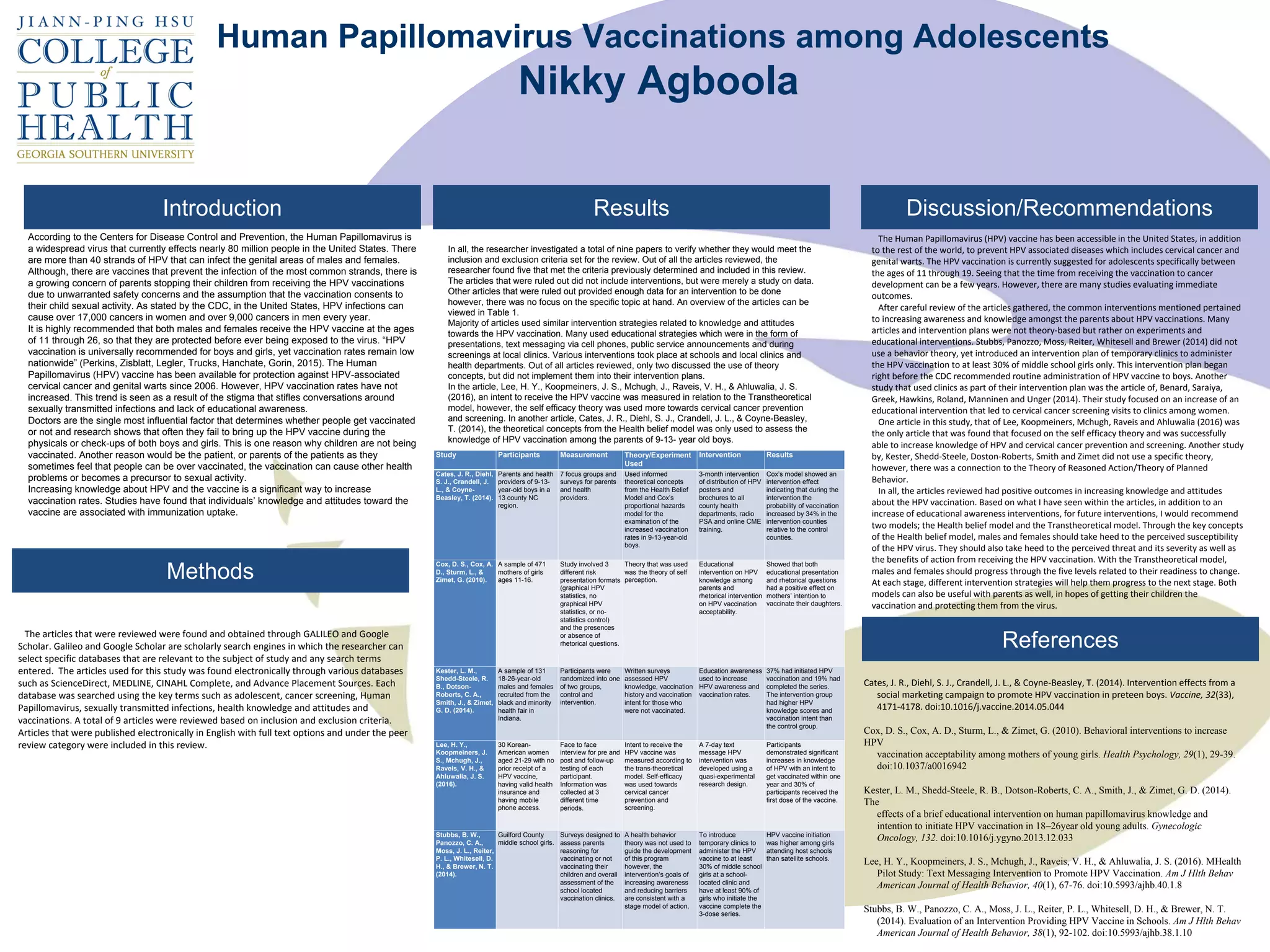
The document summarizes key findings from several studies on interventions to increase HPV vaccination rates. The studies commonly used educational interventions such as presentations and text messages to increase knowledge about HPV and the vaccine. While many interventions were not theory-based, one study found that a text message intervention grounded in the Transtheoretical Model successfully increased vaccination intent and rates. Overall, the reviewed studies found that educational awareness interventions generally improved knowledge and attitudes toward the HPV vaccine.