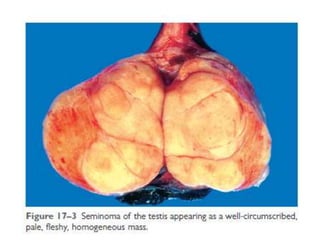
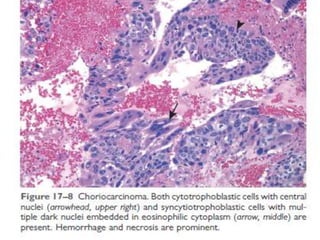
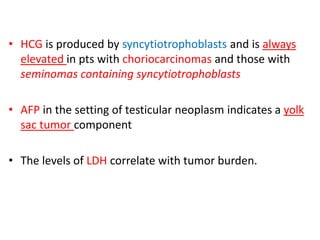
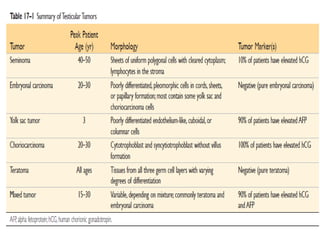
This document discusses cryptorchidism, testicular torsion, and testicular neoplasms. Cryptorchidism is the failure of one or both testes to descend into the scrotum. It affects 1% of males and increases the risk of testicular cancer and infertility. Testicular torsion occurs when the spermatic cord twists, cutting off blood flow to the testis. It requires urgent surgery to untwist the cord. Testicular tumors are most often painless enlargements of the testis. Seminomas and non-seminomatous germ cell tumors are the main types and differ in aggressiveness and spread. Treatment involves surgery and chemotherapy with good cure rates.