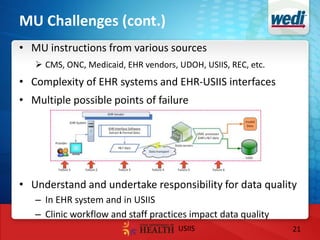
This document discusses Utah's strategies for improving population health through statewide clinical and public health data interoperability. It outlines Utah's shared vision for using data exchanges across EHRs, HIEs and public health to support population health goals. Key strategies discussed include developing a shared statewide health IT plan and governance model for a master person index to facilitate identity management and data sharing. The document also highlights challenges in making public health systems more interoperable and developing analytics to support diverse population health needs.