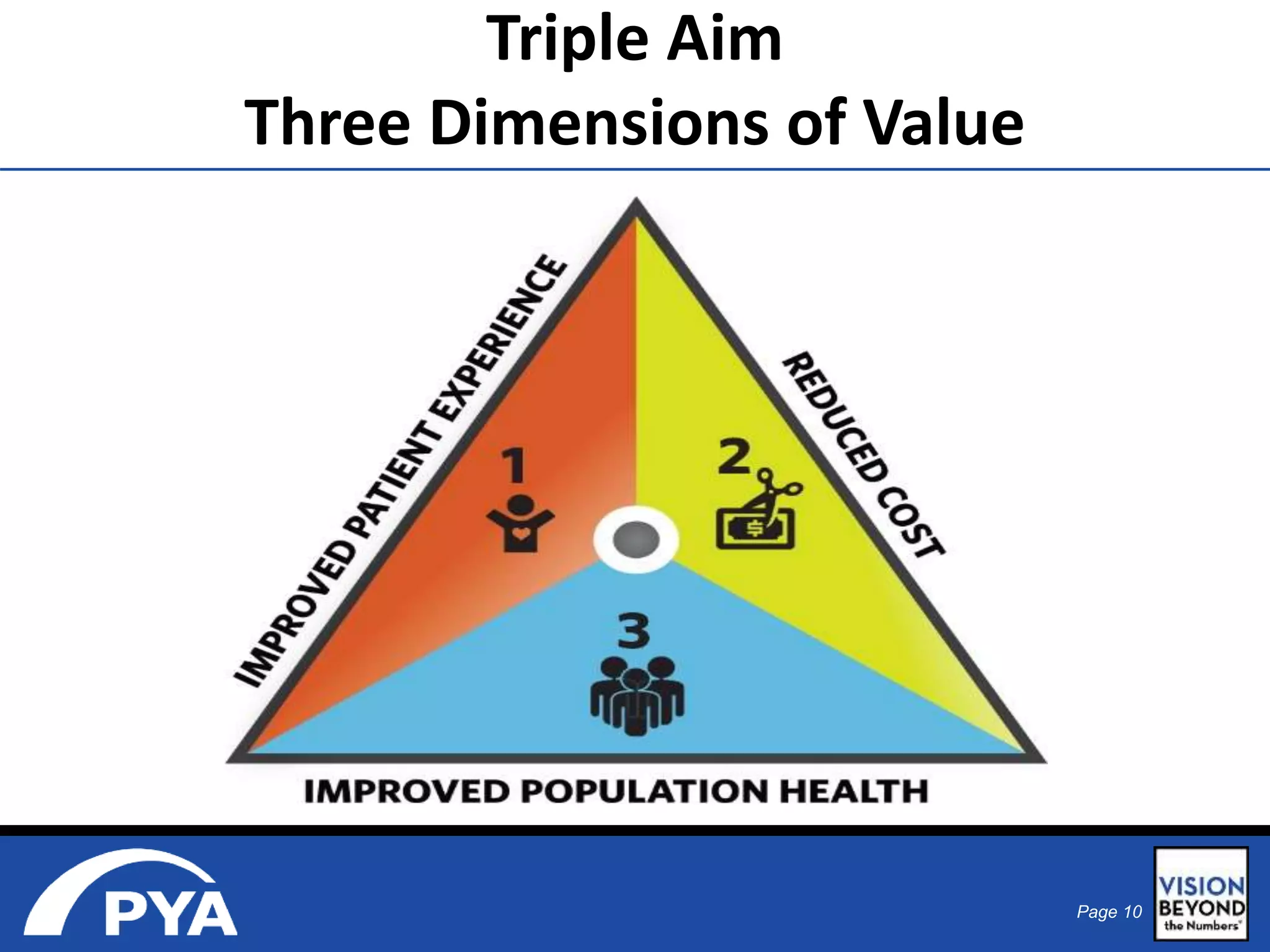
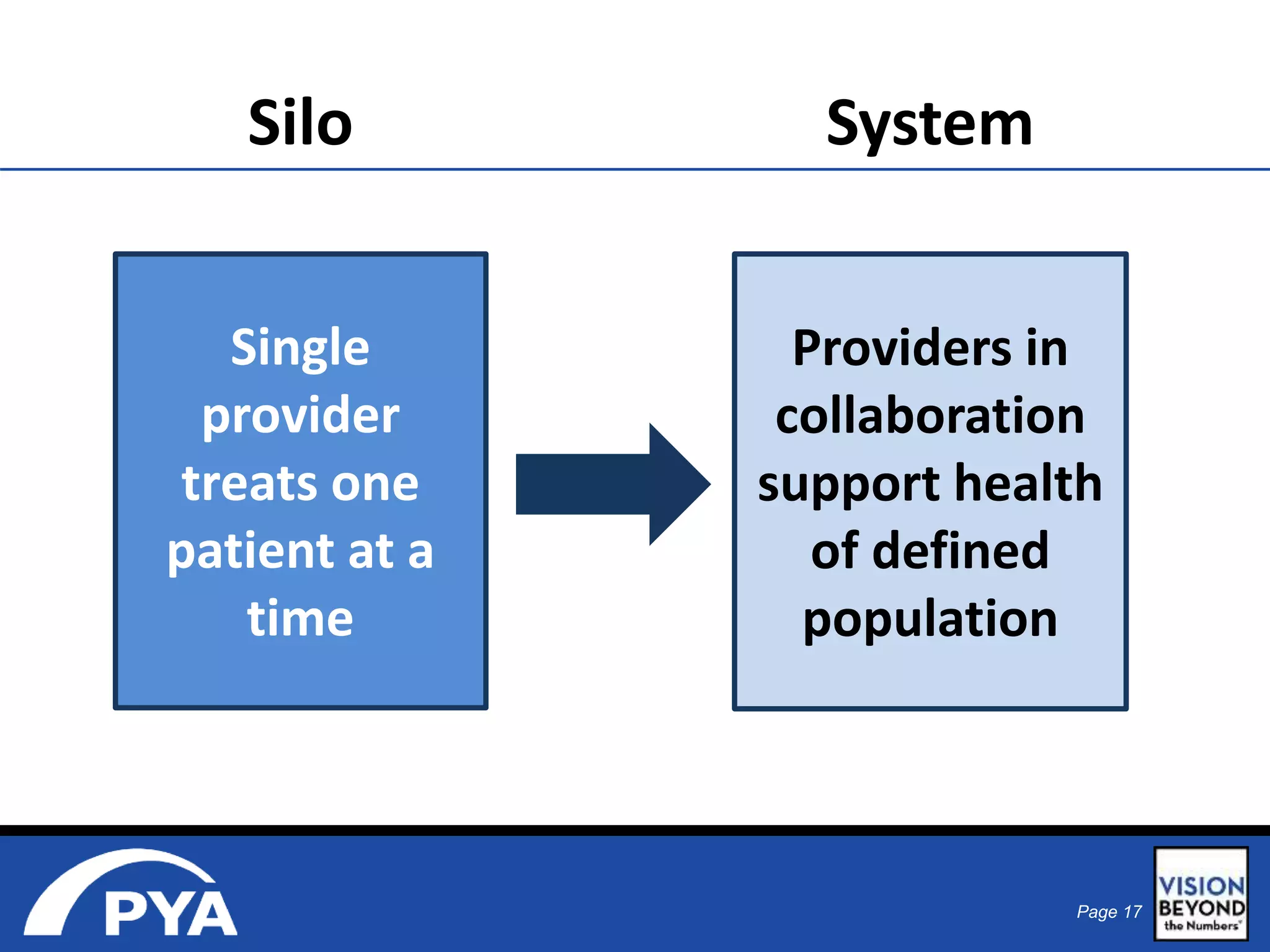
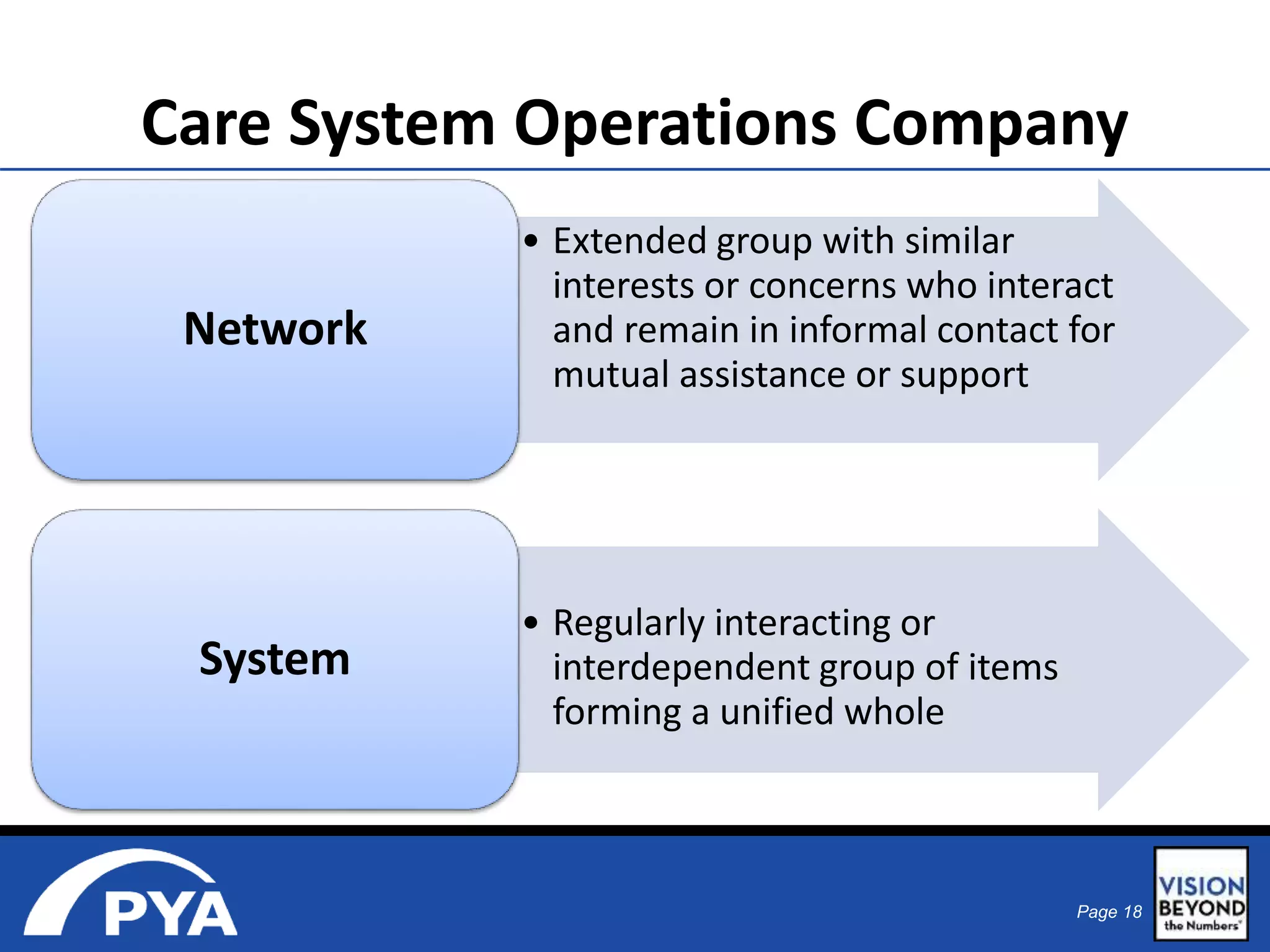
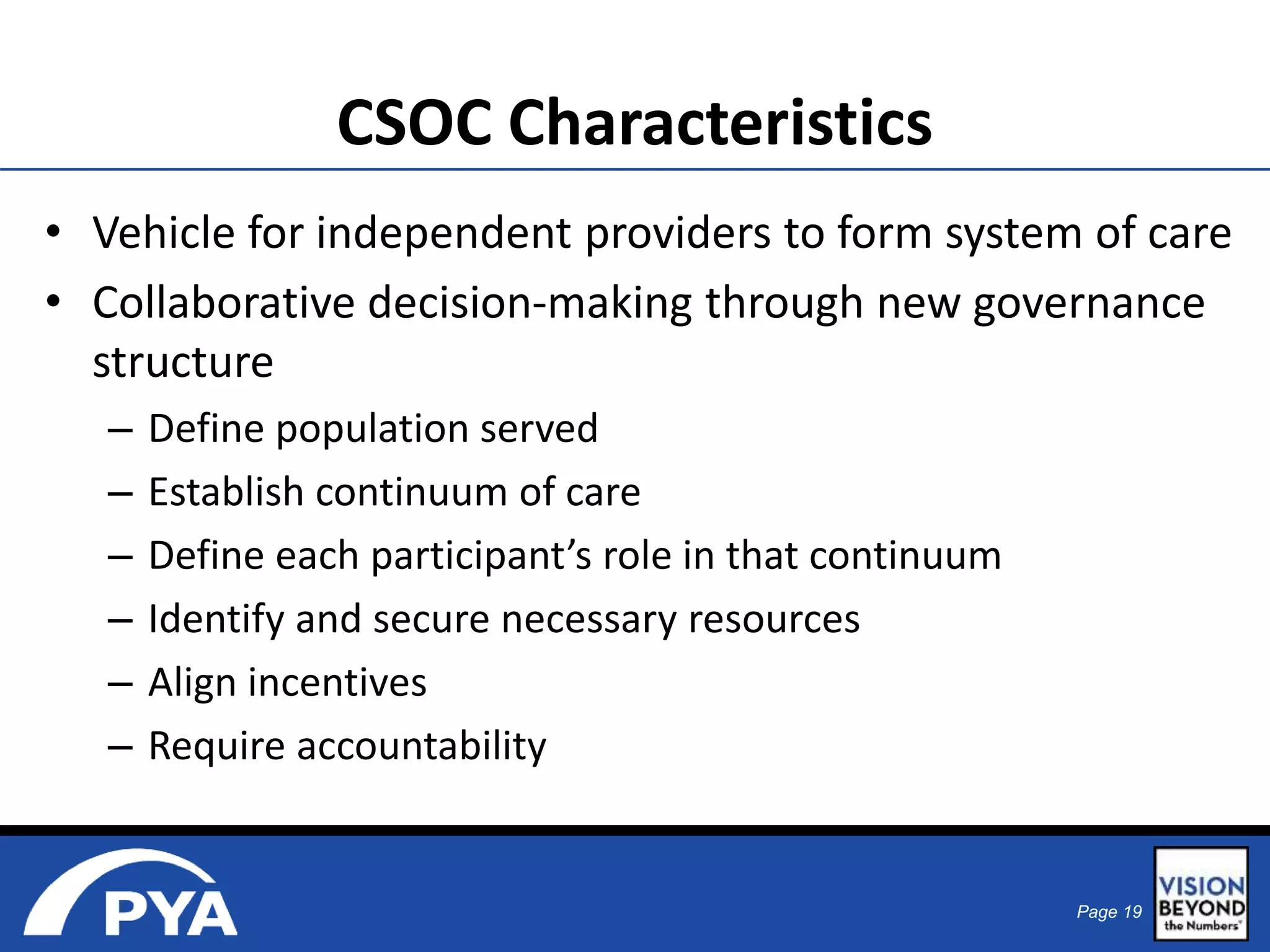
