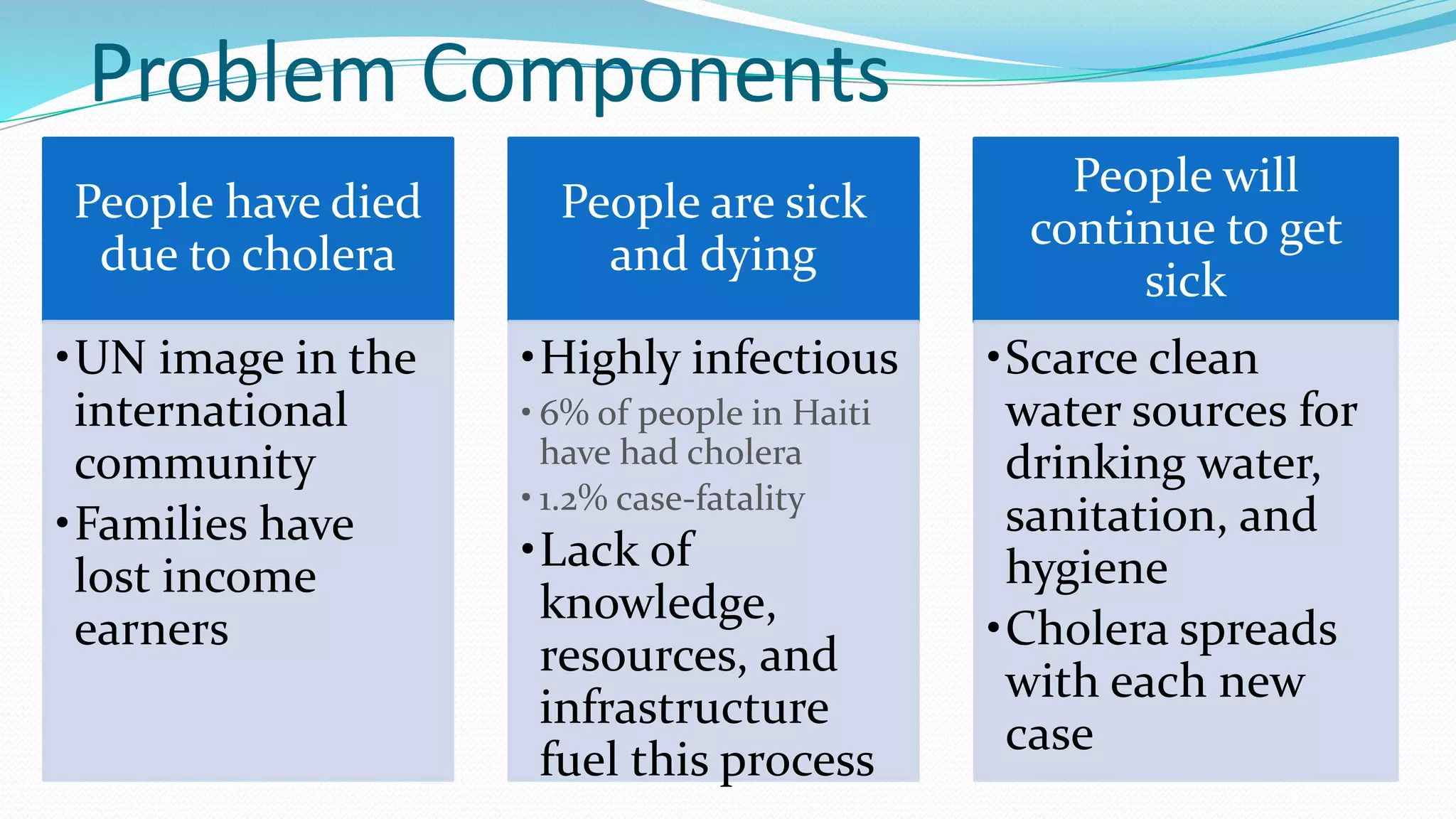
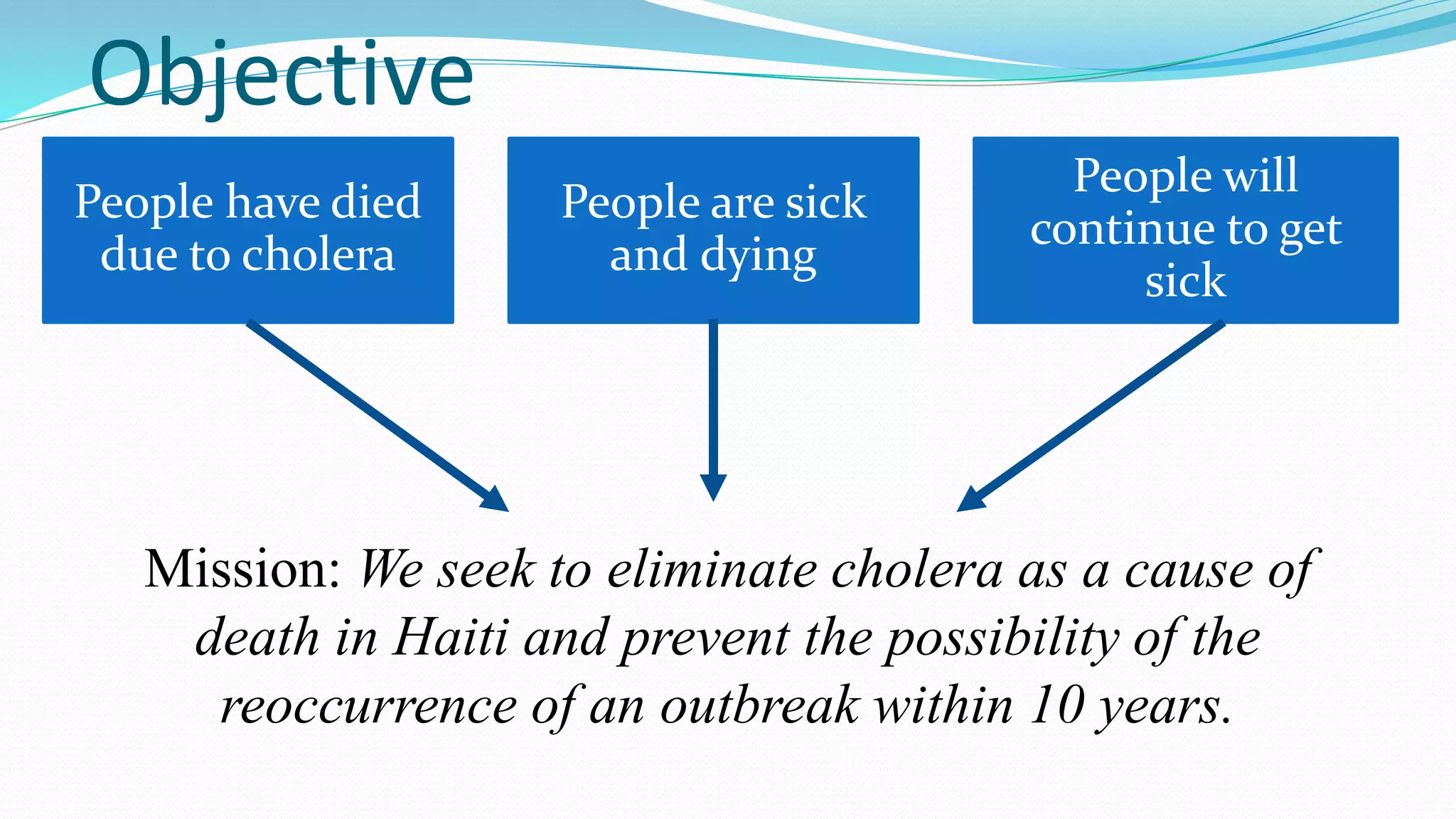
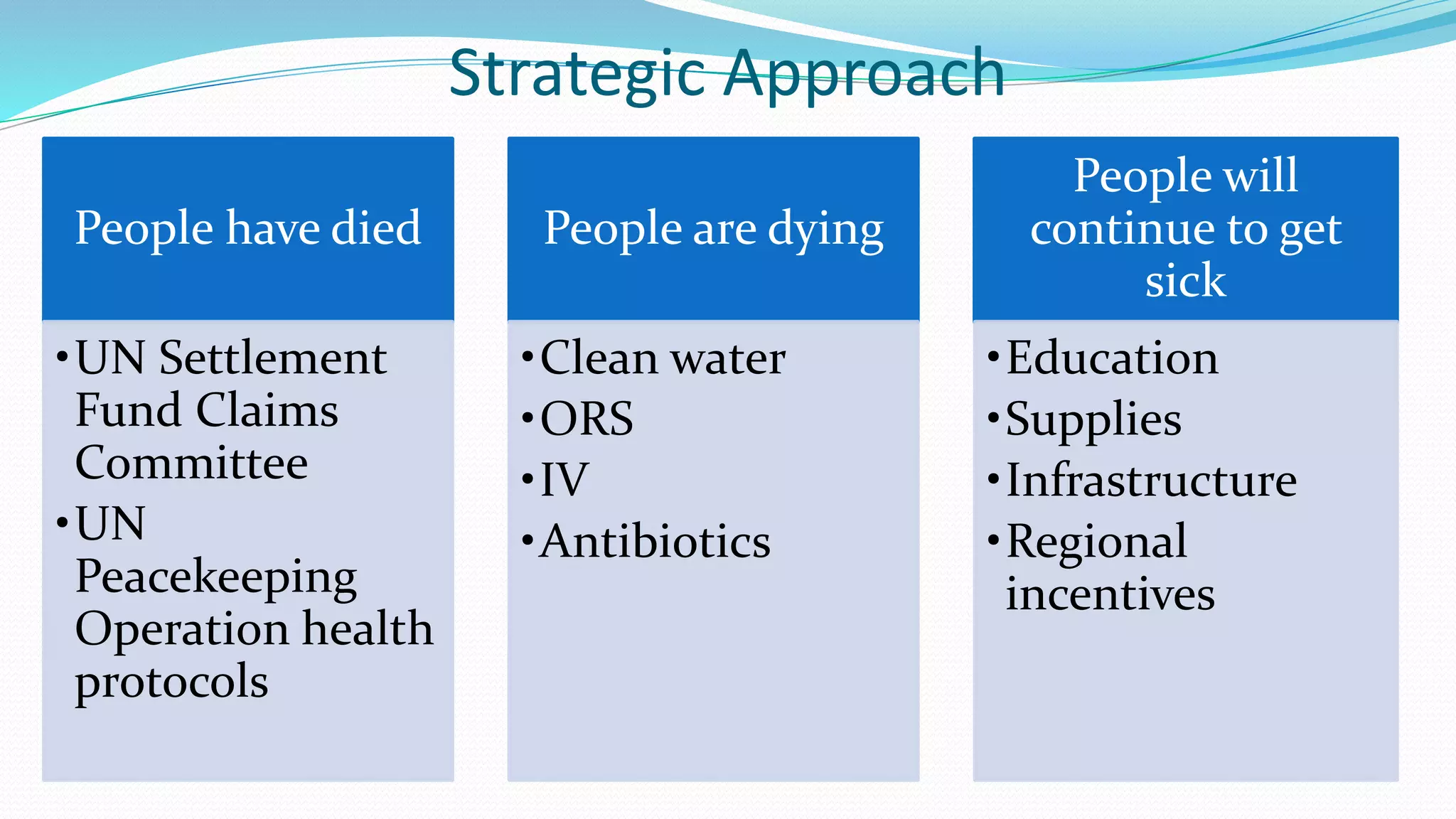
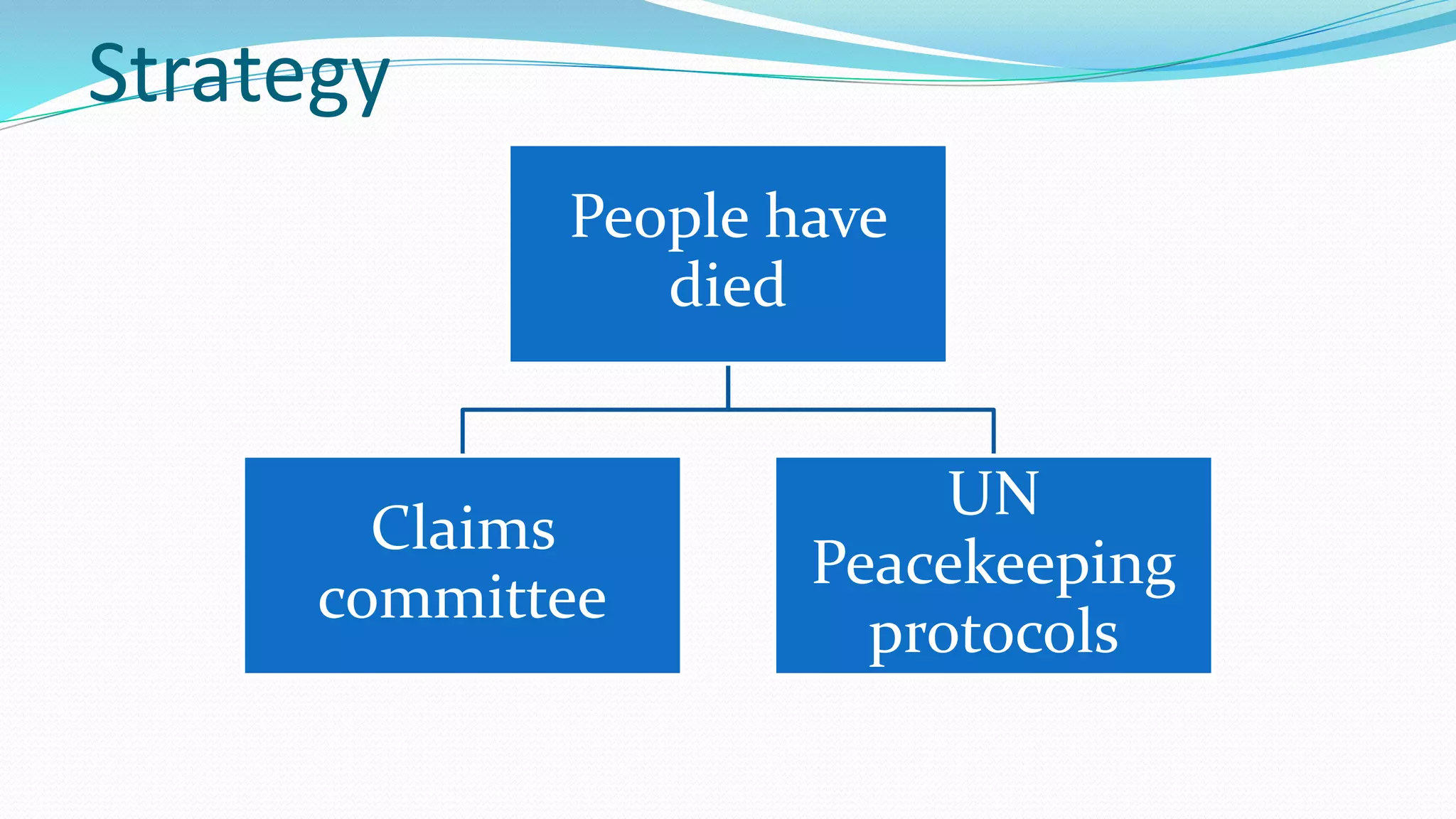
