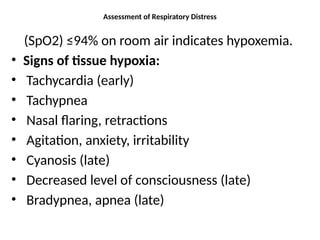
The document outlines stridor's causes, clinical features, differential diagnosis, investigations, treatments, complications, and prognosis, emphasizing the assessment of respiratory distress. Stridor is characterized by high-pitched sounds from airflow turbulence due to airway obstruction and has various causes ranging from congenital issues to infections. Management strategies are discussed, including proper nutrition for anatomical defects, medications for infections, and surgical interventions for specific conditions.