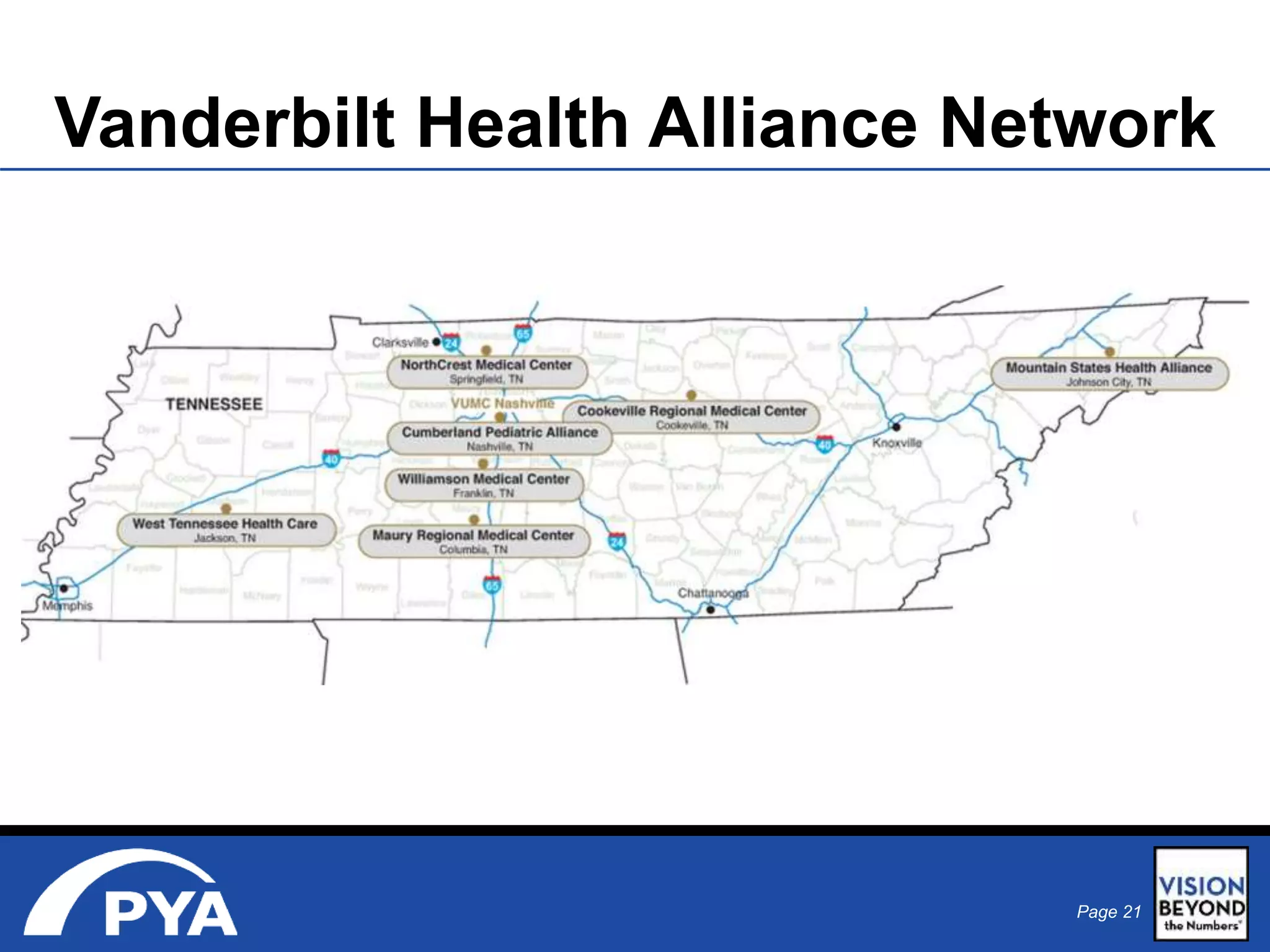
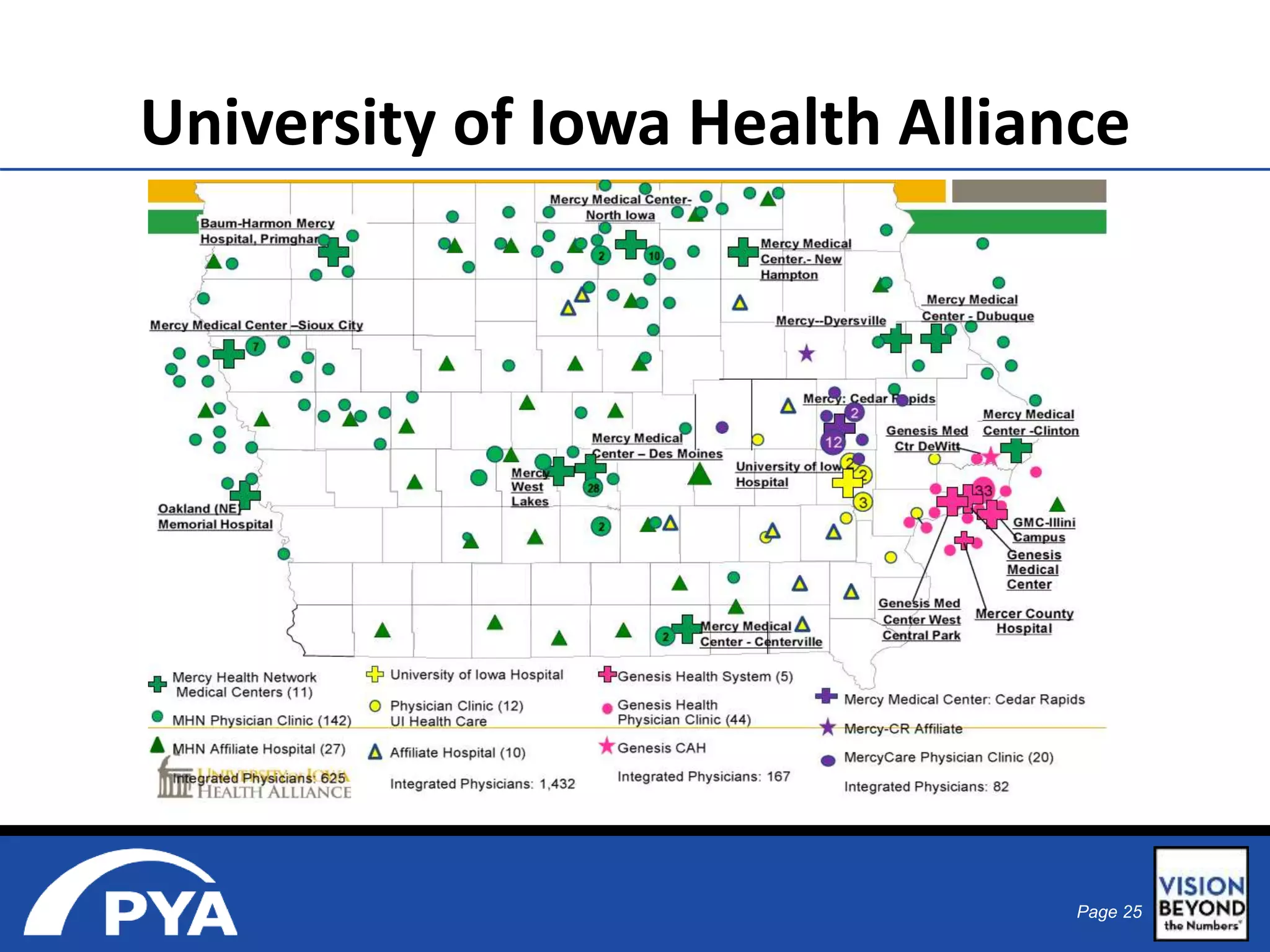
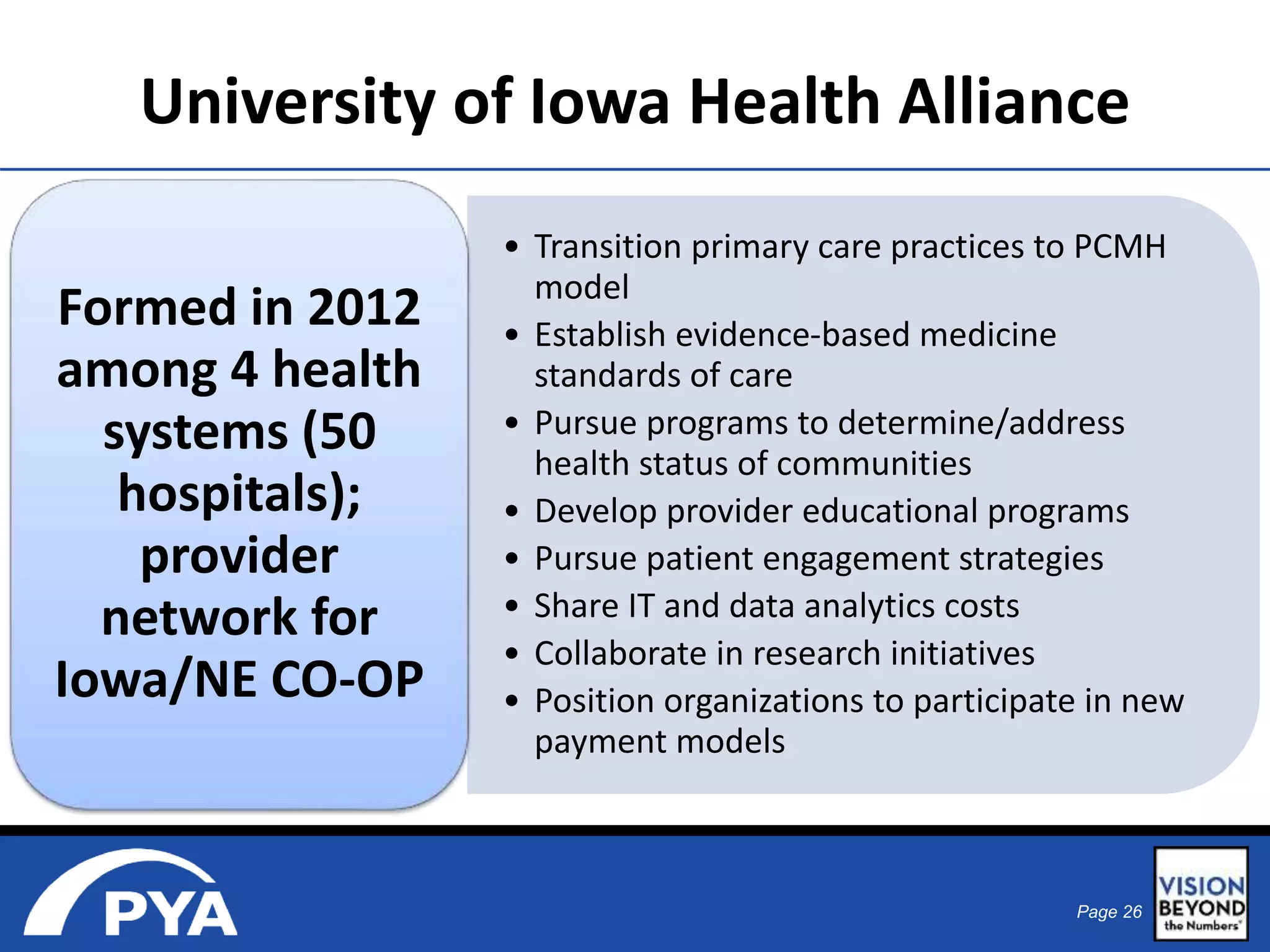
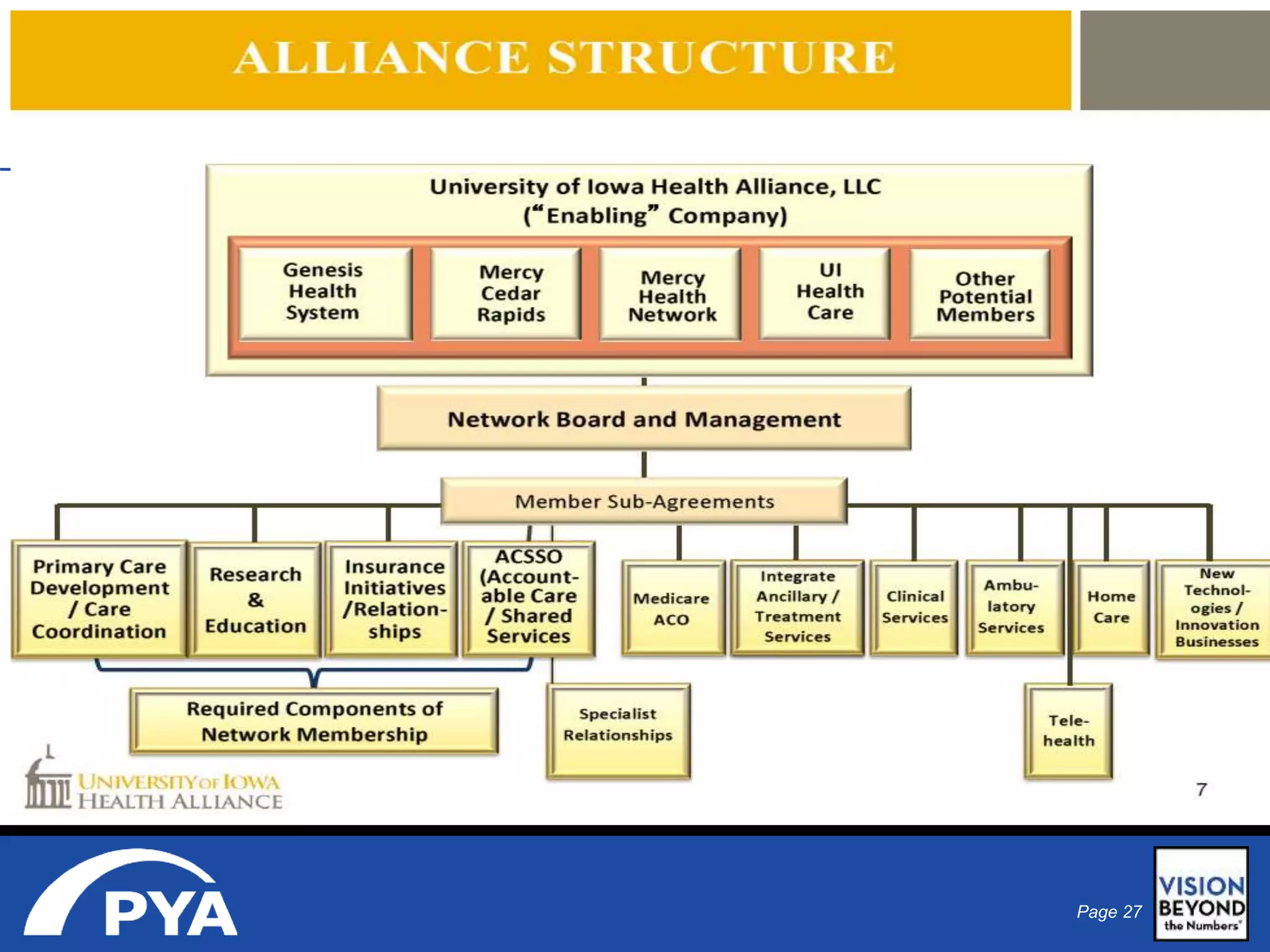