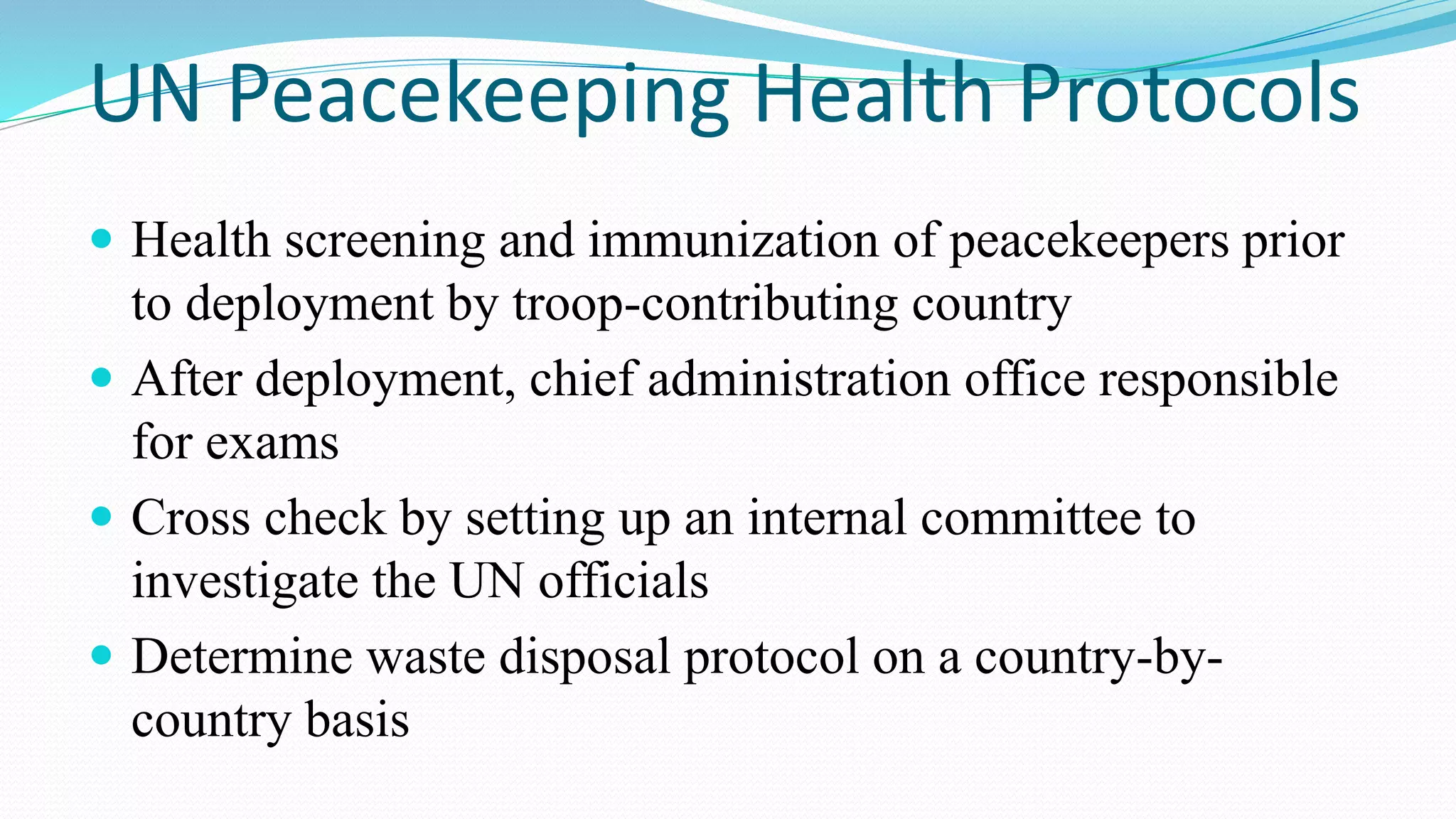
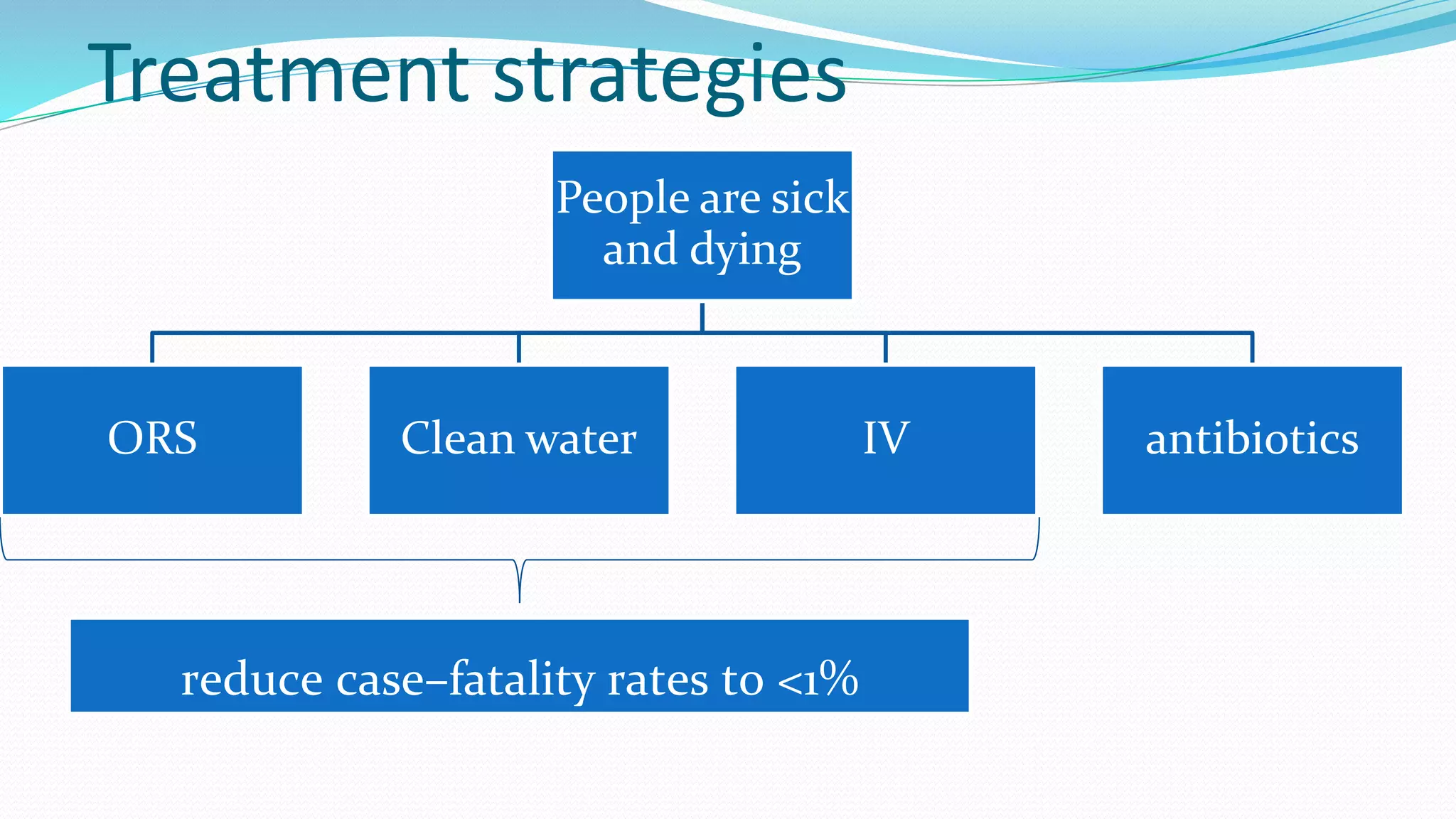
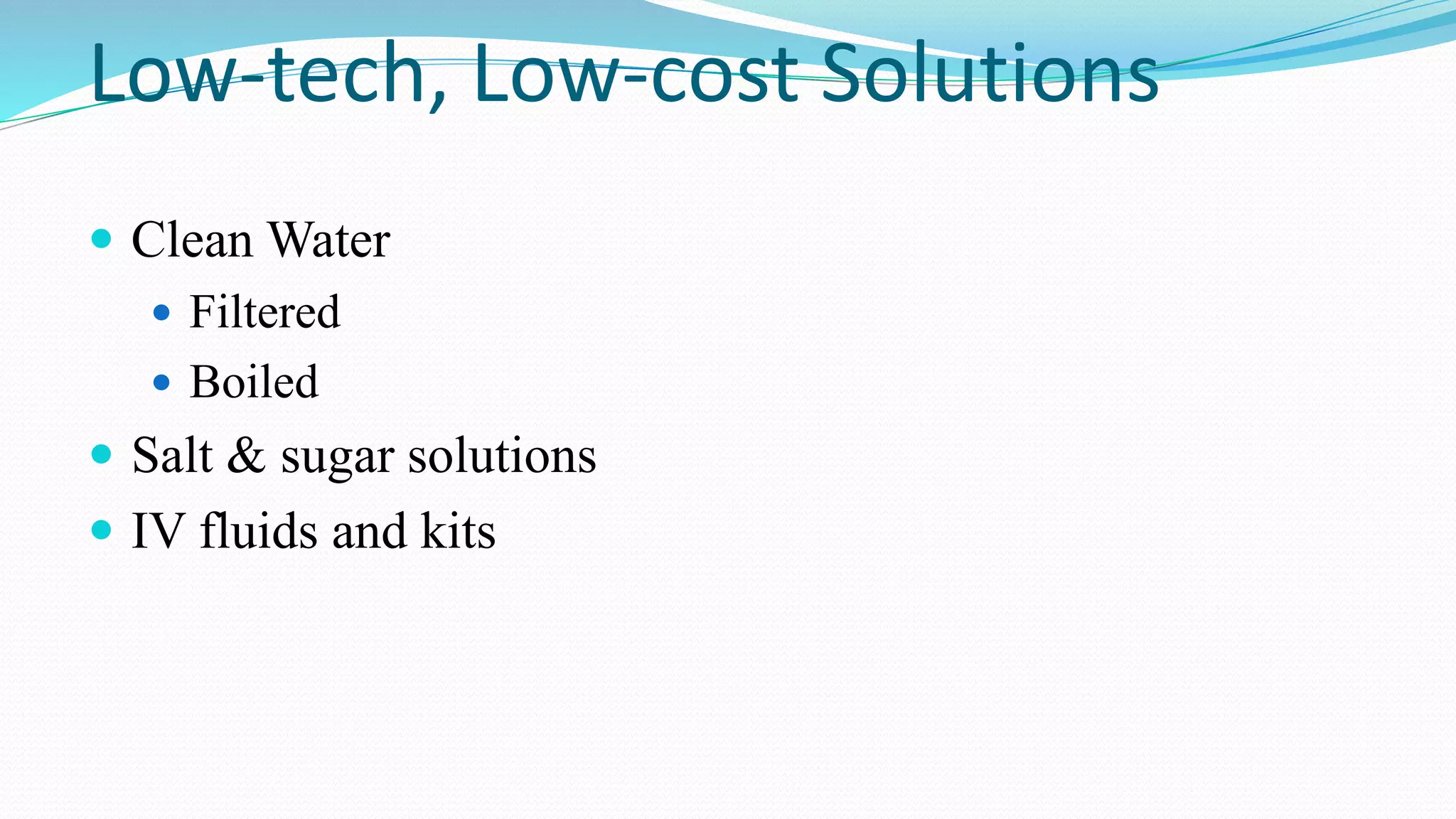
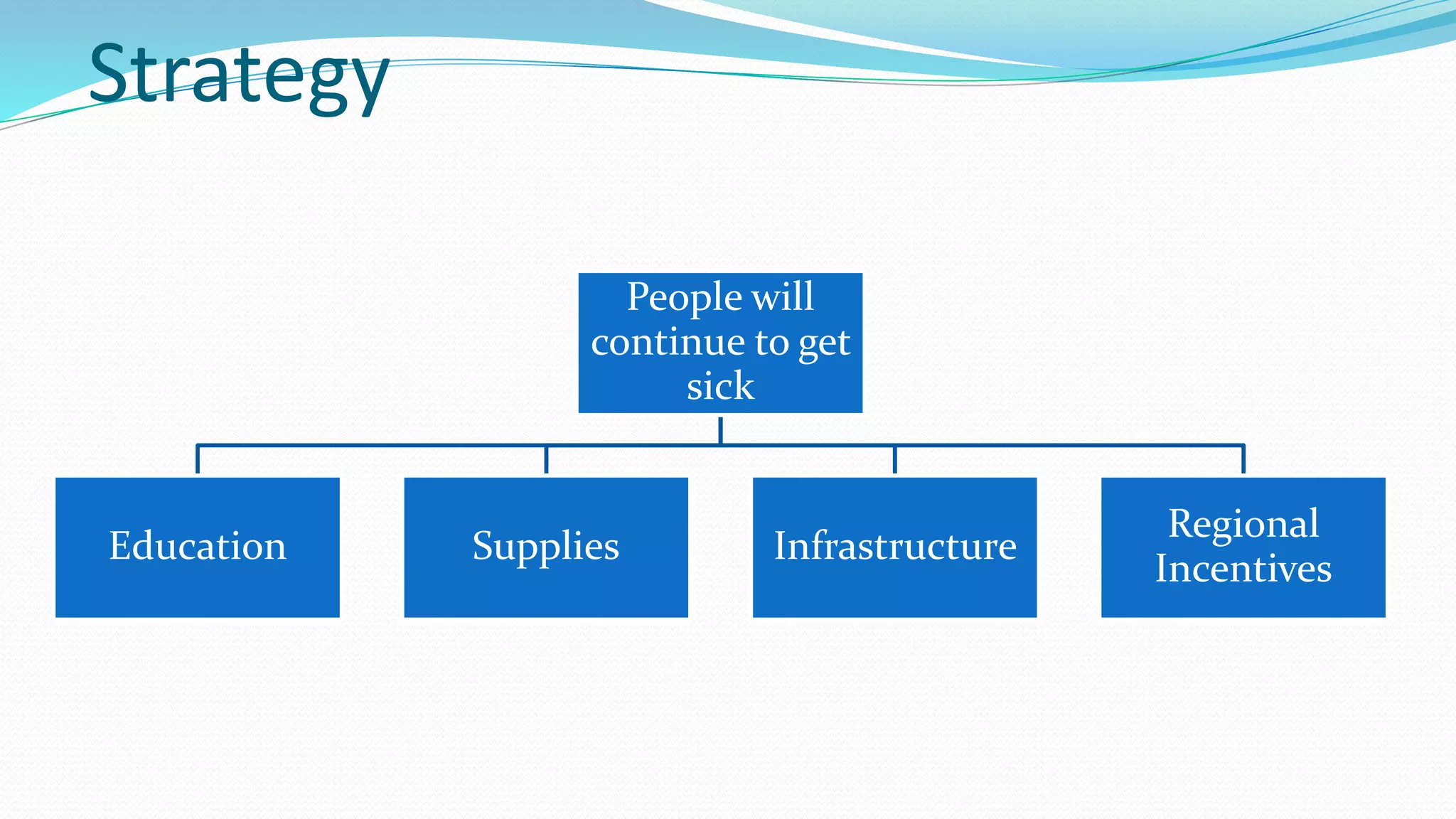
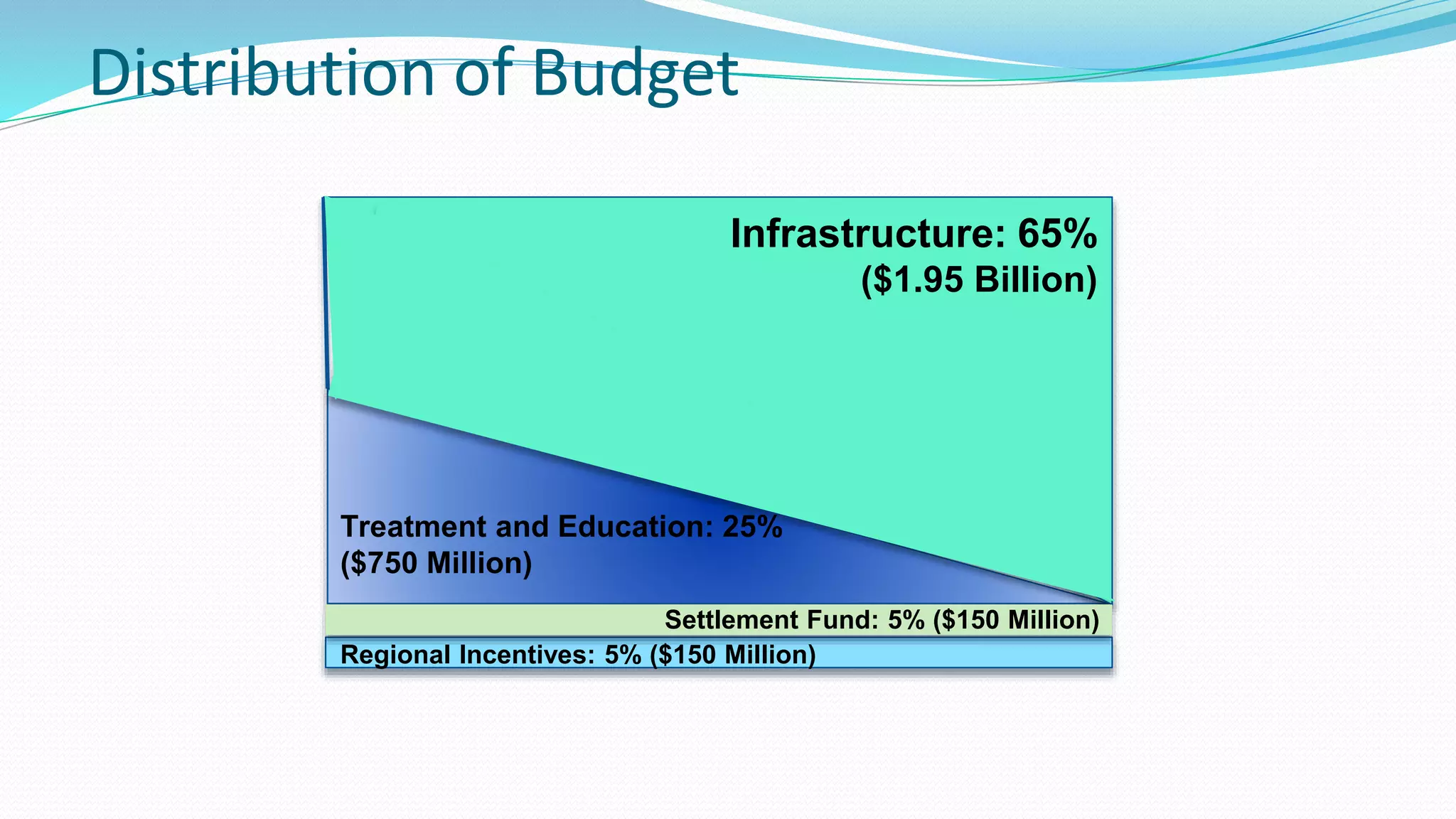
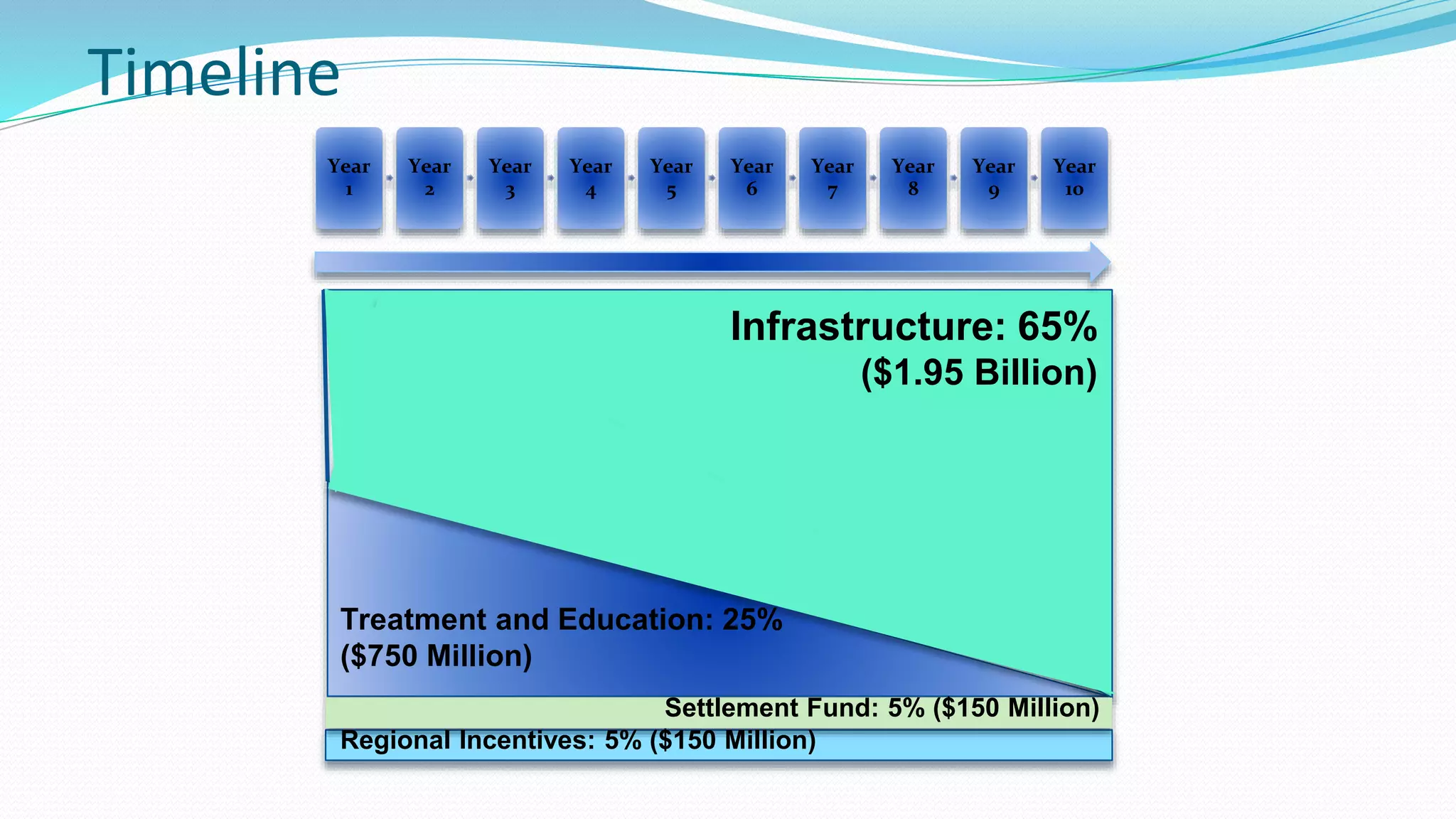
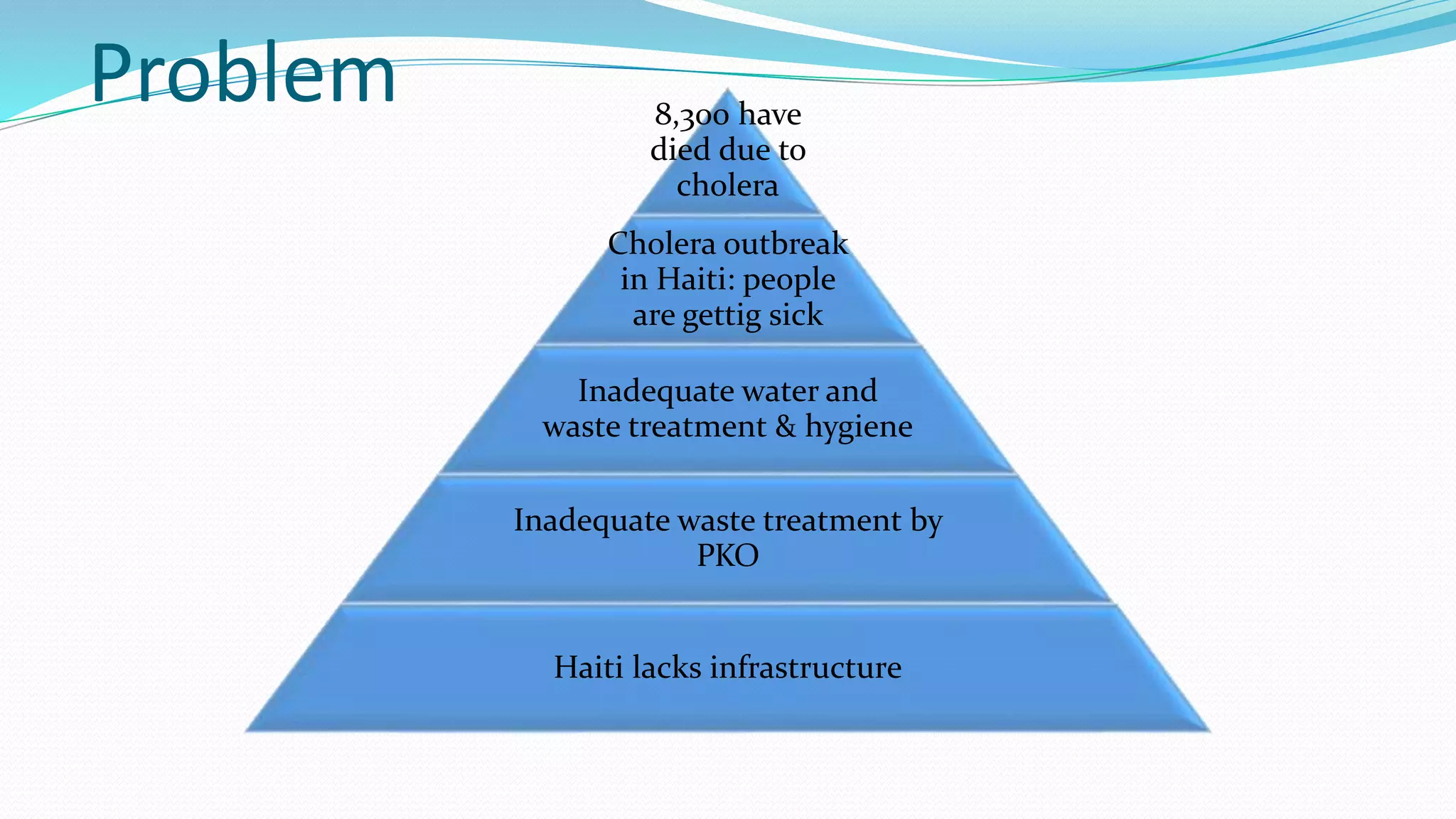
The document outlines a strategic plan to eliminate cholera in Haiti within 10 years. It proposes using funds for treatment, education, and long-term infrastructure development. Key aspects include settling UN claims, improving waste treatment, increasing access to clean water and healthcare, and coordinating with neighboring countries. The goal is to end deaths from cholera and prevent future outbreaks through sustainable solutions.