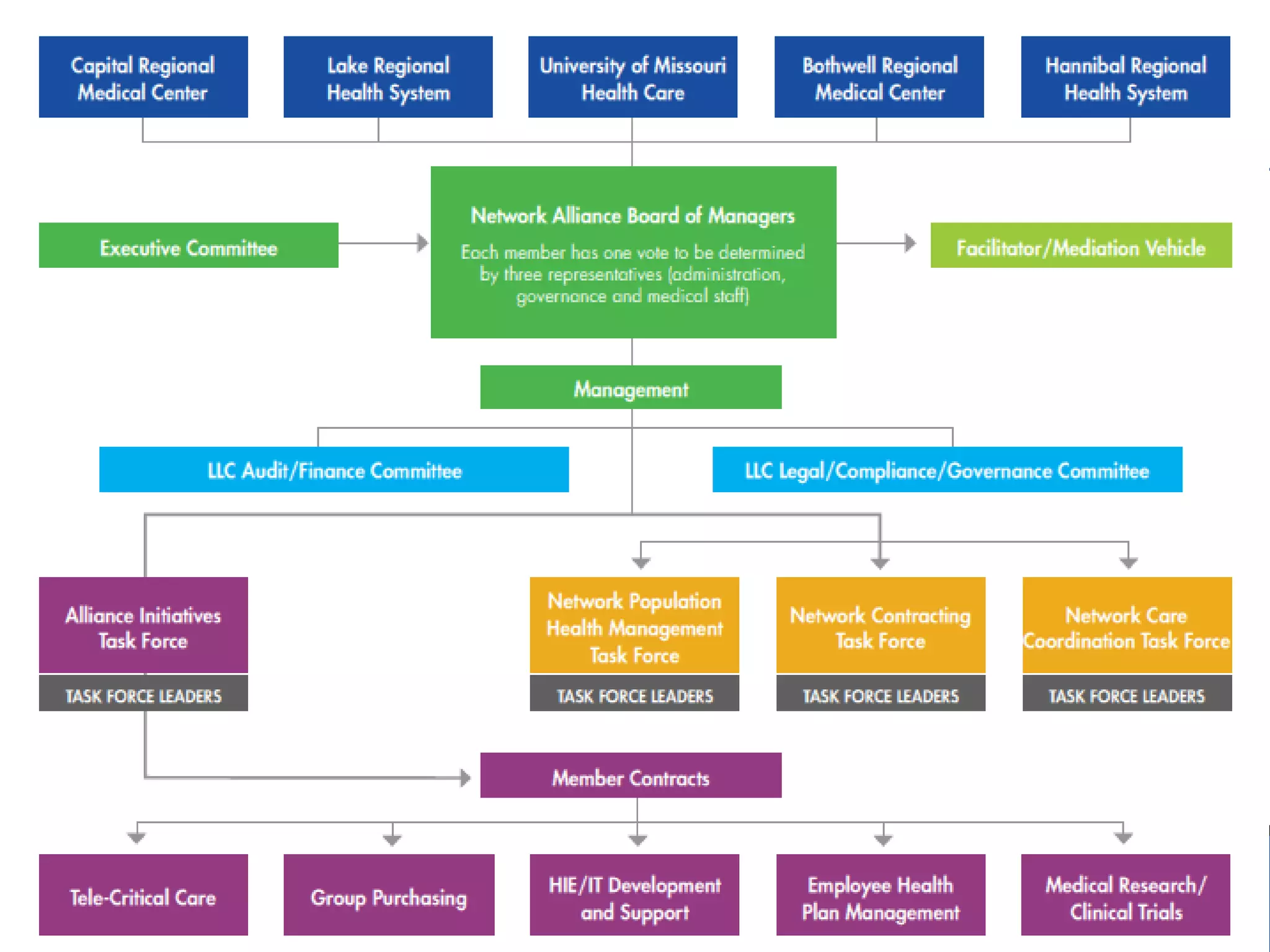
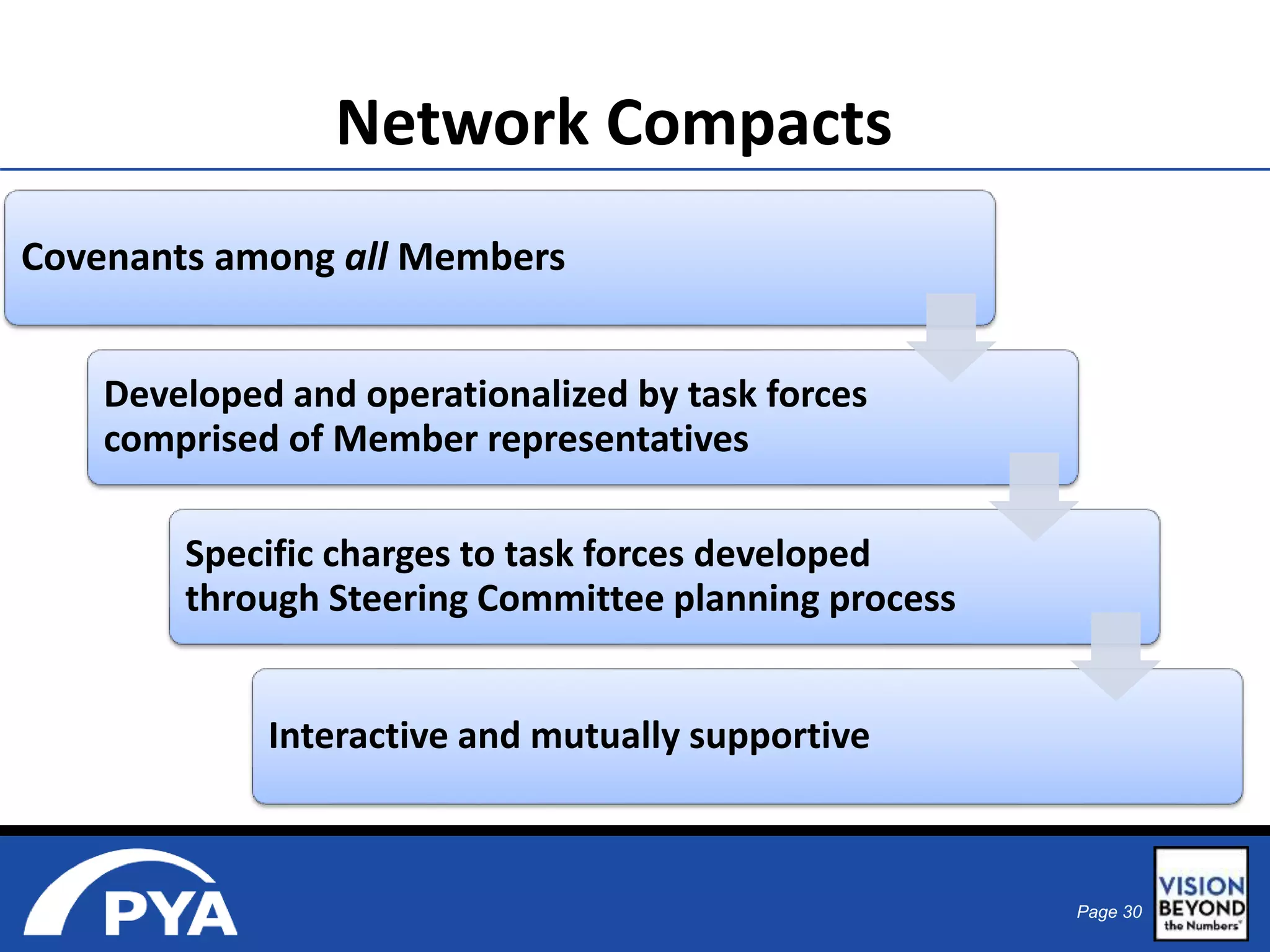
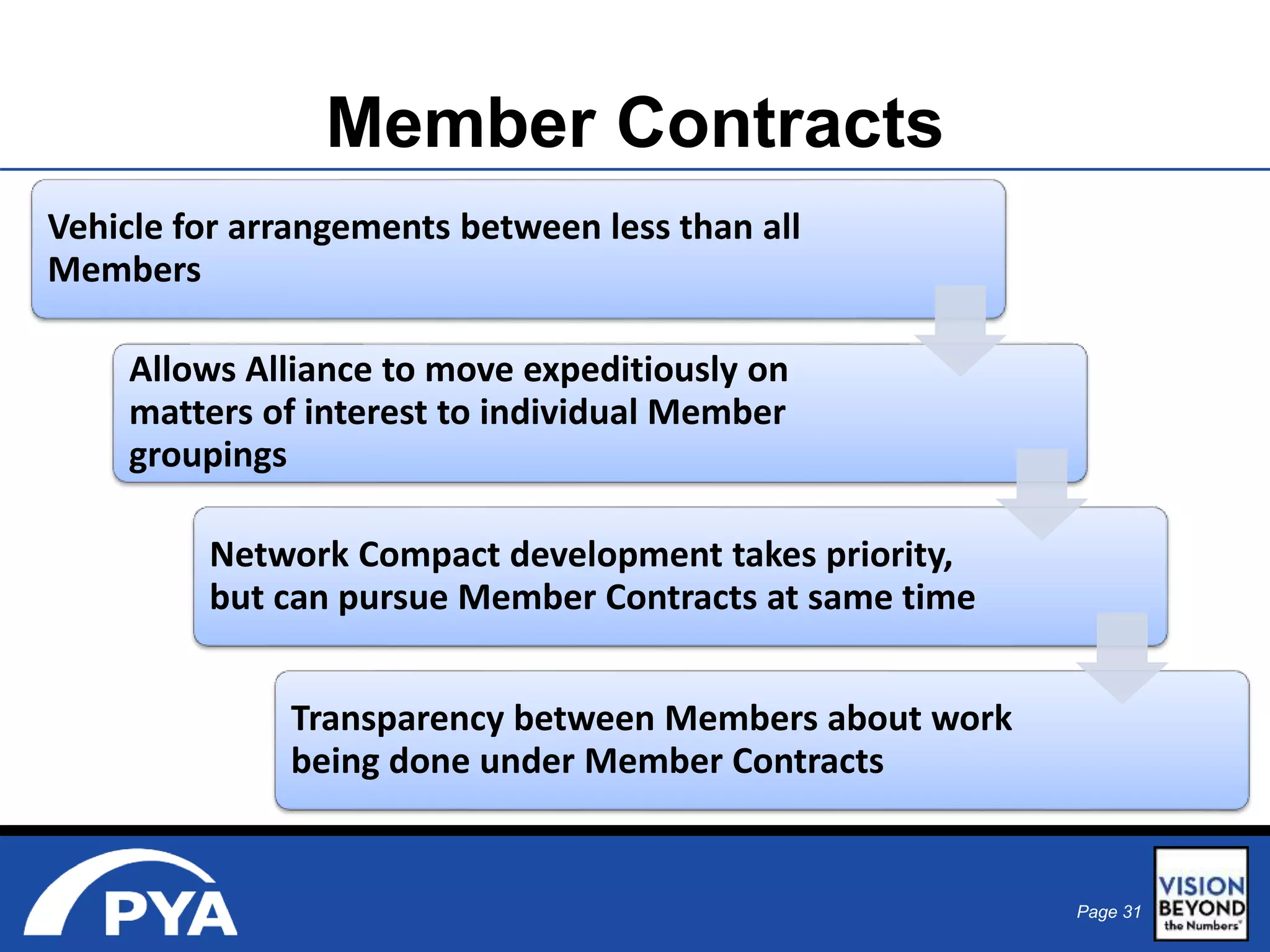
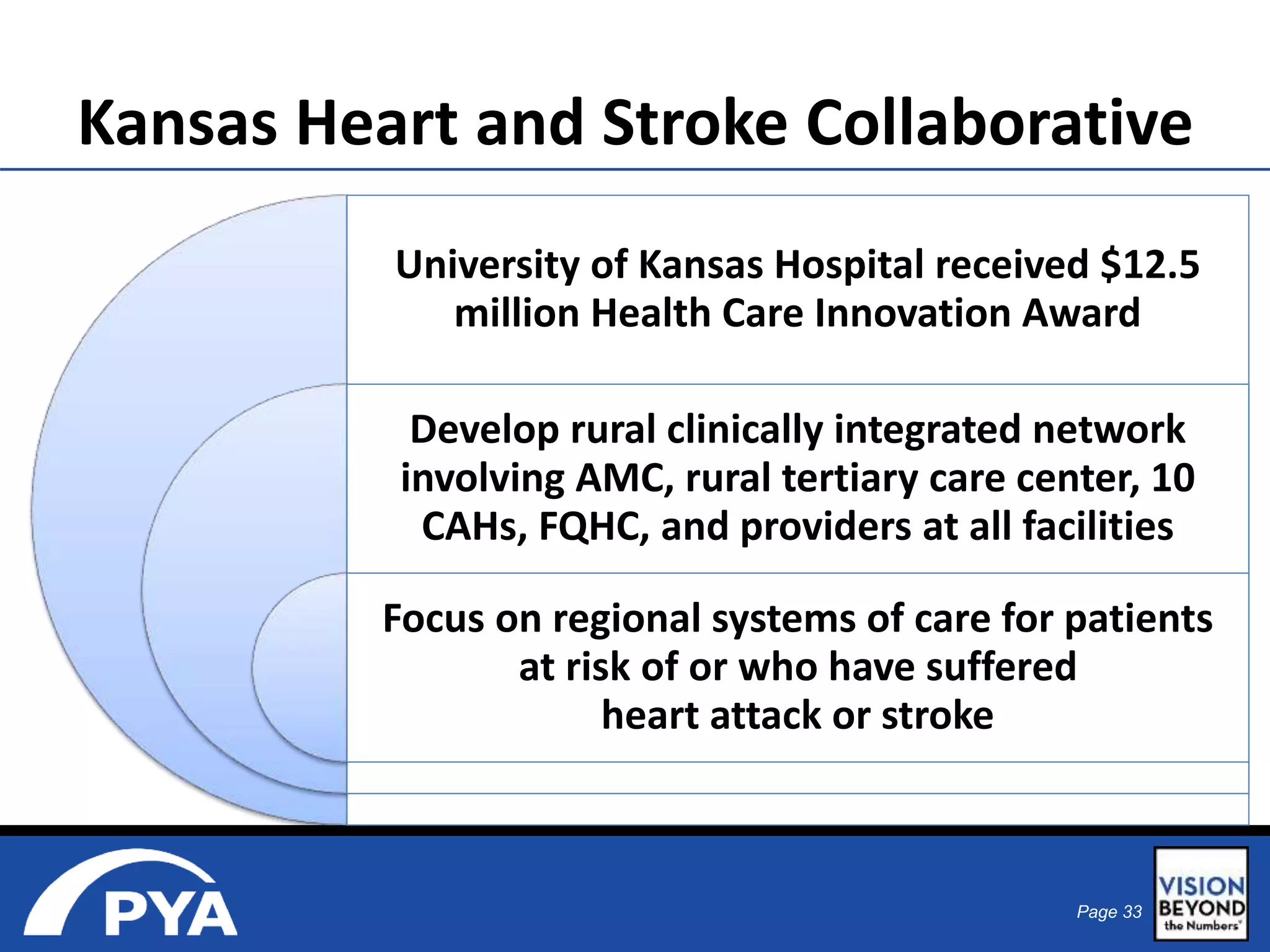