![Solutions
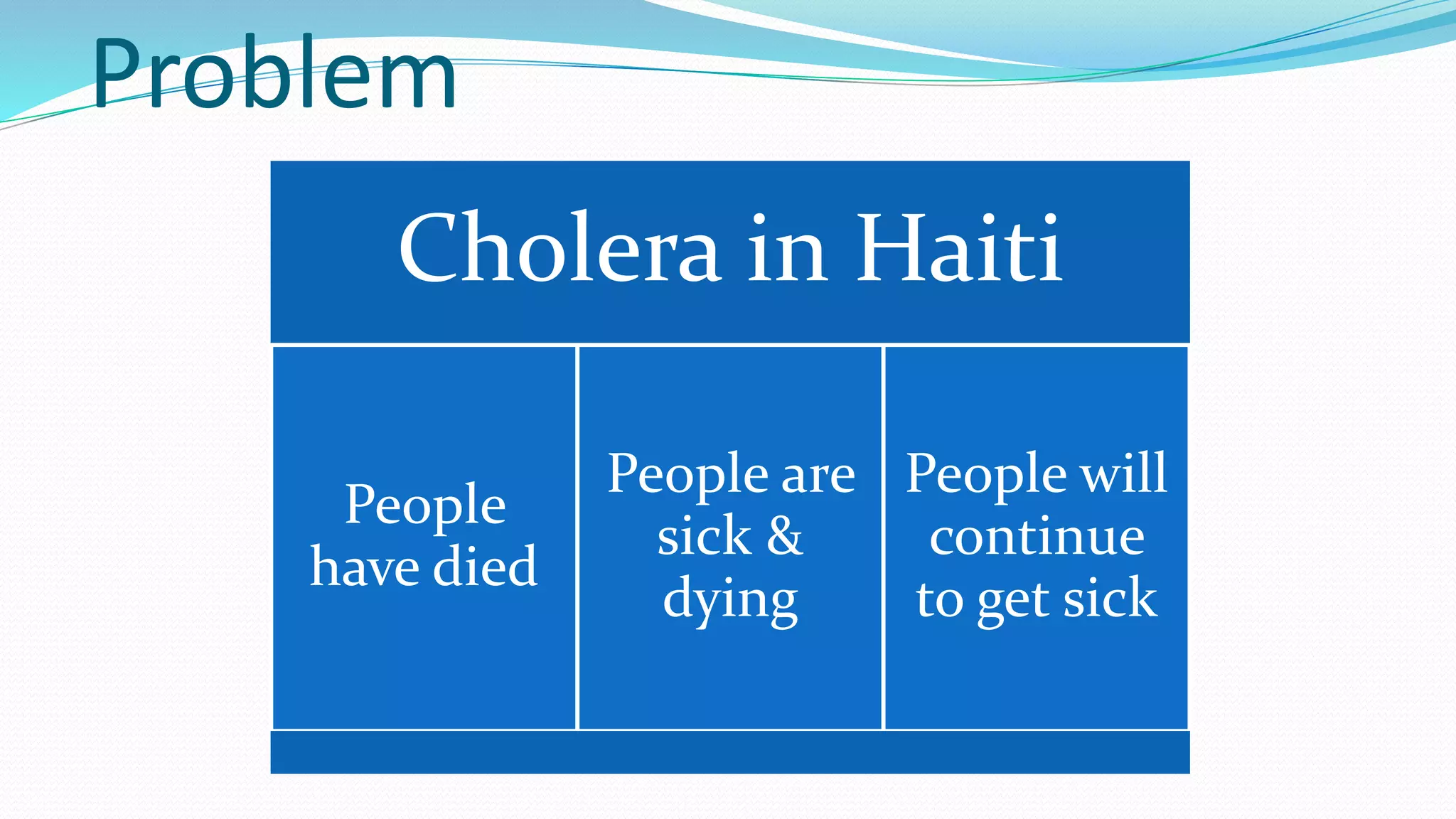
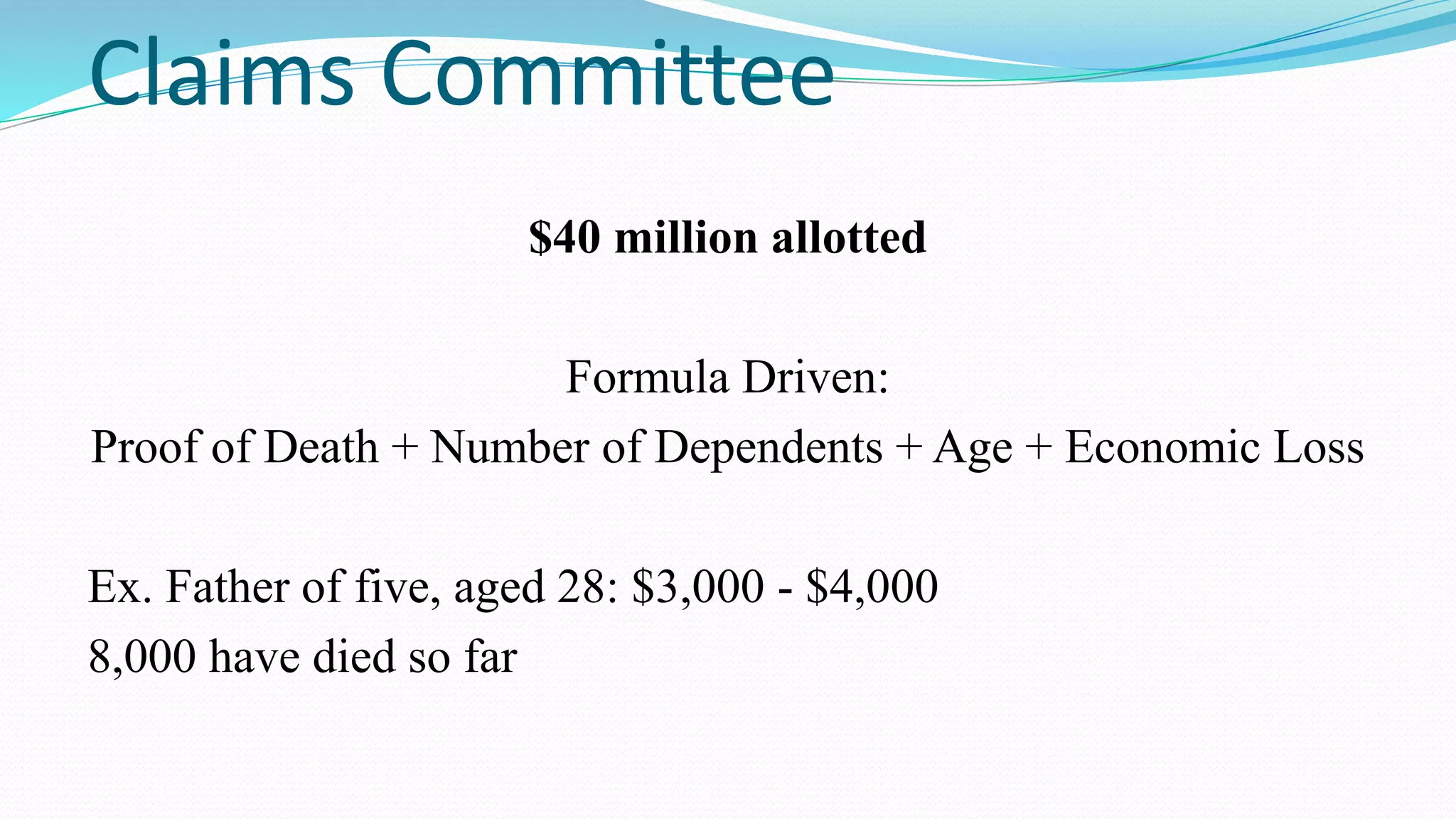
8,300 Haitians who died as a result of the cholera epidemic as well as some 650,000
more survivors of the illness.
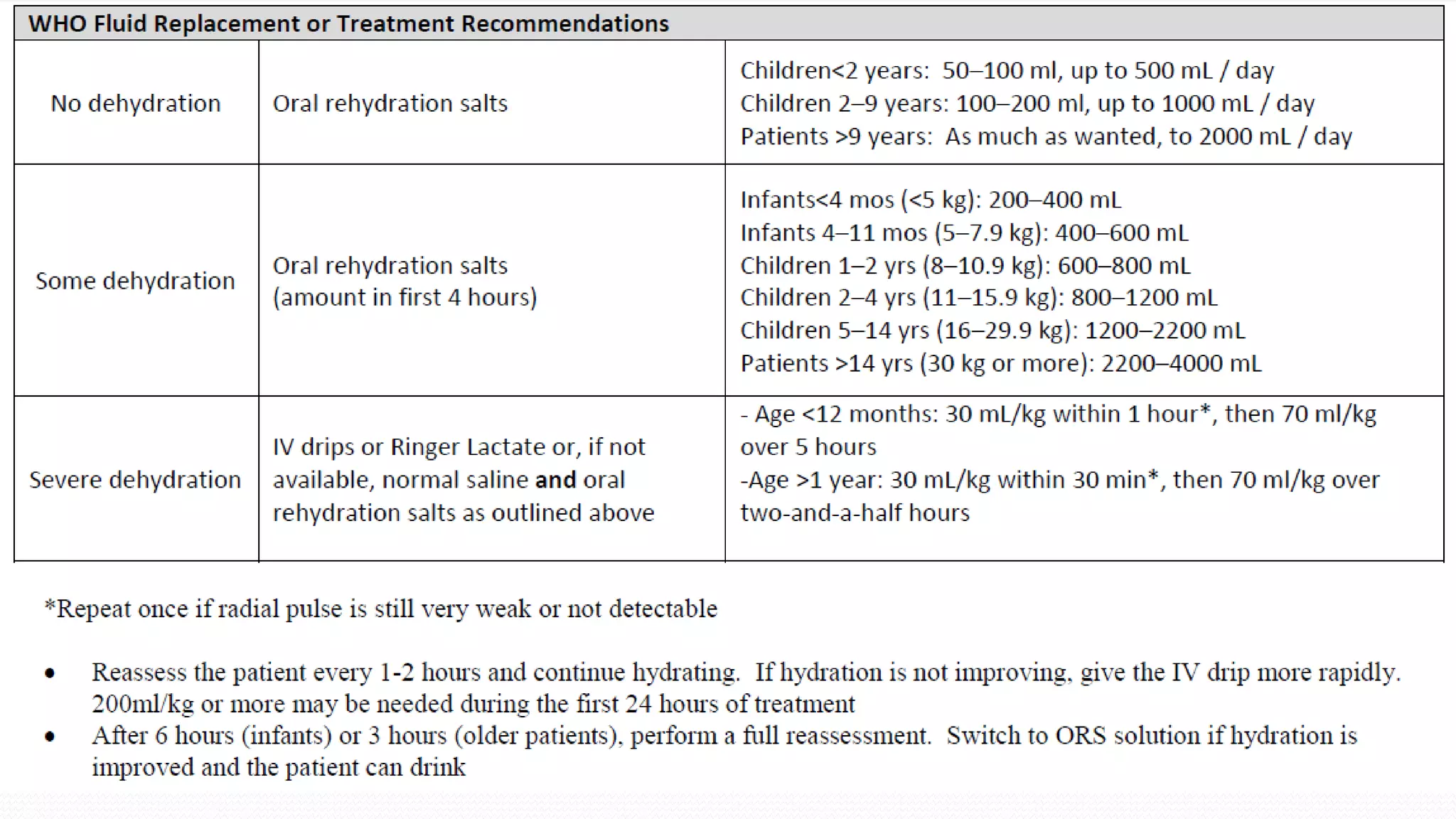
$2,220,000 ORS (.11cents per packet, 20 packets per person, 1,000,000 ppl)
$10,000,000 vaccine/yr (1.85 per vaccine, vaccines for 1,000,000)
$9,600 (.04per 200mg tablet)
$920,000 (7 per IV Ringer Lactate solution kit) *really 840,000 but a bit
more added just in case
[120,000 hospitalization per year]
$1,222,300,800 Full sanitation system (cost of treatment system for all of the domestic
water
$250,000 (300,000liters per day)
Hôpital Universitaire de Mirebalais (HUM) Mirebalais](https://image.slidesharecdn.com/team20-140217122615-phpapp01/75/Team-20-30-2048.jpg)