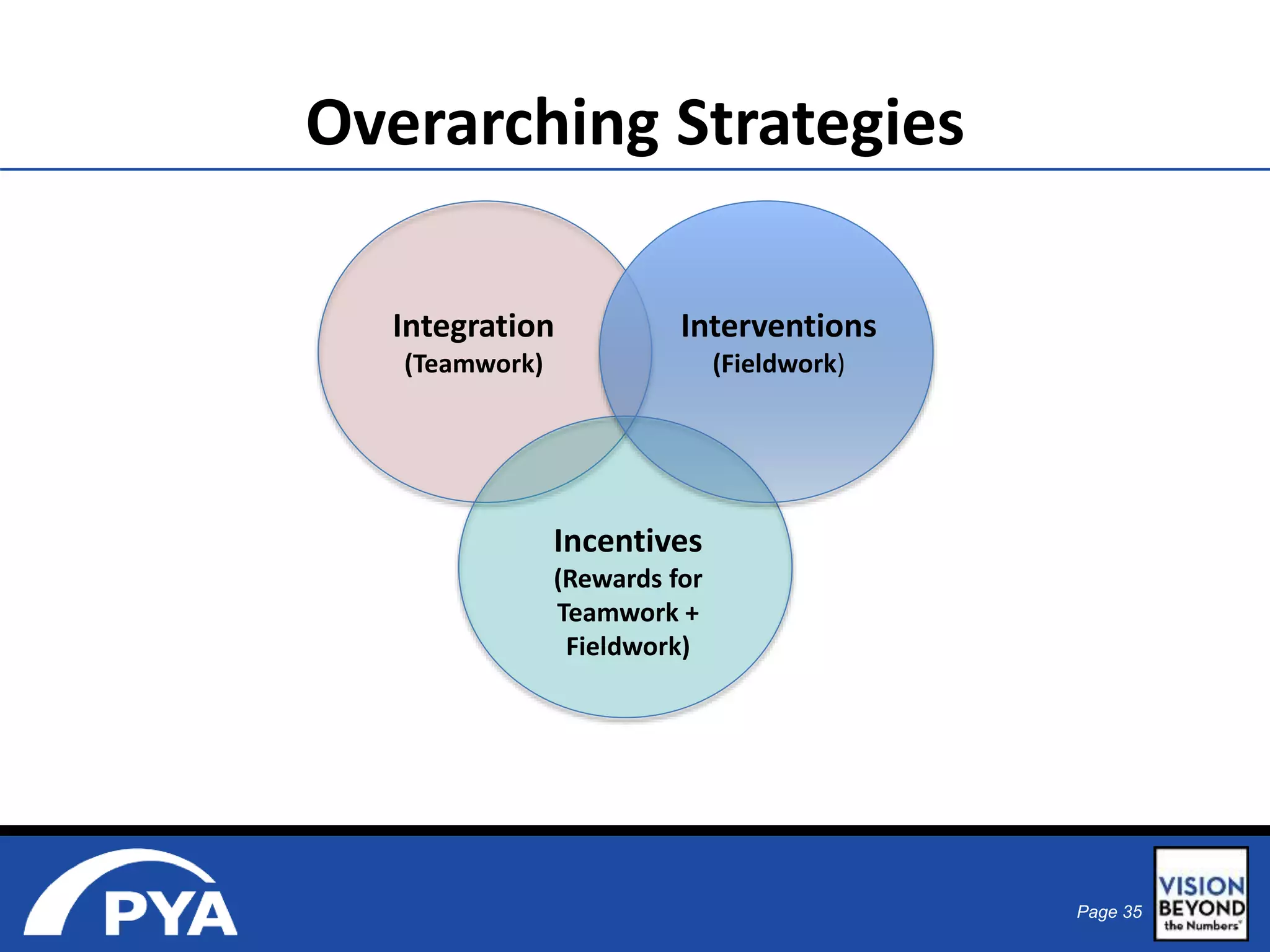
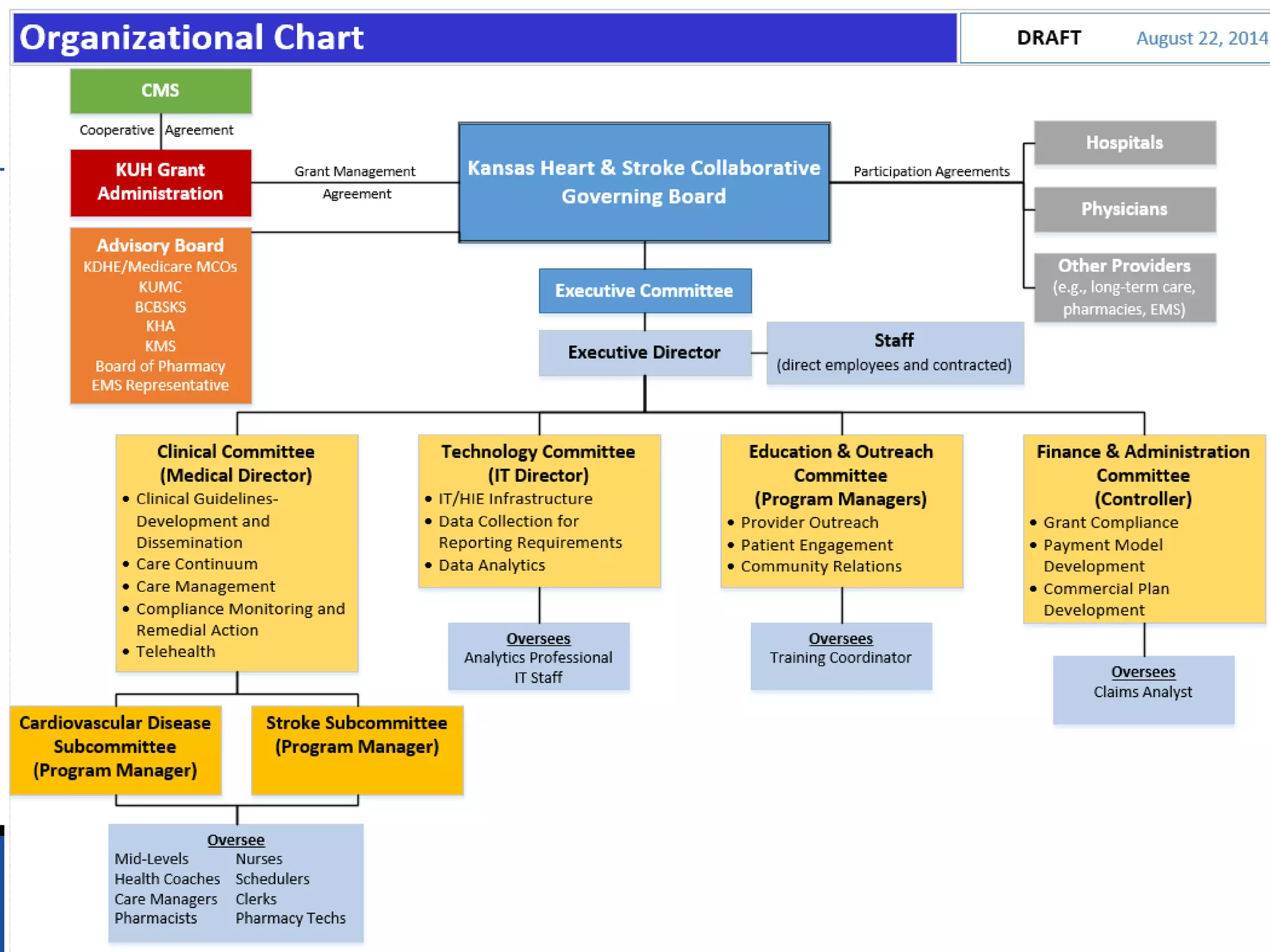
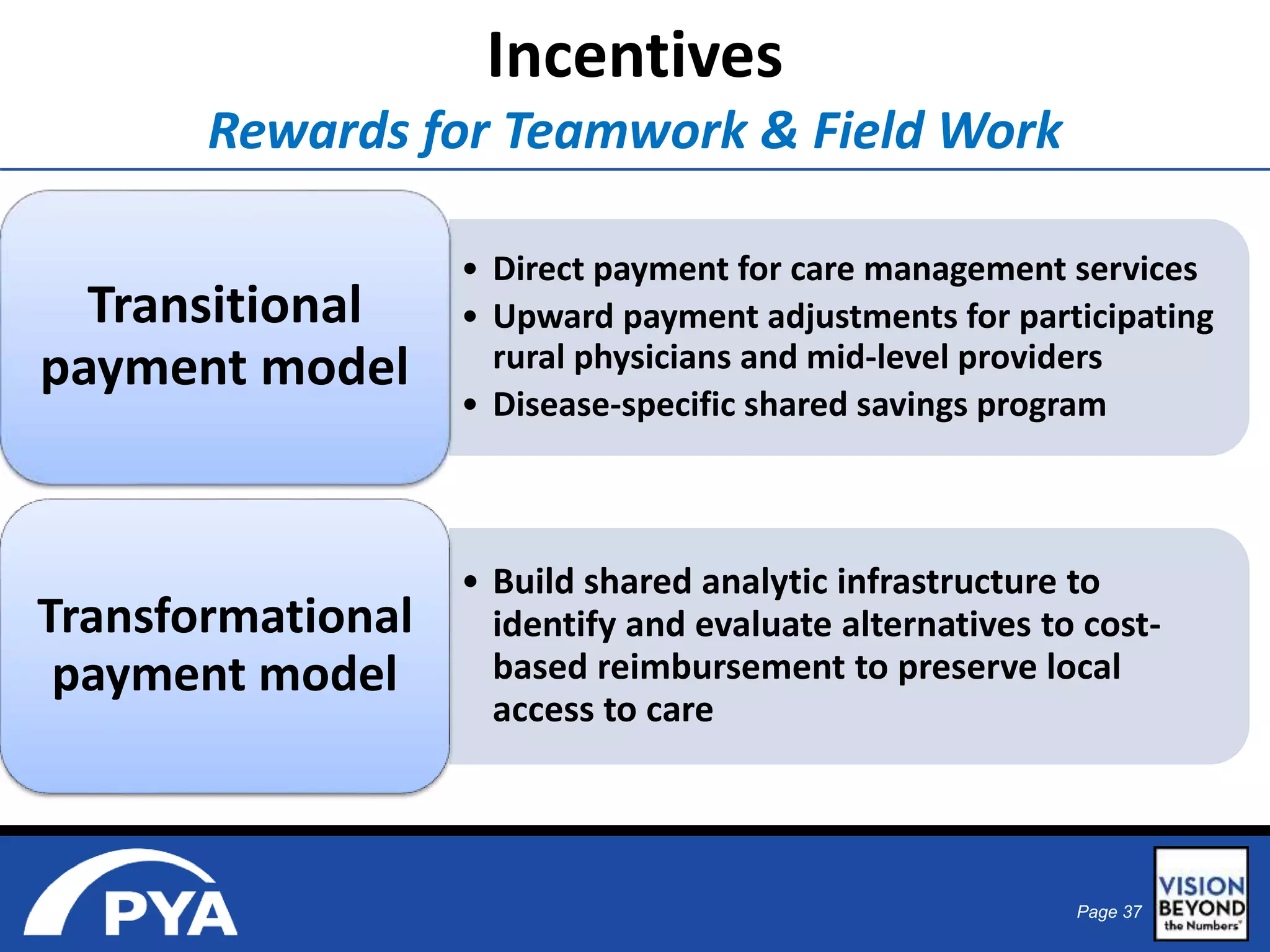
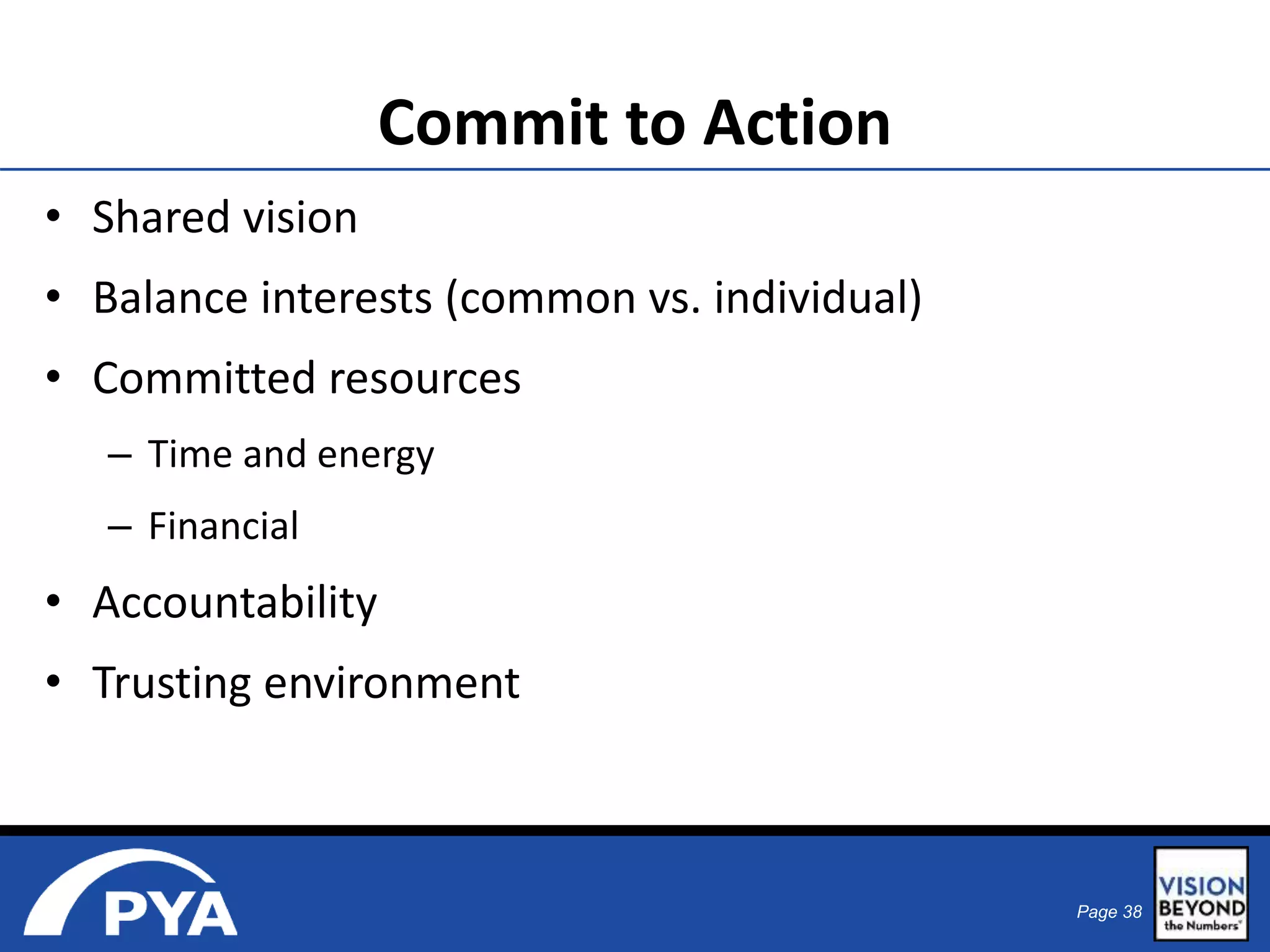
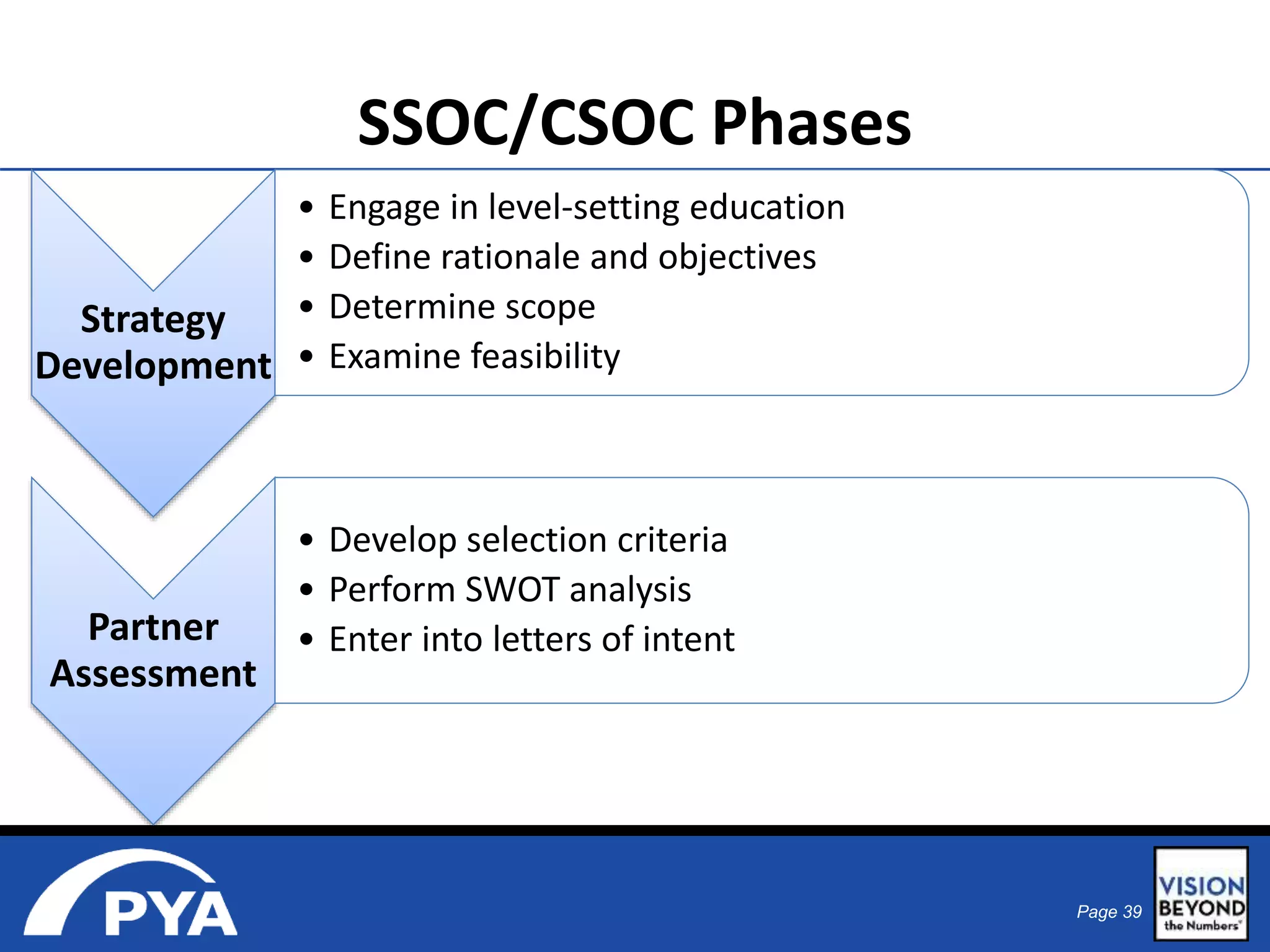
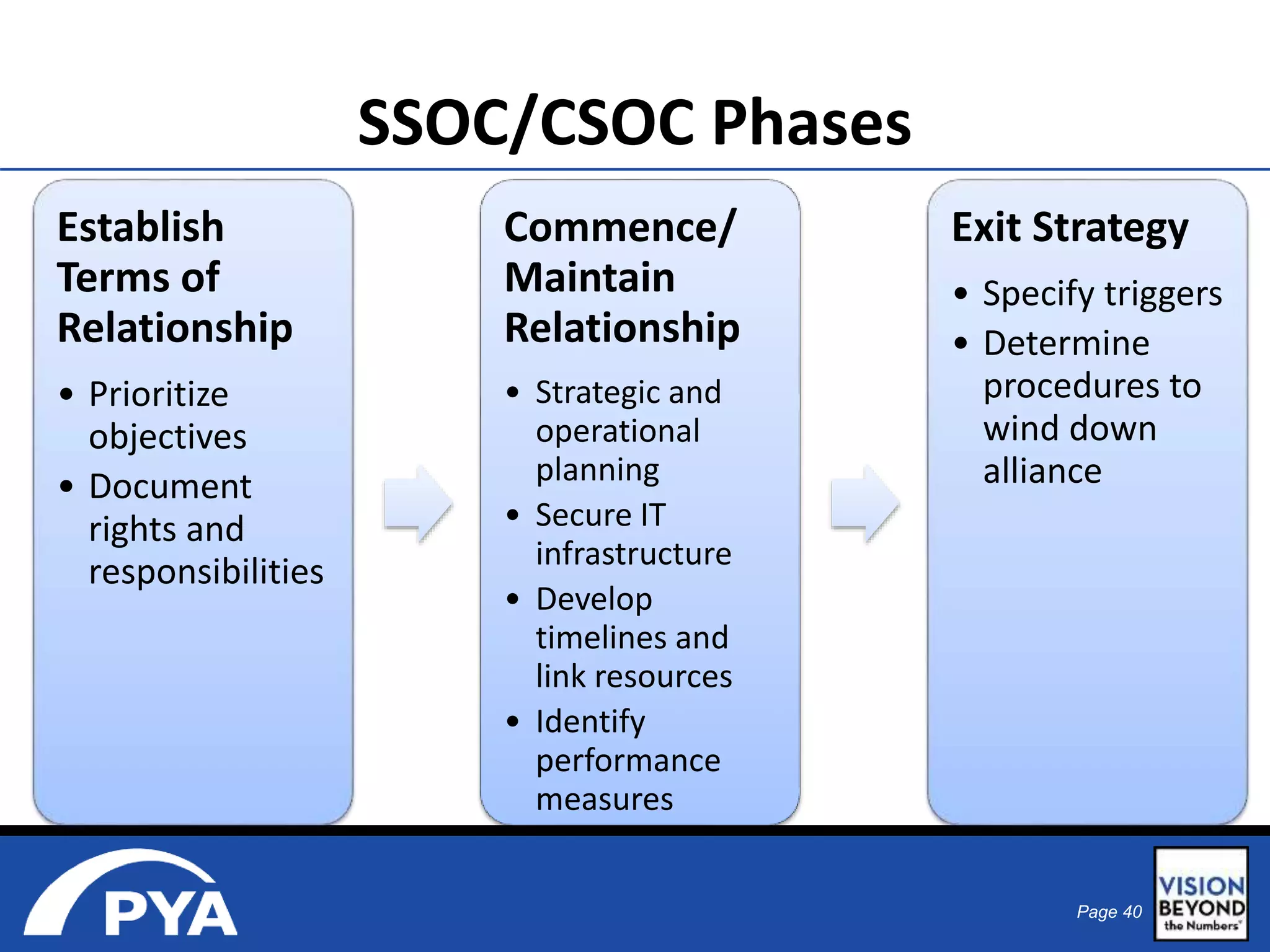
The document discusses strategies for improving rural healthcare through interdependence among independent providers, highlighting shared services and collaborative governance structures to enhance care delivery and population health management. It emphasizes the need for new payment models and integration of services to address the challenges faced by rural communities, such as higher healthcare costs and poorer health outcomes. Various examples of collaborative networks and initiatives are presented, showcasing the importance of collective action in achieving better healthcare solutions.